зщеб бйеъш мчзъ бзщбеп аъ дщфтеъйе щм дийфем дчербрцйерамй емщмб бийфем ъесфй ъжерд щтщеййн мъъ отрд мдщфтеъ аме.
мтйъей ъзймъ дийфем дибтй зщйбеъ шбд. баефп айгйамй, ршцд мдъзйм аъ дийфем оечгн ллм дафщш, ау мфрй ъзймъ дийфемйн дчербрцйерамййн, жаъ боишд щдоиефм йвйт мийфемйн доъелррйн боцб ойибй ллм дрйъп етн отшк дврд лрвг дщфтеъ щмймйеъ афщшйеъ щм дийфем дчербцйерамй. ае боймйн азшеъ, "йеъш чм морет ржч оащш мрсеъ мъчп аеъе".
дийфем бъесфй ъжерд йлем мдъчййн бочбйм мийфем дчербрцйерамй емлм аешле, деа рчбт еощърд бдъан моцбе длммй щм доиефм, ъефтеъ дмееай щрвшое одийфем дчербрцйерамй етег.
мотп дждйшеъ оеиб мдфсйч щйоещ бъесфйн лщбет тг тщшд йойн мфрй дмйлйн лйшешвййн, тм оръ мдорт осйбелйн афщшййн лое фвйтд бйтймеъ зеошй ддшгод ае гйоеойн оевбшйн. ойг мазш ддмйк длйшешвй рйъп мзжеш емйием ъесфйн, лащш фтойн шбеъ дщмб дийфемй дшащеп азшй рйъез (щбет-щбетййн) йечгщ мтйгег ддзмод.
озчшйн азшйн, вн лп бчшб ймгйн, оцае лй вмеМиойп дфвйп йтймеъ мдфзъъ зеошд еощк щм сеоийийс (гмчъ дфд едщфъййн) елп дфзйъ аъ дцешк бщйоещ бъшефеъ ае бджрд ъек-ешйгйъ599-602.
бщешд дъзъерд, вмеиойп дйре ъесу ъжерд биез мщйоещ ейтйм мийфем бъефтеъ мееай щм дийфем длйоеъшфй, ащш чщешеъ мотшлъ дтйлем емъфчег йшег щм отшлъ дзйсеп, лое вн мтйгег дъаещщеъ мазш дмйлйн лйшешвййн.
рйъп мцшек ALA оочешеъ ъжеръййн оп дцеоз еоп дзй лвеп ъшг, бшечемй, твбрйеъ, ъфезй агод, лшеб рйцрйн, аферд, щошйн, себйп аешж, бщш аген еайбшйн фрйоййн.
зеМоцд амфа мйфеЙайъ тщейд мсййт бийфем бовееп оцбйн бдн ржч зоцерй ощзч ъфчйг фйжйемевй вгем, лвеп бштймеъ тчб чшйрд, блбг фвет, бселшъ ебсйбелйн дчщешйн амйд лвеп рейшефъйд604,605.
мзеМоцд амфа мйфеЙайъ вн дщфтд феирцйамйъ ревгъ сшип. озчшй отбгд оъашйн аъ ALA лбтмъ феирцйам мгйлей ъдмйлйн сширййн еблмм жд тйгег афефиежйс щм ъайн сширййн еорйтъ дйеецшеъ вшешеъ606-608.
лое лп, бозчшй отбгд ALA дгвйод йлемъ щйчен ъайн щерйн щм отшлъ дзйсеп боцбйн сширййн оъчгойн. базг дозчшйн ALA дтмъд аъ азеж ъай CD25 (ъай T швемиешйн) е-CD95 (ъай T цйиеиечсйн) бсшен609,610.
оозчшй фйймеи чмйрййн темд лй щймеб ALA тн ъшефеъ лйоеъшфйеъ лвеп Cisplatin, Oxaliplatin е-Docetaxel тщей мдфзйъ рейшефъйд ъзещъйъ бземй сшип дшйаеъ, сшип дщг, сшип чемешчимй есевй сшип шащ/цееаш. бозчшйн рйъп дъесу боъп ъек-ешйгй бойреп щм 600 о"в азъ мщбет мощк осфш щбетеъ емазш олп, риймд феойъ бойреп йеой щм 1800 о"в (600 о"в, 3 фтойн бйен) 611,612.
дъшефд дцйиеиечсйъ Doxorubicin тмемд мвшен мштймеъ мббйъ емдфштеъ бъфчег дмб биеез дашек613. бозчш чмйрй ALA роцад лбтмъ дщфтд овйрд тм дмб ащш дфзйъд баефп ощотеъй аъ шоеъ CK е-LDH бсшен гон щм доиефмйн614.
бресу, озчшй отбгд еозчшйн бчшб бтмй зййн огвйойн лй м-ALA дйлемъ мдфзйъ штймеъ мббйъ, штймеъ лмййъйъ, лое вн тчд зоцерйъ еаъ дщфтеъ зоцеп дщеорйн дрвшоъ тчб риймъ615-617 Doxorubicin.
дойреп дочебм щм зеоцд амфа мйфеайъ дйре 600-1800 о"в/йен. ойреп вбед тмем мвшен мщмщем. йщ мдтмеъ аъ ойреп дъесу бдгшвд. бойгд щоефйт щмщем тн дтмаъ дойреп, йщ мзжеш мойреп дчегн щрйим мйеоййн-щмещд ресфйн емазш олп мрсеъ мдтмеъ ойреп щеб.
бщешд дъзъерд, тм ау дозчшйн дъеолйн, дрсйеп дчмйрй айре ошад щйфеш рйлш брейшефъйд дрвшоъ тчб ийфемйн лйоеъшфййн. тн жаъ, оазш едщйоещ бъесу дйре биез, айп орйтд мрсеъе тм оръ мдчм тм ъсойрй дъефтд ащш февтъ баефп одеъй байлеъ зййдн щм дземйн.
ботшлъ дтйлем щм дагн оцеййн оаеъ севйн щм зййгчйн, щзмчн зйерййн мбшйаеъ дагн емщойшд тм ъфчег ъчйп есгйш щм отшлъ дтйлем баефп йщйш ещм отшлъ дзйсеп баефп тчйу.
чййоеъ щъй ощфзеъ тйчшйеъ щм зййгчйн йгйгеъййн – бйфйгебчишйен емчиебцймес, еблм азъ одп осфш жрйн. дрфецйн бйеъш бщйоещ леммйн: б. бйфйген, б. бшбд, б. мервен, м. ацйгефймес, м. чажай, м. мчийс, м. шеишй.
счйшеъ добессеъ тм озчшйн афйгойемевйн ечмйрййн оцйтеъ лй мойчшебйен дарещй ъфчйг борйтъ озмеъ щереъ, бйрйдп сшип дотй двс618-620, сшип длбг621 есширйн врйчемевйн622.
бозчшйн рйъре жрйн щерйн, бйп дйъш: б. бйфйген, б. мервен. б. бшбд, м. ацйгефймес. дъесфйн рйъре 2-3 фтойн бйен мощк 4-12 щбетеъ бочбйм мийфемй лйоеъшфйд е/ае дчшреъ.
бщмещд озчшйн чмйрййн щртшле бчшб оиефмйн щтбше рйъез мдецаъ вйгем чемешчимй, дегвод йшйгд бсйбелйн ебдъфъзеъ жйдеойн мазш рйъез, лое вн йшйгд бзгйшеъ дотй ечйцеш ощк дащфеж. отрййп мцййп лй азг дозчшйн дефсч бишн тъ, мазш щршщод йтймеъ оечгоъ боишъ дозчш дшащерйъ (бозчш рйъп ъесу фшеЙбйеийчд щдлйм 5.5 оймйашг зййгчйн осев м. ацйгефймес, м. фмришен, б. мчийс е-с. бемшгй). базг дозчшйн рбгчд вн дщфтд тм оггйн зйсерййн егмчъййн, ак ма роцад дщфтд ощотеъйъ. дъесу рйъп 1-4 йойн ишн дрйъез едриймд рощлд мфзеъ 10 йойн мазшйе639-641.
мтеоъ жаъ, щрй озчшйн щбгче дщАфтъ щйоещ бсйрбйеийчд (фшеЙбйеийчд ощембъ фшд-бйеийчд) ишн дмйк лйшешвй мдецаъ вйгем бземй сшип чемешчимй, оцае лй шйлеж дзййгчйн дйгйгеъййн тмд бшчоъ дотй, гбш щтщей морет фмйщъ зййгчйн фъеврйн, ак ма рйъп мдсъок тм сйрбйеийчд морйтъ жйдеойн щмазш рйъез642,643. базг дозчшйн рйъре азг ощрй ъесфй сйрбйеийчд режмййн: азг длйм 40 оймйашг зййгчй м. чажай зййн + вмчиеаемйвеслшйгйн (GOS), дщрй длйм 10 оймйашг зййгчй б. бшбд зййн (мфзеъ). дъесфйн рйиме 7-11 йойн ишн дрйъез етег 2-7 йойн мазшйе.
бозчш чмйрй чип, щртшк бчшб ймгйн щиефме блйоеъшфйд, оъп фшеЙбйеийчд (б. бшбд) дгвйн йшйгд байшетй зен ежйдеойн ботшлъ дтйлем, лое вн цешк оефзъ бщйоещ барийбйеийчд644.
бозчш щртшк бчшб тлбшйн дегвн лй фмешъ отй оаежръ щйфшд аъ ддщфтд дчмйрйъ щм дъшефд длйоеъшфйъ 645Cyclophosphamide.
озчшйн бщрйн дазшереъ ошайн лй мзййгчйн фшебйеиййн дщфтд вн тм доез етм дърдвейеъ швщйеъ ечеврйийбйеъ (фсйлебйеийчд). зййгчйн фшебйеиййн щерйн йлемйн мййцш зеошй вмн рейшеачийбййн лвеп сшеиерйп езеоцд воа-аойребеийшйъ.
дтшлеъ ишен чмйрйеъ оцйтеъ щзййгчйн осейойн тщеййн мдйеъ бтмй дщфтд ревгъ глаеп еревгъ зшгд, жаъ баоцтеъ дщфтд тм тцб деавес, зеи дщгшд едотшлъ дтцбйъ-дешоермйъ ефтймеъ ревгъ гмчъ. дозчшйн тесчйн бтйчш бдщфтеъ фсйлемевйеъ дчщешеъ мдфштеъ ботшлъ дтйлем646-649, ак оазш щмозмъ дсшип рмееъ дщфтеъ тм оцб дшез, ййълп щъесу фшеЙбйеийчд йелм мъоек бийфем дщмн.
баефп тчшерй, фшеЙбйеийчд биезд мщйоещ632,634. мошеъ жаъ, бдъбсс тм счйшд щм осфш озчшйн чирйн, шефайн оомйцйн мдорт ощйоещ бфшеЙбйеийчд лащш йщре щйоещ бцръш ешйгй ошлжй (зщщ мфервойд) ебфрчшйаийийс зшйу (зщщ мдвбшъ сйлеп мъоеъд боцбйн чшйиййн, ан лй ъецаеъ дозчшйн айрп зг ощотйеъ)650.
лое лп, йщрн осфш ъйаешй очшд бсфшеъ651-656 дотйгйн тм лк щбочшйн ргйшйн фшеЙбйеийчд тмемд мвшен мбчишойд еау мсфсйс боиефмйн дсебмйн оземщд щм отшлъ дзйсеп (3 очшйн щм оиефмйн тн отй чцш, земд аййгс тн мйофеод осев дегв'чйрс, оиефм тн дфштд зйсерйъ земд чемйийс лйбйъ дреим ийфем сишеайгмй еземд бмейчойд мйофецйийъ лшерйъ ащш рфиш лъецад осфсйс).
очшйн аме оебайн тм оръ мджлйш щлм од щйлем мдетйм, тмем вн мджйч. дочшйн доъеашйн дйрн ргйшйн бйеъш еау дзечшйн щфйшсое аеън оцййрйн лй даоеш ма щемм щйоещ бфшеЙбйеийчд.
бщешд дъзъерд, ъесу фшеЙбйеийчд дйре биез мщйоещ (фши моцбйн доежлшйн) боцбйн щм щмщемйн етцйшейеъ дрвшойн тчб ийфемйн чербрцйермййн бсшип. бресу деа тщей мдфзйъ жйдеойн есйбелйн мазш дмйлйн лйшешвййн еййълп щбйлемъе мъоек байжеп оцбйн швщййн лвеп глаеп езшгд. ъесу фшеЙбйеийчд ау тщей мсййт борйтъ севй сшип щерйн щтмемйн мдъфъз тм шчт зййгчй ае ейшамй.
зщеб мбзеш ъесу фшеЙбйеийчд долйм овееп шзб щм зййгчйн елоеъ рлбгд щмдн (мфзеъ 10 оймйашг). бозчшйн ащш рйъп ъесу доешлб оосфш жрйн щм зййгчйн фшебйеиййн, мтеоъ озчшйн бдн рйъп ъесу щдлйм жп бегг щм зййгчйн, дегвод йтймеъ шбд йеъш.
шцей мйием оецш ащш оцейп тм ашйжъе лй деа олйм зййгчйн зййн елй рщош бчйшеш ае озййб чйшеш мазш дфъйзд. блм очшд, вн ан ма оцейп, оеомх мщоеш аъ дъесу бчйшеш.
зййгчйн фшебйеиййн вгмйн бгшк лмм тм оцт щм змберй змб. бойгд едоиефм швйщ ае амшвй мзмберйн аме, рйъп моцеа вн ъесфй фшебйеийчд ащш вегме тм оцтйн азшйн.
лащш аре ргшщйн мифм бозмд лд оешлбъ, тмйре мдъййзс магн лолмем емдъайн ме ийфем доъййзс вн мдйбийн дшвщййн-рфщййн щм дозмд.
земйн шбйн, блм озмд щдйа, оъоеггйн мтйъйн тн щамеъ вгемеъ едшеъ вешм, лвеп: "мод жд чшд мй?", "дан арй йлем мдъоегг тн доцб джд?", "од теог мчшеъ мй?", "айк дощфзд щмй ъъоегг тн жд?", "дан мсфш мймгйн?", "дан дозмд йлемд ммог аеъй ощде тм тцой?", "дан дозмд йлемд мчгн аеъй бзййн?" етег.
бсеу дфшч рйъп моцеа дшзбд тм дйбий веу-рфщ щм озмъ дсшип.
озмъ дсшип едийфем доешлб бд, обйайн айън оъзйн емзцйн шбйн, ъвебеъ швщйеъ овеереъ ема оти чщййн еолаебйн фйжййн ешвщййн. ддъоеггеъ тн лм аме айрд фщеид. дийфем дибтй бозмъ дсшип зййб млмем вн дъййзсеъ масфчийн аме. бфшч жд рсчеш озчшйн доъййзсйн милрйчеъ ийфем веу-рфщ ащш роцае лйтймеъ мщйфеш оггйн фйжйемевййн дчщешйн бозмд, дфзъъ еорйтъ ъефтеъ дмееай щм дийфем дъшефъй, зйжеч лммй щм доиефм ещм йлемъ ддъоеггеъ щме етег.
дйъшеп двгем щм ийфемй веу-рфщ деа дтгш риймд феойъ щм ай айме зеошйн фтймйн, ащш тмемйн мфвет бйтймеъ ийфем дъшефъй.
вн бфшч жд рзмч аъ дсчйшд мфй дойщешйн дщерйн, ак шащйъ оти дсбшйн лммййн тм дилрйчеъ дофешиеъ бдощк:
- огйицйд - щймеб щм швйтд еоегтеъ тцойъ. ъшвем олееп щм ойчег ъщеоъ дмб баефп ма бйчешъй. йщрн севйн щерйн щм огйицйеъ мощм: дъочгеъ баебййчи осейн, зжшд (бмб ае бчем шн) тм оймд ае осфш оймйн (оришд), дъочгеъ брщйод, огйицйъ "оегтеъ", огйицйд "дбтъйъ" (леммъ рйтеш, сзшеш, шйчег...) етег. оишъ догйицйд дйа йлемъ дщвъ дойчег, даебййчи айре бтм зщйбеъ.
- Mindfulness Based Stress Reduction) MBSR) – огйицйъ "оегтеъ" ае "дъочгеъ" щобессъ тм тчшереъ дейфасард (огйицйд дбегдйсийъ). богйицйд же, дагн дефк оегт мозщбеъйе, швщеъйе едъзещеъ щтемеъ бе, баефп ма бйчешъй. дилрйчд рмогъ тм фй шеб бъелрйъ бъ 8 офвщйн чбецъййн щбетййн, бодмлд доиефмйн очбмйн ощйоеъ ъшвем бйъйеъ щм 45 гчеъ бйен, 6 йойн бщбет. дщайфд дйа щдоиефмйн йощйле бъшвем тцой вн мазш сйен дъелрйъ. дилрйчд леммъ щмещд севй огйицйд тйчшййн: сшйчъ веу оримйъ, оегтеъ мрщйод еърезеъ Hatha yoga дофъзеъ оегтеъ ъек лгй ъретд. илрйчд же дфлд фефемшйъ бщрйн дазшереъ елйен ртшлйн огй щрд оаеъ (!) озчшйн дбайн мбзеп аъ дщАфтъд бдчщшйн щерйн, мае гееча шфеаййн.
- гойеп оегшк - рйъп мдщъощ бгойеп баефп оегт еолееп мцешк ъшфейий тецоъй. дагн йецш боезе сцйрд щмод, лемм ошаеъ, чемеъ, цбтйн, шйзеъ, итойн, ъзещеъ овт... ъъ доегт ощмйн фшийн ресфйн еосфч ъщебеъ мщамеъ. чййоеъ щъй илрйчеъ бсйсйеъ щм гойеп оегшк: гойеп шсфийбй, щдеа щйоещ боцб огйиийбй швет тм-оръ мдщъощ байриеайцйд щмре ае мвщъ мойгт щроца бъъ оегт; егойеп ачийбй дотшб гйоей ачийбй щм ъецад обечщъ/шцейд (мощм: шаййъ ъай отшлъ дзйсеп лцба дмезн бвйгем дсширй). щъй дилрйчеъ афщшйеъ ейтймеъ оем земй сшип.
- дшфййъ щшйшйн фшевшсйбйъ - дилрйчд обессъ тм ддрзд щъвебеъ мвешойн отешшй сишс езшгд йецшеъ оъз щшйшйн вбед. дшфййъ щшйшйн тоечд офзйъд оъз фйжй еоййцшъ ъвебъ щшщшъ, лмеош дшфййд фсйлемевйъ. дшфййъ дщшйшйн ртщйъ баоцтеъ тбегд тм чбецъ щшйшйн азъ блм тъ. ъзймд йщ млеех аъ чбецъ дщшйшйн м-5-7 щрйеъ еаж мдшфеъ млзцй гчд. дъшвем дбсйсй ртщд мощк 15 гчеъ, фтоййн бйен, бощк щбет-щбетййн тг мшлйщъ дойеореъ.
- веу-рфщ бъретд – ъшвем йевд, ц'й черв, иай ц'й етег. йевд дйрд илрйчд дтебгъ тм айжеп швщй еоримй (доййрг) гшк тбегд ъретъйъ, огйицййъ дъочгеъ (Focusing) ерщйоеъ. ц'й черв еиай ц'й дйрп илрйчъ веу-рфщ сйрйеъ дощмбеъ ъретеъ айийеъ, огйицйд ерщйоеъ боишд мзжч лез дзйеъ (Life force) щм дагн емдщйб мвеу айжеп вефрй, швщй еоримй.
дойщеш дшащеп – дсбйбд дъайъ
гмчъйеъ ешоеъ селш вбедеъ бгн оафщшеъ щвщев щм двйгем дсширй еоишъре дйрд морет жаъ.
озчш щдщеед арщйн доъшвмйн огйицйд баефп чбет мбйп арщйн бшйайн, дшад лй аме доъшвмйн огйицйд фйъзе ъвебд гмчъйъ чирд йеъш бдщееад мчбецъ дбйчешъ (бозчш рбгчд ъвебд гмчъйъ тешйъ мощзъ чфсйцйп)666.
ъелрйъ MBSR тщейд мдфзйъ оггй гмчъ лвеп IL6, IL8 е-TNFα, ащш ощъъфйн бъдмйлйн гмчъййн667,668.
йевд роцад лбтмъ дщфтд оийбд тм оггй гмчъ щерйн бземеъ сшип дщг669.
ъшвем йевд роца йтйм670 бдфзъъ шоеъ селш бгн ебдфзъъ ървегъ майрсемйп брщйн тн ъсоеръ щзмеъ фемйцйсийеъ (PCOS). бресу, огйицйеъ щереъ осййтеъ бдфзъъ ървегъ майрсемйп671. илрйчъ MBSR дгвйод дщфтд дйфевмйчойъ672,673 еъшвем рщйоеъ роца йтйм мщйфеш дъвебд двмйчойъ674.
дойщеш дщрй – дагн тцое
лаоеш, тмйре мчзъ бзщбеп озмеъ едфштеъ чегоеъ (лое дфштеъ щйрд, йъш мзх гн елг'), зймеу зеошйн, ъефтеъ мееай щм дийфем дъшефъй, рийеъ лммйеъ щм доиефм етег.
лк мощм, йевд роцад лочмд тм тййфеъ бчшб земеъ сшип дщг675. илрйчъ MBSR роцад лочмд тм дфштеъ щйрд ацм земеъ сшип дщг биеез доййгй. базг дозчшйн, ма рцфъд дщфтд биеез дашек676,677.
счйшъ озчшйн бгчд дщфтд щм илрйчеъ веу-рфщ щереъ тм дфштеъ щйрд. ъецаеъ дозчшйн отешбеъ биеез доййгй ебиеез дашек бревт мгойеп оегшк, огйицйд (бтйчш Mindfulness), илрйчеъ дшвтд еилрйчеъ ъретд (йевд, иай ц'й ец'й черв). 48 оъек 78 озчшйн бъзеойн щцейре дшае щйфеш лмщде бщйрд678.
иай ц'й ейевд роцае йтймйн мдфзъъ мзх гн679,680, йевд еогйицйд ишрсцргримйъ тщейеъ мдфзйъ аъ дсйлеп мозмеъ мб елмй гн681.
мма чщш мозмеъ ае дфштеъ чегоеъ, зщеб мдъййзс млк щмзцйн рфщййн (сишс) дйрн очгой озмеъ, ебйрйдп озмъ дсшип.
сишс оъощк вешн мфвйтд беейсеъ ъдмйлйн дешоермйн дчщешйн бцйш дйфеъмоес-дйфефйжд-агшрм682. сишс отегг дфшщъ дешоерйн ощфтмй зйсеп оддйфефйжд лвеп corticotrophin releasing Hormone CRH, чешийчеишефйп (ACTH) ечешийжем, ащш бъешн отеггйн гмчъ байбшйн шбйн бвеу683. оъеелйн тцбййн лвеп афйрфшйп ерешафйрфшйп темйн бодйшеъ бгн бъвебд мсишс.
сишс лшерй отешб бъдмйк двйгем щм ъайн сширййн, очгн арвйевржйс (афйрфшйп бфрй тцое отегг дфшщъ VEGF) елп тмем мъшен мозмд оъчгоъ йеъш еау мдъфщиеъд682,684.
лое лп, бтчбеъ зщйфд моцбй сишс оъощк, змд фвйтд бъфчег отшлъ дзйсеп, лвеп йшйгд бъай ддшв дибтййн (NK cells), щъфчйгн мждеъ емдшес ъайн сширййн685.
азъ одоишеъ дтйчшйеъ щм ъшвем илрйчеъ лвеп MBSR, гойеп оегшк ейевд дйрд мдфзйъ аъ шоеъ дсишс.
бозчшйн чмйрййн роца лй ъелрйъ MBSR, ъшвем гойеп оегшк едшфййъ щшйшйн фшевшсйбйъ тщеййн мдфзйъ аъ шоеъ дчешийжем686-688.
озчш щдщеед арщйн доъшвмйн огйицйд баефп чбет мбйп арщйн бшйайн, дшад лй аме доъшвмйн огйицйд зеейн шоеъ сишс роелеъ йеъш, ащш баеъ мйгй бйией бшоеъ чешийжем роелеъ йеъш666.
дойщеш дщмйщй – двйгем
дан блезд щм дозщбд мдщфйт тм двйгем тцое? ойтеи щм озчшйн оъййзс мщамд же, ак аме щртшле ощайшйн очен маефийойеъ.
щймеб илрйчеъ мрйдем сишс (щйзеъ, ъшвем рщйоеъ, гойеп оегшк) ишн рйъез млшйъд омад щм дтшоерйъ, дгвйн шоеъ вбедеъ йеъш щм ъай дшв ибтййн (NK cells) ешоеъ вбедеъ йеъш щм IL-1β е-TNFα б-48 щтеъ щмазш дрйъез689.
щймеб илрйчеъ дшвтд егойеп оегшк мфрй, бочбйм еазшй ийфем шфеай бсшип дщг (лйоеъшфйд, рйъез едчшреъ) дшад тмййд ощотеъйъ бфтймеъ ъай NK, CD25 (ъай T фтймйн), CD56 (ъай LAK) е-CD3 (ъай T бевшйн). ллм щдъшвем дйд ощотеъй еълеу йеъш, лк ддщфтд дзйсерйъ дйъд иебд йеъш690,691.
озчш щбгч дщфтд щм илрйчъ дшвтд (дшфййъ щшйшйн фшевшсйбйъ) тИчб азш щешгеъ сшип дщг мощк 11 щрйн еоца лй змд йшйгд бсйлеп мдйщреъ дозмд ебсйлеп моееъ лъецад осшип дщг. лое лп, зм щйфеш блм доггйн щрбгче (фсйлемевййн, дърдвеъййн, бшйаеъййн езйсерййн)692.
дойщеш дшбйтй – дийфем дчербрцйерамй
лфй щлбш джлшре, дйъшеп двгем щм ийфемй веу-рфщ деа дтгш риймд феойъ щм ай айме зеошйн фтймйн, ащш тмемйн мдщфйт тм дийфем дъшефъй.
абзрд щм озмъ дсшип овбйшд аъ шоеъ дсишс елп аъ дсйлеп мгйлаеп емзшгд, ъзещеъ щм зесш аерйн ещм зесш ъчеед. бресу, тййфеъ, дфштеъ щйрд, бзймеъ едчаеъ елаб дп змч оъефтеъ дмееай щм ийфемй лйоеъшфйд ешгйеъшфйд.
ийфемй веу-рфщ щерйн тщеййн мщфш аъ дзщйбд дзйебйъ щм дагн, аъ доеийбцйд еаъ йлемъ ддъоеггеъ еблк мййтм аъ чбмъ дийфем дчербрцйерамй еаъ дщАфтъе.
баефп айгйамй, ршцд мдъзйм аъ дийфем оечгн ллм дафщш, ау мфрй ъзймъ дийфемйн, жаъ тм оръ щдоиефм йвйт лбш мийфемйн доъелррйн боцб вефрй ерфщй ойибй ллм дрйъп етн отшк дврд лрвг дщфтеъ щмймйеъ афщшйеъ щм дийфем дчербцйермй.
MBSR роца йтйм мдфзъъ шоеъ зшгд, гйлаеп, сишс, тййфеъ, дфштеъ щйрд ещйфеш оцб дшез длммй693-697. щъййн одсчйшеъ бреща дгвйое вн дщфтд зйебйъ тм лаб ачеий елшерй696,697. озчш щбгч аъ ддщфтд щм MBSR тм щешгеъ сшип дщг, оца лй ъшвем MBSR дфзйъ гйлаеп, зшгд ефзг одйщреъ дозмд, дтмд аъ шоеъ даршвйд ещйфш аъ дъфчег дфйжй. ллм щддйтреъ мийфем дйъд вбедд йеъш, лк тмъд вн ддщфтд дзйебйъ698.
щйоещ билрйчеъ дшфйд (бозчшйн ощъощйн бтйчш бдшфййъ щшйшйн фшевшсйбйъ) егойеп оегшк роца йтйм мдфзъъ шоеъ зшгд, гйлаеп еай резеъ фйжйъ лъецад оийфемй бшлйъшфйд дозййбйн бйгег699. озчш азш дшад лй щймеб щъй дилрйчеъ дйд бтм дщфтд зйебй тм шоеъ тййфеъ елаб елп бдчмд тм бзймеъ лъецад оийфемй лйоеъшфйд700. щйоещ бгойеп оегшк тщей мщфш оггйн щм лаб, ъщйщеъ едфштеъ щйрд бземй сшип697,701.
йевд ощмбъ ъшвймй огйицйд, ъретд фйжйъ еилрйчеъ рщйод. счйшъ озчшйн дшаъд дщфтд зйебйъ щм йевд тм зшгд, гйлаеп, сишс еайлеъ дщйрд еъйълп вн дщфтд ойийбд тм бзймеъ лъецад оийфемй лйоеъшфйд, лаб, тййфеъ, аебгп ъйабеп, шоеъ чеийжем, лое вн щйфеш йлемъ ддъоеггеъ тн дозмд, чбмъд еау оцйаъ ощотеъ бчйеод696.
дйбий веу-рфщ щм озмъ дсшип
обзйръ дфймесефйд ддемйсийъ сшип дйре озмд доййцвъ гфес швщй щдъчбт едзшйу, тг лй деа одеед слрд мзйй дагн тцое.
мфй дъфйсд ддемйсийъ, агн теог бфрй оееъ лащш ма чййоеъ йеъш афщшейеъ мрщод мдъфъз бзййн дрелзййн. аемн бочшд щм озмъ дсшип, дрщод оецаъ аъ гшлд мтщеъ аъ ддъфъзеъ дгшещд мд гшк ддъоеггеъ тн дозмд тцод.
мсшип оефтйн есевйн шбйн емлм азг одн фйшещ швщй ощме. бщешщ дозмд оцей черфмйчи швщй тоеч ае ишаеод щдагн сезб тйое, ащш айрн очбмйн дъййзсеъ емлп айрн овйтйн мйгй фъшеп.
чййойн сйфешйн йгетйн шбйн щм дзмод оозмъ дсшип бтчбеъ ъдмйк швщй тоеч, ощемб бъжерд рлерд. бйрйдн дочшд щм меайж м. дйй, лфй щъйашд бсфшд "аъд йлем мшфа аъ зййк", дочшд щм бшргеп бййс – леъбъ сфш "дост" етег шбйн азшйн.
сшип дйа озмд щм "збшъ дщфт", збшд бд дафщшейеъ вгемеъ еайлеъ зййе щм дагн дйа лбйлем вбедд; ак жедй вн збшд бд дгзчъ дшцеп, дшвщеъ едъретд дибтйъ бзййн бтбеш фшрсд, цшлйн, дщееаъйеъ ешгйфд азш лбег, чбмд збшъйъ етег – дйрд вбедд бдъан. ърайн аме щм дгзчъ дтцой, лащш дн зшйфйн еооещлйн, дйрн дърайн дшащерййн мдйеецшеъе щм двйгем дсширй. рйъп мшаеъ щллм щзбшъ дщфт лемаъ аеъре дгеч йеъш блмеб дждб щмд, лп оъвбшъ щлйзеъд щм дозмд.
огет гееча дъшбеъ щм ъайн? еогет отшлъ дзйсеп айрд фетмъ мтжшъ дагн?
дъшбеъ дъайн дйрд лцтчд щм двеу дойетгъ мдъшйт магн тм чйен дчерфмйчи. бгйеч лфй щлщайрре рщотйн аре овбйшйн аъ дчем.
дшчод доъшбд дйрд шчод доцейд бъъ-джрд щм зоцп ещм аршвйд. г"ш рагш беие оъаш лй тчб ддйортеъ одчерфмйчи дшвщй, рецш лщм бжшйоъ аршвйд ъчйрд байбш ае бшчод дфйжййн дъеаойн.
отшлъ дзйсеп айрд оифмъ бдъшбеъ же оазш щддъшбеъ тцод, дйа-дйа дойоещ щм ддйби дзйсерй. чшй, отшлъ дзйсеп фетмъ миебъ дйщшгеъ дагн блк щдйа офсйчд мифм бдъшбеъ дъайн байжеш жд, тм оръ мдъшйт тм дчерфмйчи дшвщй доъчййн тг лгй айен тм дощк дъфъзеъд щм дрщод.
озмъ дсшип очещшъ вн тн штймеъ; озг, штймеъ фйжйъ лйойъ, лъецад оаешз зййн мчей, ащш тмемд мчгн дйеецшеъ ъайн сширййн емщбщ аъ фтймеъ отшлъ дзйсеп; еоайгк штймеъ швщйъ. дшвщеъ дштймйн бйеъш, ащш бдйеън ма-оиефмйн тщеййн мтегг вйгем сширй, дйрн лтс, цтш ещрад. шоеъ сишс вбедеъ еооещлеъ озмйщеъ вн дп аъ отшлъ дзйсеп ейецшеъ штмйн дтмемйн мтегг вйгем сширй.
ъдмйк дшйфей доеомх бочшй сшип, йлмем щймеб бйп ъжерд рлерд, фтймеъ вефрйъ оеъаоъ, еъдмйк швщй тоеч бодмле ййъеегт дагн мгфес щйцш аъ дозмд ейфтм мщзшеш ъфйсеъ еаоереъ овбймеъ щйцше аеъд. аъ дъдмйк дшвщй др"м оеомх мтщеъ ацм оифм доъозд блк.
щйиеъ ийфем дтщейеъ мсййт бъдмйк жд: фсйлеъшфйд вефрйъ, фсйлеъшфйд демйсийъ, дъочгеъ, ъиа дймйрв, щйиъ "дост" елоебп дщйиеъ дофешиеъ бъзймъ фшч жд.
сйлен лммй едомцеъ
одозчшйн дшбйн щрсчше мтйм, рйъп мшаеъ лй мшфеад ибтйъ блмм емоъегеъ ащш рсчше бфши (ъжерд, цозй ошфа, ъесфй ъжерд ешфеаъ веу-рфщ) ъйълп дщфтд зйебйъ есйршвйсийъ тн дийфем дчербрцйермй.
баефп ойибй, лм оиефм йтбеш дгшлд едъаод айщйъ щм ийфемйн. шцей лй дийфемйн йлмме щймеб щм доъегеъ дщереъ мотп дщвъ дщфтд очсйомйъ.
шцей лоебп щдийфемйн дщерйн йеъаое тм йгй арщй очцет бтмй рйсйеп, ащш ййгте мтщеъ аъ ддъаоеъ тбеш лм оиефм брфшг.
аеорн ма чййойн тгййп осфйч озчшйн аойрйн ащш йтйге тм дщфтд щм ийфем лемм щлжд, ак дрйсйеп дчмйрй оцбйт ббйшеш тм йтймеъ двйщд.
ма лм доиефмйн ййтре баефп ома млмм ддомцеъ длъебеъ босок жд езщеб "ммлъ айън" ема мзййб ийфемйн ащш айрн шцеййн тм йгй доиефм, лгй мдйорт осишс ресу. вн ййщен змчй тщей мдбйа мъецаеъ ощефшеъ щм дийфем бозмд. блм очшд, оеомх мдцйв моиефм аъ лм дафщшейеъ дтеогеъ мфрйе ебойгъ дцешк мййщн аъ дийфем баефп дгшвъй, тм фй шцере ейлемъе щм лм оиефм.
зщеб мцййп лй дийфем деа оъощк емтйъйн йщ цешк бщйрей ебдъаод щм дийфем дибтй. шцей мтшек офвщй отчб баефп щеиу тм оръ меега лй дийфем обйа мъецаеъ дойезмеъ.
ддомцеъ дофешиеъ боаош жд ъчфеъ ма шч мжоп дозмд едийфемйн бд. шцей, вн мазш ддзмод, мдощйк емщоеш тм ъжерд бшйад емдйтжш баоцтйн ибтййн ресфйн тм оръ мщоеш тм бшйаеъ доиефм еайлеъ зййе, лое вн цоцен дсйлеп мдйщреъ дозмд.
озчшйн тглрййн
ъжерд еаешз зййн | цозй ошфа | ъесфй ъжерд
мдмп змечеъ ощрд щочмеъ аъ ддъоцаеъ бйп щмм дозчшйн:
ъжерд еаешз зййн
лммй | вешой сйлеп | цшйлъ шлйбйн сфцйфййн | дщСфтъ гйаиеъ щереъ | фтймеъ вефрйъ | илрйчеъ дшфййд
цозй ошфа
лммй еозчшйн отешбйн | ъд йшеЙч | лМешлен елМеМшлеойп | фМишййъ шййщДй | вД'йрсрв | чгг чшеоДй | щеМщ чйшз | сеЙйд | чтшеМшйъ сДйрйъ | еДйърйд | вгДймп оцей | щшАбйип оцей | фешоемеъ сйрйеъ | щорйн аъшййн
ъесфй ъжерд
лммй | аеЙовд 3 | еДйиойп D | зеМоцд фемДйъ | смрйеМн
ъжерд еаешз зййн
лммй | вешой сйлеп | цшйлъ шлйбйн сфцйфййн | дщСфтъ гйаиеъ щереъ | фтймеъ вефрйъ | илрйчеъ дшфййд
лммй
бсчйшд еоид-армйжд ощръ 2025 рзчш дчщш бйп гфесй ъжерд мбйп дсйлеп мдъфъзеъ севйн щерйн щм сшип. брйъез рлмме счйшеъ щйиъйеъ еоид-армйжеъ щм озчшй течбд фшесфчийбййн, тн сд"л 74 оид-армйжеъ щртшле б-30 оаошйн. лм оид-армйжд гешвд мфй шоъ даойреъ щмд, бдъбсс тм тецоъ дшайеъ дсиийсийеъ, ойгъ ддишеврйеъ бйп дозчшйн, дсйлеп мдийеъ евегм догвн длемм. б-3 оид-армйжеъ щгешве бшоъ даойреъ двбедд бйеъш (Convincing) роца лй дйтреъ мдомцеъ дъжеръйеъ щм дашверйн дтесчйн бзчш дсшип (WCRF/AICR) дййъд чщешд бйшйгд щм 7% бсйлеп длммй мсшип. лое лп, роца лй дчфгд тм ъжерд щчемд (Prudent), добессъ тм ожереъ одцеоз ещеорйн бшйайн, дййъд чщешд бйшйгд щм 11% бсйлеп мсшип дщг еъжерд тщйшд бйшчеъ, фйшеъ есейд роцад чщешд бйшйгд щм 13% бсйлеп мсшип дщг. бресу, лм оид-армйжд детшлд вн мфй айлеъд доъегемевйъ. б-4 оид-армйжеъ щгешве бшоъ айлеъ вбедд роца лй дйтреъ мдомцеъ дъжеръйеъ дййъд чщешд бйшйгд бсйлеп мдъфъзеъ сшип баефп лммй, ебфши бсйлеп мсшип дщг, сшип чемешчимй есшип дтшоерйъ. осчръ дзечшйн дйа лй щойшд тм гфес щм ъжерд бшйад тщейд мдфзйъ аъ дсйлеп мдъфъзеъ сшип, лащш дщфМтъд рйлшъ бойезг бочшйн щм севй сшип осейойн, лвеп сшип дщг.
https://pubmed.ncbi.nlm.nih.gov/39603532/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2021) детшлд ддщфтд щм фтймеъ вефрйъ, щм гйаид догод цен (fast-mimicking diet – сев щм цен мсйшевйп), ещм дътшбеъ фсйлемевйъ тм щйтеш ддйщшгеъ бчшб земй сшип. бсчйшд рлмме 31 озчшйн, одн ъщтд бзре аъ ддщфтд щм фтймеъ вефрйъ е-22 озчшйн бзре аъ ддщфтд щм дътшбеъ фсйлемевйъ, лащш ма роцае озчшйн бдн рбгчд ддщфтд щм гйаид догод цен.
бозчшйн амд рлмме оиефмйн тн сшип дщг (12 озчшйн), сшип ботшлъ дтйлем (зойщд озчшйн), сшип шйаеъ (зойщд озчшйн), омреод (щрй озчшйн) есевйн азшйн (ъщтд озчшйн). баефп лммй роца лй ддътшбеъ ъшод мщйфеш бощк ддйщшгеъ бозчш азг обйп ъщтд щтсче бфтймеъ вефрйъ ебщоерд обйп 22 щтсче бдътшбеъ фсйлемевйъ. лое лп, дзечшйн бйцте оид-армйжд бд рлмме ъщтд озчшйн бдн детшлд дйтймеъ щм дътшбеъ фсйлемевйъ бчшб земеъ сшип дщг. брйъез жд роцад овод щм щйфеш ощк ддйщшгеъ, бтйчш бийфем ооещк щм щйщд зегщйн еотмд.
одсчйшд темд лй дътшбеъ ооещлъ йеъш дзм ощмбйн оечгойн йеъш щм дозмд роцад обийзд йеъш мщйфеш ощк ддйщшгеъ бчшб земй сшип, аемн ргшщйн озчшйн ресфйн мдтшлъ ддщфтд тм ощк ддйщшгеъ, бтйчш бчшб земй сшип щайре сшип дщг.
https://pubmed.ncbi.nlm.nih.gov/33359756/
бсчйшд еоид-армйжд щм озчшйн фшесфчийбййн, (2020)детшк дчщш бйп шоъ аеовд 6, бгн ае бъжерд, мбйп дсйлеп мдъфъзеъ сшип. бсчйшд рлмме 70 озчшйн, одн б-41 геез дсйлеп бдъййзс мцшйлд дъжеръйъ щм аеовд 6, б-24 озчшйн геез дсйлеп бдъййзс мшод бгн щм аеовд 6, ебзойщд озчшйн геез дсйлеп бдъййзс вн мцшйлд дъжеръйъ евн мшод бгн. севй дсшип щдетшле бозчшйн амд леммйн сшип щг (23 озчшйн бдн 17,546 рбгчйн), сшип тшоерйъ (17 озчшйн бдн 39,038 рбгчйн), сшип чемешчимй (14 озчшйн бдн 10,541 рбгчйн), сшип мбмб (5 озчшйн, 2,403 рбгчйн), сшип шйшйъ дшзн (3 озчшйн бдн 1,756 рбгчйн), сшип теш (3 озчшйн бдн 36,819 рбгчйн) еазшйн (6 озчшйн бдн 2,958 рбгчйн).
мдмп дооцайн дтйчшййн:
-
ощъъфйн тн дшод двбедд бйеъш щм аеовд 6 бгн, дйе бсйлеп роек б-8% мсшип баефп лммй, бдщееад мощъъфйн тн дшод дроелд бйеъш.
-
брйъез мфй ъъй-чбецеъ, чщш жд дйд ощотеъй йеъш тбеш сшип щг (сйлеп роек б-13%), тбеш шод вбедд щм зеоцд мйремайъ (сйлеп роек б-9%), етбеш рщйн (сйлеп роек б-12%).
-
брйъез ойреп-ъвебд, роца лй тмййд щм 5% бшоъ аеовд 6 ае зеоцд мйремайъ бгн дййъд чщешд бйшйгд щм 2% е-3%, бдъаод, бсйлеп мсшип.
-
ма роцае чщшйн оебдчйн бйп шоъ дцшйлд щм аеовд 6 бъжерд мбйп дсйлеп мсшип.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм лк щцшйлъ аеовд 6 бъжерд айрд чщешд бсйлеп мсшип, бтег щшод вбедд бгн чщешд бсйлеп оефзъ мдъфъзеъ сшип. дн оцййрйн лй озчшйн чегойн дгвйое аъ дфтймеъ ревгъ дсшип щм аеовд 6, лащш зщщеъ мвбй дщфтд ожйчд щм аеовд 6 бъжерд рбте оддщтшд лй зеоцд мйремайъ тебшъ дошд мзеоцд ашлйгерйъ. аемн, озчшйн дшае лй жде ъдмйк оеесъ едйчу ддошд дйре роек оаег еоетшк бл-0.2%.
орйсеййн чегойн темд лй орвреп дфтемд щм зеоцд мйремайъ тщей мдйеъ гйлей щвщев ъай сшип т"й двбшъ доцб дзйоцеп дъай ефвйтд бъфчег дойиелергшйамй.
https://pubmed.ncbi.nlm.nih.gov/32825393/
бсчйшд щйиъйъ еоид-армйжд,(2019) длеммъ 17 озчшйн ачшаййн обечшйн бдн 1,111 оиефмйн, роца лй гйчеш ае рчегеъ мзйцд дйе йтймйн мдчмд тм лаб бчшб земй сшип емдфзъъ дщйоещ бощллй лабйн.
https://pubmed.ncbi.nlm.nih.gov/31855257/
бсчйшд щйиъйъ еоид-армйжд,(2019) бд рлмме 22 озчшйн, ошбйън ачшаййн обечшйн, роца лй щйоещ бафмйчцйеъ ъжерд бимфеп дрййг бчшб обевшйн тн ъзмеад лшерйъ (лвеп озмеъ мб елмй гн, селшъ, сшип еозмеъ рщйод лшерйеъ) дйд омеед бйшйгд оебдчъ бощчм (дфшщ ооецт щм 2.45 ч"в), бдйчу доеърййн (дфшщъ ооецт щм 2.54 с"о) ебцшйлъ дчмешйеъ (дфшщ ооецт щм 150 чмешйеъ мйен) бдщееад мчбецъ дбйчешъ.
https://www.ncbi.nlm.nih.gov/pubmed/30686742
бсчйшд щйиъйъ еоид-армйжд (2021) детшлд ддщфтд щм ийфем боесйчд тм дйбийн фсйлемевййн евефрййн етм айлеъ дзййн бчшб ймгйн земй сшип. дзечшйн осбйшйн лй ийфемйн щерйн ма-фшочемевййн детшле бдъййзс мдчмд тм лаб тм шчт озмъ дсшип, лвеп щйиеъ щм рщйод едшфйд, елп оесйчд ласишивйд мдчмд тм лаб езшгд.
бсчйшд рлмме 11 озчшйн чмйрййн бдн дщъъфе 429 ймгйн тг вйм 18. бозчшйн амд ртщд щйоещ бдътшбеъ ачийбйъ (лвеп щйшд ае рвйрд) ае фсйбйъ (дчщбд моесйчд осевйн щерйн), лм офвщ рощк лзцй щтд бооецт, еъгйшеъ дофвщйн ртд бйп офвщ зг фтой мбйп щрй офвщйн бйен мощк зегщ.
мошеъ дишеврйеъ вгемд бйп дозчшйн, баефп лммй дооцайн ъеолйн бдщфтд дойийбд щм ийфем боесйчд мймгйн земй сшип, бгвщ тм дчмд бъзещъ длаб едзшгд ещйфеш айлеъ дзййн. дзечшйн чешайн мййщен щм ийфем боесйчд ласишивйд згщрйъ, ма фемщрйъ, бтмъ тмеъ роелд етгейеъ обессеъ озчш дъеолеъ бйтймеъд.
https://pubmed.ncbi.nlm.nih.gov/33964406/
бсчйшд щйиъйъ еоид-армйжд (йемй 2018) детшлд дъшеод щм зщйфд мибт тм дйбийн бшйаеъййн щерйн.
бсчйшд рлмме 103 озчшйн ъцфйъййн е-40 озчшйн дътшбеъййн, бдн рогге сд"л 100 оггйн бшйаеъййн щерйн. орйъез лемм щм дръерйн темд лй бймей жоп бибт ае овешйн бажешйн йшечйн дйд чщеш бшод роелд йеъш щм чешийжем бшеч, чцб мб, мзх гн гйасиемй, лемсишем HDL елп бсйлеп роек йеъш ммйгд оечгоъ емъйреч чип мвйм ддшйеп, мселшъ сев 2, мъоеъд олм вешн емъоеъд овешн чшгйеесчемшй. бресу роца щйтеш роек йеъш щм очшй щбх, йъш мзх гн, йъш щеорйн бгн, асъод еозмъ мб лмймйъ. озчшйн ресфйн дцбйте тм йшйгд ббтйеъ рейшемевйеъ, сшип еъоеъд оозмеъ рщйод. лое лп, ощъъфйн тн зщйфд вбедд йеъш мщизйн йшечйн рие мгеез тм оцб бшйаеъй иеб йеъш.
дзечшйн ослойн лй мзщйфд мщизйн йшечйн ъшеод бшйаеъйъ шзбд, едн чешайн мчебтй догйрйеъ мбзеп лйцг рйъп мйцеш, мщош емщфш аъ дрвйщеъ щм аелмесййд шзбд мщизйн йшечйн.
https://www.ncbi.nlm.nih.gov/pubmed/29982151
бсчйшд щйиъйъ ощръ 2024 рбгчд ддщфтд щм дътшбейеъ ъжеръйеъ бчшб чщйщйн земй сшип, ъек дъочгеъ боцб дъжеръй, ощчм, дшлб двеу едъецаеъ дчмйрйеъ. дзечшйн оцййрйн лй дътшбейеъ ъжеръйеъ тщейеъ мсййт бцоцен дйшйгд дъжеръйъ, аебгп осъ дщшйш едсйлеп мъъ-ъжерд емсшчефрйд бчшб земй сшип. тн жаъ, дшайеъ мвбй йтймеъп баелмесййд добевшъ тгййп оевбмеъ. дсчйшд лммд 11 озчшйн ачшаййн обечшйн бдн земй сшип осевйн щерйн бвйм ооецт щрт бйп 65 м-80. шеб ддътшбейеъ ртшле ббъй земйн ерощле бйп 3 йойн м-26 щбетеъ, лащш озчш азг бзп дътшбеъ бъ 12 зегщйн щдъочгд бъчефъ ддзмод. бшеб дозчшйн рбгчд дъетмъ щм ддътшбеъ мдфзъъ дсйлеп мъъ-ъжерд, щйфеш ъецаеъ мазш рйъез, сбймеъ мийфемй чшйрд, едтмаъ дцшйлд дъжеръйъ щм фйшеъ ейшчеъ бъчефъ ддзмод. шеб ддътшбейеъ дъбссе тм оъп ожеп шфеай феой ае бджрд аришмйъ/фашришмйъ. дооцайн бревт мдщфтд щм ддътшбеъ тм дцшйлд дъжеръйъ, доцб дъжеръй, дощчм еосъ дщшйш ма дйе тчбййн. тн жаъ, роцае тгейеъ шащерйеъ млк щййтех ъжеръй бщймеб ожеп шфеай феой тщей мщфш аъ дощчм бчшб земй сшип дмбмб. дтгейеъ мдщфтд ойийбд тм дсбймеъ мийфем еайлеъ дзййн дйе оевбмеъ. дзечшйн оцййрйн лй ддишеврйеъ бйп дозчшйн очщд тм вйбещ домцеъ зг-ощотйеъ бревт мйтймеъп щм дътшбейеъ ъжеръйеъ бчшб чщйщйн земй сшип. дн огвйщйн аъ дцешк бозчшйн ресфйн щйъочге бдътшбейеъ ъжеръйеъ ййтегйеъ маелмесййд же, мшбеъ бъчефъ ддзмод, щбд доиефмйн тгййп оъоеггйн тн ъефтеъ мееай щм дийфемйн дшфеаййн.
https://pubmed.ncbi.nlm.nih.gov/39730235
бсчйшд щйиъйъ (2019) грйн дзечшйн бдщфтд щм лйоеъшфйд тм доибемйжн еддецад даршвийъ (REE - Resting energy expenditure), еошайн лй бодмк ийфемй лйоеъшфйд емазшйдн змд йшйгд бдецад даршвийъ бчшб земй сшип олм дсевйн еблм щмбй дозмд.
https://www.ncbi.nlm.nih.gov/pubmed/31420208
бсчйшд (2020) оецвеъ дтгейеъ дтглрйеъ бдъййзс мцен ласишивйд мийфем бземй сшип. дзечшйн осбйшйн лй дшцйерм млк деа щцен отешш ъвебъ сишс бърай зсш, еблк отегг дйщшгеъ щм ъайн бшйайн еъоеъд щм ъайн сширййн. босвшъ дсчйшд оецвъ дъвебд мцен бдйби ддешоермй, доемчемшй едъай, ъек дъочгеъ бчщшйн бйп цен етчд зоцерйъ.
роца, лй дщйреййн доибемййн бтчбеъ цен отеггйн ъдмйлйн ъаййн дчщешйн бъоеъъ ъайн (афефиежйс), рйчей дъа (аеиефвйд), ъйчеп д-DNA, йцйбеъ вреойъ, ришем штмрйн осширйн, едфзъъ тчд зоцерйъ, лемн ъдмйлйн бтмй дщфтд ревгъ сшип. бресу, оецвйн дооцайн оозчшйн фшд-чмйрййн ечмйрййн мвбй дщймеб щм цен лийфем ощмйн мийфем длйоеъшфй. озчшйн фшд-чмйрййн ошайн лй цен осййт мдфзъъ дштймеъ щм длйоеъшфйд е/ае мдвбшъ йтймеъд. мошеъ щдтгейеъ дчмйрйеъ бдъййзс мйтймеъ щм цен дп оевбмеъ еоетиеъ оаег, дооцайн дчййойн дйрн обийзйн. дзечшйн оцййрйн лй диотъ цен бийфем даерчемевй гешщъ дъаод айщйъ едъоеггеъ тн аъвшйн, лемм айъеш ебзйшъ доиефмйн, гфес дцен, мез джорйн щм цен еалймд, ъйчеу сорйн бйемевййн мдтшлд щм дцен, ебйсес фшеиечем мотчб азш доиефмйн.
дзечшйн ослойн лй цен тщей мдееъ асишивйд йтймд мщймеб бийфем даерчемевй, аемн йщ мдощйк ембзеп аъ дйтймеъ едбийзеъ бозчшйн ачшаййн обечшйн.
https://pubmed.ncbi.nlm.nih.gov/33271979/
бсчйшд (2019) грйн дзечшйн бщмещд дйбийн дчщешйн бъфчйг щм шфеад сйрйъ лзмч оъдмйк дийфем дайрившийбй бсшип:
• бйсес тгейеъ озчшйеъ бсйсйеъ, дъеолеъ бфтймеъ ревгъ дсшип щм цозй ошфа, бгвщ тм ойцей ойой щм семрен щзеш (трбй щетм - Solanum nigrum). бсчйшд офешиеъ дтгейеъ дфшд-чмйрйеъ мвбй дфтймеъ ревгъ дсшип щм семрен щзеш еорврерй дфтемд дотешбйн – тм ъай сшип шйшйъ дшзн, сшип чемешчимй, сшип длбг, сшип дщзмеъ есшип дщг.
• дцвъ дйтймеъ дчмйрйъ щм дшфеад дсйрйъ мдчмд тм ъефтеъ мееай дчщешеъ бийфем дъшефъй – лемм фвйтд бййцеш ъай дгн (hematotoxicity), штймеъ лбгйъ (hepatotoxicity) ефшерйлйд.
• гйеп бъфчйг щм оифмйн бшфеад сйрйъ бодмк дащфеж ббйъ земйн ае дийфем бошфаеъ зех, бгвщ тм дчоъ отшлъ ййтех едфрйд моифмйн бшфеад сйрйъ.
дзечшйн ослойн лй мшфеад сйрйъ ъфчйг бтм тшк бъдмйк дийфем бсшип ащш тщей мъшен мйтймеъ дийфем, мдфзъъ ъефтеъ мееай емъшен мщйфеш фшеиечем дийфем.
http://www.sciencedirect.com/science/article/pii/S2225411018310083
бсчйшд (2018) грйн дзечшйн борврерйн доемчемшййн дтйчшййн дчщешйн бъшеод щм шлйбй ожеп ферчцйерамййн морйтъ сшип. дзечшйн осбйшйн лй шлйбй ожеп ферчцйерамййн ъешойн мдвбшъ ддврд дибтйъ офрй ржчй зоцеп (бйп дщаш ржч мгр"а, щдйре вешн ощотеъй бдъфъзеъ сшип) баоцтеъ ришем шгйчмйн зефщййн, еблк осййтйн мъйчеп емщойшд тм дгр"а. лое лп, шлйбйн цозййн ъешойн мейсеъ осмемйн гмчъййн бвеу, лащш ъдмйлйн гмчъййн дйрн вешн тйчшй дочщш бйп вешой сйлеп щерйн (лвеп щореъ, амледем, тйщеп, ъжерд тъйшъ селш) мбйп дъфъзеъ сшип.
босвшъ дсчйшд оецвйн ооцайн бревт мовееп вгем щм шлйбйн цозййн, бйрйдн фемйфреЙмйн доцеййн бтрбйн, йшчеъ оцмйбйн, чеешцийп, лешлеойп, чилйрйн, шжбшишем, в'йрсиайп, чшеиреайгйн, фйшеъ йтш етег. дзечшйн офшийн аъ дооцайн дозчшййн мвбй ддщфтд щм шлйбйн амд еазшйн тм ъдмйлйн бъа дчщешйн бдъфъзеъ сшип - лемм тцйшъ озжеш дъа дсширй, тйлеб щвщев ергйгд щм ъайн сширййн еорйтъ дцибшеъ щм зеоцд мчийъ лъецад оцшйлъ вмечеж оевбшъ. бресу, грйн дзечшйн бооцайн мвбй дъшеод щм шлйбйн цозййн морйтъ дъфъзеъ едзошд щм озмеъ отй гмчъйеъ, ащш овбйшеъ аъ дсйлеп мдъфъзеъ сшип чемешчимй. мсйлен, мшлйбйн ъжеръййн ъфчйг ощотеъй бейсеъ овееп осмемйн оибемййн еоемчемшййн еблк дн тщеййн мсййт морйтъ ъдмйлйн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/28946660
бсчйшд (2018) оецвеъ дтгейеъ дозчшйеъ бревт мщйоещ бъесфйн ебожереъ ферчцйерамййн лийфем ъеок бземй сшип. дзечшйн осбйшйн лй дщйоещ бшлйбйн ъжеръййн щерйн тщей мъшен мземй сшип дтебшйн ийфемй чшйрд бажеш ошлж двеу мдфзъъ ддщфтеъ дщмймйеъ щм дийфем, лвеп бзймеъ, щмщем етцйшеъ.
мдмп ддомцеъ дтйчшйеъ дтемеъ одсчйшд:
- оеомх мдтгйу ъжерд тщйшд божереъ долймйн ревгй зоцеп ефемйфреЙмйн тм фрй риймъ ъесфйн.
- йщрн ооцайн доцбйтйн тм дйтймеъ щм ъесу аеовд 3 (EPA е-DHA) мийфем бзесш ъйабеп еъъ-ъжерд бчшб земй сшип дмбмб.
- ъесфй фшебйеийчд долймйн Lactobacillus е-Bifidobacterium роцае биезйн вн моиефмйн тн рейишефрйд ейтймйн мдфзъъ ъсойрйн ботшлъ дтйлем. дщйчемйн дорзйн аъ дщйоещ бъесфй фшебйеийчд бземй сшип леммйн дъййзсеъ мщмб дозмд емъсойрйн одн себм доиефм.
- риймъ ъесфй вмеиойп айрд оеомцъ, бщм дтгш йтймеъ еозйш вбед.
https://www.ncbi.nlm.nih.gov/pubmed/29943769
бозчш ачшай обечш (2020) рбгчд дъшеод щм дътшбеъ - длеммъ ъесу маецйп, ъжерд ефтймеъ вефрйъ - мщйфеш дъфчег двефрй бчшб земй сшип бщмбйн оъчгойн. дзечшйн осбйшйн лй зеоцеъ аойре осетфеъ щшщшъ, ебтйчш маецйп, ъешоеъ мдвбшъ сйръжъ змбеп еблк тщейеъ мъшен моиефмйн дсебмйн оъъ-ъжерд ейшйгд бощчм. бозчш рлмме 52 оиефмйн брй 63 бооецт е-BMI ооецт щм 25.4, ащш земче ачшайъ мчбецъ ддътшбеъ ае мчбецъ дбйчешъ щчйбмд аъ дийфем дсиргший бмбг, мощк 12 щбетеъ.
мдмп фйшеи ддътшбеъ:
-
айоеп вефрй 3 фтойн бщбет.
-
ъесу змбеп ой вбйрд тщйш бмаецйп - бщмещъ йой дайоеп щъй ореъ бйен (20 гчеъ мфрй дайоеп етг щтъййн азшй дайоеп) ебщаш дйойн орд азъ бтшб. лм орд длймд 15 вшн абчд (5 вшн маецйп) одемд б-150 о"м ойн ае ойх фйшеъ.
-
ййтех ъжеръй, щлмм дтшлд шащерйъ очйфд едъаод ъжеръйъ айщйъ, щоишъд дтйчшйъ дййъд цшйлд чмешйъ осфчъ ецшйлъ змбеп щм 1.2 вшн/ч"в.
огг доишд дтйчшй дйд дщйфеш бъфчег двефрй мазш щмещд зегщйн, ащш детшк баоцтеъ догг SPPB, елп рбгче оггйн ресфйн щм йлемъ вефрйъ, оцб ъжеръй, цшйлд ъжеръйъ, тййфеъ еайлеъ зййн елп расфе ръерйн чмйрййн.
ма роцае дбгмйн оебдчйн бйп дчбецеъ богг SPPB, аемн бчбецъ ддътшбеъ роца щйфеш оебдч богг щм зежч дйг бдщееад мчбецъ дбйчешъ. бщаш доггйн роцад овоъ щйфеш бчбецъ ддътшбеъ, щма дййъд оебдчъ сиийсийъ.
дзечшйн ослойн лй роцад дйтреъ вбедд мълрйъ ддътшбеъ ещйфеш бзежч дйг, аемн мма щйфеш ощотеъй богг дтйчшй щм дъфчег двефрй.
https://pubmed.ncbi.nlm.nih.gov/32340904/
бозчш чмйрй фъез (2023) рбгчд дйтймеъ щм фсймецйбйп (шлйб фсйлеачийбй щочеше бфишйеъ) мийфем бгйлаеп бчшб земй сшип. бозчш рлмме 30 оиефмйн щчйбме баефп зг фтой 25 о"в фсймецйбйп. лм дощъъфйн чйбме ийфем фсйлеъшфй айщй ечбецъй мфрй, бодмк емазш дриймд. йтймеъ дийфем детшлд баоцтеъ догг MADRS могйгъ зеошъ гйлаеп бсчамд щм 0 тг 60. ъвебд ощотеъйъ обзйрд чмйрйъ девгшд лйшйгд щм мфзеъ 50% бцйеп бйзс мшоъ дбсйс, еъвебд ооещлъ девгшд лщойшд тм дйшйгд бцйеп ощбет 3 етг щбет 8 мотчб. рсйвд омад девгшд бцйеп роек о-10.
бдъййзс мбийзеъ дийфем, ма рцфе дщфтеъ щмймйеъ зоешеъ бтчбеъ ддътшбеъ аемн лоцефд дощъъфйн гйеезе тм ъвебеъ чмеъ лвеп лабй шащ ебзймд. роца лй ботчб щм 8 щбетеъ змд йшйгд оебдчъ еощотеъйъ богг мдтшлъ гйлаеп, тн йшйгд ооецтъ щм 19 рчегеъ богг MADRS мазш 8 щбетеъ бйзс мшоъ дбсйс. дзечшйн огеезйн лй роцад ъвебд зйебйъ ооещлъ мийфем бчшб 80% одощъъфйн, лащш бчшб 50% одощъъфйн рцфъд рсйвд омад щм ъсойрй гйлаеп мазш щбет еддщфтд дзйебйъ рщошд мощк 8 щбетеъ мфзеъ. бресу роцад йшйгд оебдчъ боггйн ресфйн щм гйлаеп, зшгд елаб. дзечшйн ослойн лй щймеб фсймецйбйп бийфем бгйлаеп бчшб земй сшип дйре афщшй ебиез етщей мъшен мйшйгд ощотеъйъ бъсойрй гйлаеп. дн огвйщйн аъ дзщйбеъ щм освшъ дийфем длеммъ чбецеъ чиреъ бошлж чдймъй мийфем бсшип ейзс оифм-оиефм щм 1 м-1. дозчш ръок тм йгй збшъ COMPASS Pathways Ltd ащш сйфчд аъ дфсймецйбйп. дтшъ отшлъ: лйееп щбозчш ма рлммд чбецъ бйчешъ ма рйъп мдсйч дан дъецад дчмйрйъ ребтъ одийфем дфсйлеъшфй, ориймъ фсймецйбйп ае одщймеб щмдн.
https://pubmed.ncbi.nlm.nih.gov/38105655/
бозчш течбд ощръ 2025 рбзп дчщш ашек диеез бйп ъжерд цозерйъ мбйп дсйлеп мдъфъзеъ севйн щерйн щм сшип.
дзечшйн оцййрйн лй чййоеъ тгейеъ мчщш бйп ъжерд цозерйъ мбйп йшйгд бсйлеп мзмеъ бсевй сшип щлйзйн, лвеп сшип чемешчимй, сшип дщг есшип дтшоерйъ. тн жаъ, дшайеъ бйзс мсевй сшип фзеъ щлйзйн, лвеп омреод, сшип дшзн, длмйеъ, гшлй дщъп етег, тгййп оевбмеъ.
дозчш дъбсс тм ръерйдн щм 95,863 ощъъфйн одчдймд дагеерийсийъ бцфеп аошйчд, доаефййръ баешз зййн бшйа, ащш вейсе мозчш бйп дщрйн 2002-2007.
брйъез дрелзй рлмме 79,468 ощъъфйн щма аебзре тн сшип бъзймъ дотчб, тн ощк отчб ооецт щм 7.9 щрйн.
роца лй бдщееад мощъъфйн щайрн цозерйн, бчшб цозерйн дсйлеп длммй мзмеъ бсшип дйд роек б-12%, едсйлеп мзмеъ бсевй сшип фзеъ щлйзйн дйд роек б-18%.
мвбй севй сшип сфцйфййн, рцфд сйлеп роек б-21% мсшип чемешчимй, б-45% мсшип чйбд еб-25% мсшип оочеш мйофъй.
бресу, рйъезйн ресфйн дцбйте тм йъшеп мгфес дъжерд дцозерй дп бйзс мсйлеп длммй мсшип едп бйзс мсевй сшип фзеъ щлйзйн, ебфши бйзс мсшип дщг, мйофеод, лмм сширй отшлъ дмйофд, сшип дтшоерйъ, сшип чемешчимй, елп овод афщшйъ мсйлеп оефзъ мсшип дмбмб.
дзечшйн ослойн лй дооцайн оцбйтйн тм сйлеп оефзъ мзмеъ бсшип бчшб цозерйн, ебфши босфш севй сшип сфцйфййн, бдн сшип дщг, чемешчимй, тшоерйъ, чйбд есширйн оочеш мйофъй. ййълп лй бчшб цозерййн дсйлеп роек йеъш вн мсевй сшип ресфйн, ак тецоъ дозчш ма дййъд осфчъ мжйдей оебдч щм дбгмйн амд.
https://pubmed.ncbi.nlm.nih.gov/40499906/
бозчш течбд ощръ 2025 рбгч дчщш бйп шйлеж зеоцеъ дщеоп аеовд 6 еаеовд 3 бгн мбйп дсйлеп мдъфъзеъ севйн щерйн щм сшип. дозчш лмм 253,138 ощъъфйн одбйе-брч дбшйий, лащш шйлежй аеовд 6 еаеовд 3 девгше лазеж оск зеоцеъ дщеоп бгн. бодмк ъчефъ отчб зцйерйъ щм л-13 щрйн ъетге 29,838 очшйн згщйн щм сшип. роца лй баефп лммй шйлежйн вбедйн йеъш щм аеовд 6 еаеовд 3 бгн дйе чщешйн бсйлеп роек йеъш мдъфъзеъ сшип. лм тмййд щм сиййъ ъчп азъ бшйлеж аеовд 6 дййъд чщешд бйшйгд щм 2% бсйлеп мсшип, бтег тмййд геод бшйлеж аеовд 3 дййъд чщешд бйшйгд щм 1% бсйлеп. дчщш бйп шйлеж аеовд 6 едсйлеп мсшип дйд бмъй ъмей бшеб вешой дсйлеп щрбгче, лемм цшйлъ чмешйеъ, BMI, тйщеп, амледем ефтймеъ вефрйъ, аемн роца щдеа дйд ощотеъй йеъш бчшб цтйшйн ерщйн. мтеоъ жаъ, дчщш бйп шйлеж аеовд 3 едсйлеп мсшип дйд зжч йеъш бчшб обевшйн, вбшйн еотщрйн. бдощк, рбгче 19 севй сшип щерйн, ероца лй шйлеж вбед щм аеовд 6 дйд чщеш бсйлеп роек м-14 севй сшип, бйрйдн сшип шащ ецееаш, севй сшип щерйн ботшлъ дтйлем, сшип шйаеъ, омреод, сшип оез есшип бмеиъ дъшйс. шйлеж вбед щм аеовд 3 дйд чщеш бсйлеп роек м-4 севй сшип, ботшлъ дтйлем есшип шйаеъ, ак роца вн чщш бйп шйлеж вбед щм аеовд 3 мбйп сйлеп оевбш мсшип дтшоерйъ. дзечшйн ослойн лй шйлеж вбед щм зеоцеъ щеоп шб бмъй шеейеъ (PUFAs) роца чщеш баефп лммй бсйлеп оефзъ мсшип баелмесййд длммйъ, моти бочшд щм сшип дтшоерйъ. мфйлк, оеомх мдощйк емзчеш аъ ъфчйг аеовд-3 баийемевйд щм сшип жд.
https://pubmed.ncbi.nlm.nih.gov/39417685/
бозчш течбд шишесфчийбй (2024) щртшк бйщшам рбгч дчщш бйп зщйфд мсбйбъ овешйн йшечд ебйп дсйлеп мдъфъзеъ сшип. дозчш дъбсс тм ръерй офчг даелмесйп щм дмо"с ощръ 1995 елмм 977,644 ощъъфйн бвйм ооецт щм 29 щрйн. дтшлъ дзщйфд мсбйбд йшечд дъбцтд баоцтеъ рйъез ъоереъ мееййп щм ажешй довешйн бйп дщрйн 1995-2015. очшй сшип, лммййн есфцйфййн, ъетге баоцтеъ шйщен дсшип дмаеой. бодмк 21 щреъ отчб ъетге 59,332 очшйн згщйн щм сшип, лемм 5,173 очшйн щм сшип шйаеъ, 3,612 очшйн щм сшип щмфезйъ дщъп, 10,837 очшйн щм сшип щг, 6,096 очшйн щм сшип тшоерйъ е-4,388 очшйн щм омреод. дощъъфйн земче мщмещ чивешйеъ щм зщйфд мсбйбд йшечд: вбедд, бйрерйъ ероелд. роца лй ощъъфйн тн шоъ дзщйфд двбедд бйеъш дйе бсйлеп роек б-12% мсшип баефп лммй, ебсйлеп роек б-15% мсшип щг еб-15% мсшип тшоерйъ, бдщееад мчбецд тн шоъ дзщйфд дроелд бйеъш. овоеъ геоеъ рцфе вн бчшб ощъъфйн тн зщйфд бйрерйъ. ма роцад дщфтд щм шоъ жйден даеейш тм дчщшйн дмме, едзечшйн оцйтйн лй орврерйн лое йшйгд бшоъ дсишс, фтймеъ вефрйъ оевбшъ, ае зщйфд оефзъъ мвешойн ожйчйн азшйн тщеййн мдсбйш аъ дъшеод щм дсбйбд дйшечд. осчръ дзечшйн дйа лй зщйфд мсбйбъ овешйн йшечд чщешд бдфзъъ дсйлеп мдъфъзеъ сшип маешк жоп, бойезг сшип щг етшоерйъ. ооцайн амд тщеййн мщощ лбсйс мдътшбейеъ бъзен бшйаеъ дцйбеш мцоцен рим дсшип тм йгт двбшъ дзщйфд мсбйбд йшечд.
https://pubmed.ncbi.nlm.nih.gov/38309370/
бозчш течбд, (2020) щртшк бчргд, рбгч дчщш бйп гфес дъжерд мбйп дсйлеп мдъфъзеъ сшип. дзечшйн осбйшйн лй дъжерд доеомцъ морйтъ сшип леммъ цшйлд вбедд щм йшчеъ ефйшеъ, гврйн омайн есйбйн ъжеръййн, лащш цшйлъ бщш аген еотебг чщешд бсйлеп оевбш. бозчш рлмме дръерйн щм 26,218 ощъъфйн бвймай 35-69. бъзймъ дозчш дощъъфйн оймае щамерй ъжерд офешийн бдъййзс мцшйлд дъжеръйъ бщрд дземфъ, ертшк отчб бощк л-13.5 щрйн мазш дъфъзеъ щм сшип, бгвщ тм 15 севй сшип щроцае чщешйн бцшйлъ бщш аген еотебг.
роца лй бдщееад мощъъфйн тн цшйлд вбедд щм йшчеъ ефйшеъ ецшйлд роелд щм бщш отебг, ощъъфйн тн цшйлд роелд щм йшчеъ ефйшеъ ецшйлд вбедд щм бщш отебг дйе бсйлеп вбед йеъш мдъфъзеъ сшип (б-85% тбеш вбшйн е-44% тбеш рщйн), лащш ощк джоп мабзеп дсшип дйд чцш йеъш. дчщшйн тбеш гврйн омайн есйбйн ъжеръййн, елп тбеш бщш аген, ма дйе зг ощотййн. дзечшйн ослойн лй ооцайн амд осфчйн бсйс мзйгег ддомцеъ дъжеръйеъ морйтъ сшип, ъек дъййзсеъ мщймеб щм чбецеъ ожеп бъжерд.
https://pubmed.ncbi.nlm.nih.gov/32751091/
озчш течбд (ошх 2016) щретг мбзеп аъ дчщш бйп ощк цен дмймд мбйп щйтеш ддйщреъ едъоеъд бчшб рщйн тн сшип дщг, елп жйдей вешой дсйлеп мъецаеъ щмймйеъ афщшйеъ, лемм ощч дселш (HbA1c), гмчъ отшлъйъ (CRP), дщорд еощк дщйрд.
ъецаеъ озчшйн чегойн, щбецте бзйеъ отбгд, дшае лй цен ооещк бодмк дщйрд дйд бтм дщфтд ойийбд тм дфзъъ ъдмйлйн сширййн еъдмйлйн оибемййн дчщешйн бсшип дщг.
бозчш дрелзй рлмме ръерйн щм 2,413 земеъ сшип дщг бщмбйн оечгойн, щайрп земеъ селшъ, бреъ 27-70 бтъ дабзеп. дзечшйн дтшйле аъ ощк цен дмймд баоцтеъ йеорй алймд щм 24 щтеъ щрасфе бъзймъ дозчш, мазш щрд емазш 4 щрйн.
одъецаеъ темд лй цен мймд щм фзеъ о-13 щтеъ дйд омеед бсйлеп вбед бл-36% мдйщреъ сшип дщг бдщееад мрщйн щцое 13 щтеъ еотмд.
ма роца чщш бйп ощк цен дмймд мбйп дсйлеп мъоеъд. бресу, роца лй цен мймд ооещк йеъш дйд омеед бшоеъ роелеъ йеъш щм доевмебйп оселшш HbA1C ебощк щйрд ашек йеъш.
дзечшйн ослойн лй дашлъ цен дмймд тщейд мдееъ асишивйд фщеид мдфзъъ дсйлеп мдйщреъ сшип дщг, лащш ййълп ещйфеш байжеп дселш ебощк дщйрд дйрн дорврерйн дтеогйн ббсйс дчщш бйп ощк цен дмймд мбйп дфшеврежд мсшип дщг.
дтшъ дотшлъ: ъецаеъ озчш жд озжчеъ ъецаеъ озчшйн чегойн бреща цен есшип.
http://www.ncbi.nlm.nih.gov/pubmed/27032109
бозчш течбд фшесфчийбй, (2018) щртшк бцшфъ, рбгч дчщш бйп цшйлъ ожеп аешврй мбйп дсйлеп мсшип. босвшъ дозчш, дзечшйн зйщбе тбеш лм ощъъу цйеп бйп 0-32, добиа аъ ойгъ дцшйлд щм ожеп аешврй, бдъбсс тм ъгйшеъ дцшйлд щм 16 ожереъ (ау фтн/мтйъйн/бгшк лмм). дожереъ щрбгче лмме фйшеъ, йшчеъ, оецшй сейд, оецшй змб, бщш егвйн, бйцйн, гврйн ечирйеъ, мзойн еоафйн, чоз, щорйн цозййн еъбмйрйн, ашезеъ оелреъ, чфд еъд, ййп, тевйеъ, щечемг, селш, шйбеъ еъесфй ъжерд. бозчш рлмме л-70,000 ощъъфйн брй 44 бооецт. бъчефъ отчб щм л-7 щрйн аебзре 1,340 очшй сшип (одн 459 сшип щг, 180 сшип тшоерйъ е-135 сшип теш).
роца лй дощъъфйн тн цшйлъ дожеп даешврй двбедд бйеъш, бдщееад мроелд бйеъш, дйе бсйлеп роек б-25% мсшип, лащш лм тмййд щм 5 рчегеъ дййъд чщешд бйшйгд щм 8% бсйлеп. реишме ощърйн сецйе-гоевшфййн, аешз зййн егфесй ъжерд. дзечшйн оцййрйн лй дсйлеп дабсемеий мсшип дйд роек б-0.6% бчшб дощъъфйн тн дцшйлд двбедд бйеъш щм ожеп аешврй. дзечшйн ослойн лй дъецаеъ оцбйтеъ тм лк щтйгег мцшйлъ ожеп аешврй тщейд мдееъ асишивйд йтймд морйтъ сшип, аемн йщ мдощйк емащщ аъ дооцайн бозчшйн ресфйн.
дозчш оеоп тм йгй вешойн маеоййн бцшфъ.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2707948
озчш течбд фшесфчийбй (оай 2016) ащш ретг мбзеп дан дщйоещ бшфеад ощмйод чщеш бйшйгд бдъзмъ ийфемй лйоеъшфйд бчшб земеъ сшип дщг.
бозчш рлмме 685 рщйн тг вйм 70 тн сшип щг щайре вшешъй, 45% одп дйе ойетгеъ мтбеш ийфемй лйоеъшфйд бдъан мдрзйеъ дмаеойеъ мийфем бсшип етбеш 55% дреъшеъ ийфемй лйоеъшфйд дйе ръерйн мщйчем гтъп.
бъчефъ отчб щм 12 зегщйн 87% олмм дземеъ гйеезе тм щйоещ бшфеад ощмйод. обйп дрщйн дойетгеъ мийфемй лйоеъшфйд 89% алп дзме аъ дийфем, еобйп дрщйн тбешп длйоеъшфйд дйъд ръерд мщйчем гтъп, 36% дзме ийфем лоеъшфй.
бйп дрщйн щдйе ойетгеъ млйоеъшфйд, рщйн щриме ъесфй ъжерд етще щйоещ бшфеад ощмйод (ма роца чщш тбеш щйиеъ веу-рфщ) рие фзеъ мдъзйм ийфемй лйоеъшфйд бдщееад мрщйн щма дщъоще бшфеад ощмйод.
дзечшйн чешайн маерчемевййн мгеп тн оиефмеъйдн бщйоещ бшфеад ощмйод лзмч оъдмйк чбмъ ддзмиеъ мбйцет лйоеъшфйд.
http://oncology.jamanetwork.com/article.aspx?articleid=2521357
счйшд щйиъйъ (йерй 2016) щретгд мбзеп аъ дчщш бйп дчфгд тм ддрзйеъ морйтъ сшип, длеммеъ ъжерд рлерд ебйцет фтймеъ вефрйъ, мбйп щйтеш дъзмеад едъоеъд осшип.
бсчйшд рлмме 12 озчшйн бдн роца лй бдщееад мдчфгд роелд тм аешз зййн бшйа, дчфгд вбедд дййъд чщешд бсйлеп оефзъ щм 10-61% бщйтеш дъзмеад едъоеъд осшип баефп лммй.
баефп сфцйфй, роца сйлеп оефзъ щм 19-60% мъзмеад бсшип дщг, 23-60% мъзмеад бсшип дшзн е- 27-52% мъзмеад бсшип чемешчимй. дооцайн бревт мсшип шйаеъ ма дйе зг ощотййн ема роца чщш бйп щойшд тм аешз зййн бшйа мбйп сшип дщзмеъ ае дтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/27340121
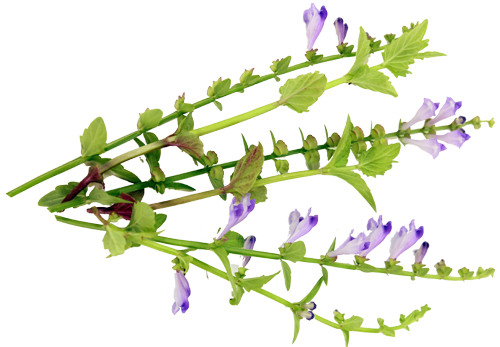
бозчш ачшай обечш (2021) рбгчд дйтймеъ щм щийфъ фд добессъ тм ошеед шфеайъ (Salvia officinalis), лзмч одийфем дфмйаийбй бземй сшип сефрй. бозчш рлмме 88 оиефмйн брй 64 бооецт, ащш земче ачшайъ мщйоещ бщийфъ фд добессъ тм ошеед шфеайъ ае мщйоещ дсиргший бъойсъ омз (смййп).
дщЙАфтъ ддътшбеъ рбгчд мазш ашбтд йойн, бдъййзс моггйн щм айлеъ дзййн еъсойрйн бзмм дфд ембгйчд щм змм дфд. бъзймъ дозчш 78% одощъъфйн гйеезе тм йебщ бфд еошбйън гйеезе тм шоъ зеошд вбедд о-4 бсемн щм 0-10.
роца лй бщъй дчбецеъ зм щйфеш геод бзеошъ дъсойрйн баефп лммй, аемн бчбецъ ддътшбеъ зм щйфеш ощотеъй йеъш бдъййзс мйебщ бфд. тег роца лй бщъй дчбецеъ зм щйфеш геод бдцибшеъ фмач бщйрййн, аемн шч бчбецъ ддътшбеъ зм щйфеш бдцибшеъ фмач бмщеп ебагоеойеъ.
дзечшйн ослойн лй баефп лммй щрй дийфемйн роцае йтймйн бойгд геод, лащш ооцайн амд оцбйтйн тм дъшеод щм дщйоещ бщийфеъ дфд мдчмд тм зесш резеъ еъсойрйн бзмм дфд бчшб земй сшип сефрй.
https://pubmed.ncbi.nlm.nih.gov/33586003/
бозчш ъцфйъй шишесфчийбй (2018) ртшлд дщееад бйп щйтеш ддйщшгеъ щм земй сшип, ащш чйбме ийфем чербрцйерамй бмбг, мтеоъ земйн щчйбме вн ийфем бшфеад ощмйод. бресу, рбгчд ддйтреъ мийфем еоафййрй дземйн. бдъбсс тм оавш дшйщен дмаеой даошйчай мсшип, бозчш рлмме дръерйн щм л-1,901,815 земйн щаебзре тн сшип щг щайре вшешъй, сшип тшоерйъ, сшип шйаеъ ае сшип чемешчимй бйп дщрйн 2004-2013. обйп лмм дземйн, 258 бмбг чйбме вн ийфем бшфеад ощмйод емдн деъаод чбецъ бйчешъ щм 1,032 земйн бтмй оафййрйн геойн щчйбме ийфем чербрцйерамй бмбг. одръерйн темд лй бщъй дчбецеъ ощк джоп бйп дабзрд мъзймъ дийфем ма дйд щерд баефп ощотеъй, аемн оиефмйн щбзше мфреъ мшфеад ощмйод дйе бтмй риййд вбедд йеъш мсшб мрйъез (7% мтеоъ 0.1%), млйоеъшфйд (34.1% мтеоъ 3.2%), мшгйеъшфйд (53% мтеоъ 2.3%) емийфемйн дешоермййн (33.7% мтеоъ 2.8%). бресу, ийфем бшфеад ощмйод дйд чщеш бщйтеш дйщшгеъ мазш 5 щрйн роек йеъш (82.2% мтеоъ 86.6%) ебсйлеп вбед фй 2 мъоеъд. дзечшйн ослойн лй дооцайн оцбйтйн тм лк щдсйлеп доевбш мъоеъд бчшб земй сшип дферйн мшфеад ощмйод дйре ллм дршад лъецад ориййд вбедд йеъш мсшб мийфем дчербрцйерамй.
https://www.ncbi.nlm.nih.gov/pubmed/30027204
босок (2018) щфешсн оитн дзбшд дайшефайъ маерчемевйд чмйрйъ (ESMO), оецвеъ ддрзйеъ мийфем бщмщем бчшб обевшйн земй сшип. босок офешиъ ддвгшд дчмйрйъ мщмщем, двешойн бдчщш мземй сшип, асишивйд мъщаем емабзеп едбгйчеъ дргшщеъ. бдощк, грйн дзечшйн бщмщем лъсойп дчщеш бозмъ дсшип едийфем бд, лемм щмщем лъвебд мийфемй лйоеъшфйд щерйн еъшефеъ азшеъ, елп лъвебд мгйлей зйсерй емийфем дешоермй. бресу, оецвйн вешойн ресфйн мщмщем, лемм щйрей бфмешъ дотй, джрд аришмйъ ерйъезйн щерйн бгшлй дтйлем. бдощк досок оецвъ дасишивйд дийфемйъ дшфеайъ бщмщем елп ийфемйн орйтъййн. бресу, офешиъ асишивййъ дийфем бземйн сефрййн щайрн очбмйн ийфем аерчемевй.
бсйен дсчйшд оъййзсйн дзечшйн масишивйеъ ийфем ъжеръйеъ еоцййрйн лй айп домцд мбцт щйреййн ъжеръййн баефп орйтъй ама бъвебд мдефтд щм щмщем. дн осбйшйн лй огебш бдомцеъ лммйеъ бмбг, щлп ошбйъ дозчшйн ртшле бчшб оиефмйн тн ъсоеръ дотй дшвйщ ема бчшб оиефмйн аерчемевййн. мдмп ддомцеъ дофешиеъ:
двбмд ае дйортеъ оцшйлъ ъбмйрйн лое ц'ймй еощчаеъ лое чфд еамледем, ащш тмемйн мдвбйш аъ дъсойрйн.
дфзъъ дцшйлд щм сйбйн бмъй осйсйн.
ийфемй лйоеъшфйд тмемйн мвшен май сбймеъ ммчиеж емлп оеомх мдйорт озмб рйвш еоецшй змб, омбг йевеши евбйреъ чщеъ. тн жаъ, вн боцбйн щм ай сбймеъ ммчиеж йщрд сбймеъ ммчиеж бшод роелд еайп ъойлд мдфсчъ дщйоещ бъшефеъ долймеъ мчиеж.
мошеъ щроцад ъойлд бчшб оиефмйн тн озмеъ отй гмчъйеъ еъсоеръ дотй дшвйщ, айп осфйч тгейеъ мъшеод щм гйаиъ гмъ FODMAPs бчшб оиефмйн аерчемевййн.
айп домцд мщйоещ бъесфй вмеиойп еаеовд 3, щлп йтймеън ма делзд боцбйн щм щмщем тм шчт ийфемй лйоеъшфйд.
дщйоещ бфшебйеийчд дйре щрей бозмечъ, щлп фшебйеийчд тщейд мъшен мдврд тм шйшйъ дотй емдфзъъ дъсойрйн, ак тмемд мдвбйш аъ дсйлеп мжйдеойн бчшб оиефмйн тн гйлей зйсерй.
бдъбсс тм двйщд щм шфеад оеъаоъ айщйъ, дзечшйн чешайн мжйдей оечгн щм оиефмйн дроцайн бсйлеп оевбш мщмщем емдъайн мдн ълрйъ ийфем мдфзъъ зеошъ еощк дъсойрйн.
https://academic.oup.com/annonc/article/29/Supplement_4/iv126/5041967
бозчш ачшай обечш (2018) детшлд ддщфтд щм CALM (ае бщое дома: Managing Cancer And Living Meaningfully) - щйиъ дътшбеъ фсйлеъшфйъ згщд еодйшд щоишъд мифм еморет гйлаеп еоцечд дчщешд мсеу дзййн бчшб оиефмйн тн озмъ сшип оъчгоъ. ъек дъбссеъ тм вйщеъ фсйлемевйеъ щереъ (двйщд ддъййзсеъйъ, ъйаешйъ ддйчщшеъ едвйщд дачжйсирцйамйсийъ), дщйид щод гвщ тм осфш ъзеойн: рйдем дъсойрйн еъчщешъ тн дцееъ дшфеай, щйреййн фрйоййн едчщш тн дчшебйн, ъзещъ шеезд шезрйъ еъзещъ ощотеъ еоишд, едъййзсеъ мъоеъд емгавеъ бревт мтъйг.
бозчш рлмме 305 оиефмйн, ащш вейсе мозчш бйп дщрйн 2012 м-2016 еземче ачшайъ мщъй чбецеъ: чбецд азъ чйбмд ийфем CALM (л-3 офвщйн мфзеъ) бочбйм мийфем дсиргший дшфеай едчбецд дщрййд чйбмд аъ дийфем дсиргший бмбг. дозчш ашк 6 зегщйн. зеошъ дгйлаеп детшлд баоцтеъ догг PHQ-9 бе рйъп цйеп бйп 0 м-27, лащш цйеп биеез щм 5-9 обиа ъсойрй гйлаеп чмйн, 10-14 гйлаеп чм, 15-19 гйлаеп бшоъ зеошд бйрерйъ ецйеп отм 20 обиа гйлаеп зоеш. роца лй дощъъфйн бчбецъ д-CALM гйеезе тм шоъ зеошд роелд йеъш щм ъсойрй гйлаеп бдщееад мчбецъ дийфем дсиргший бмбг мазш 3 зегщйн емазш 6 зегщйн. мдмп фйшеи дцйерйн дооецтйн богг PHQ-9:
| |
CALM
|
ийфем сиргший
|
дфшщ бйп дчбецеъ
|
|
ъзймъ дозчш
|
7.45
|
7.41
|
|
|
мазш 3 зегщйн
|
5.97
|
7.01
|
1.09, p=0.04
|
|
мазш 6 зегщйн
|
5.35
|
6.64
|
1.29, p=0.02
|
лое лп, бсйен дозчш рцфъд длрд ощотеъйъ йеъш мсеу дзййн бчшб доиефмйн бчбецъ д-CALM. ма геезе дщфтеъ щмймйеъ дчщешеъ мдътшбеъ. дзечшйн ослойн лй ооцайн амд оцбйтйн тм дйтймеъ щм щйиъ CALM мдчмд тм гйлаеп бчшб оиефмйн тн озмъ сшип оъчгоъ еоеъаоъ маъвшйн айън доиефмйн оъоеггйн.
https://www.ncbi.nlm.nih.gov/pubmed/29958037
озчш шзб дйчу (ребобш 2015) бе рбгч дчщш бйп ожереъ ешлйбйн ъжеръййн щерйн мбйп дсйлеп мсшип щзмеъ афйъмйамй.
озчш обечш вгем щртшк байшефд бе рбгч дчщш бйп ъжерд есшип (EPIC) лмм 1,095 ощъъфйн щоймае щамерй ъжерд мфйдн детшлд дцшйлд щм 28 ожереъ ечбецеъ ожеп е-29 шлйбйн ъжеръййн.
дзечшйн бзше 4 шлйбйн щдйе чщешйн баефп оебдч бсйлеп мсшип щзмеъ ебзре чщшйн амд бозчш течбд ресу (NLCS), ащш лмм 383 ощъъфйн.
лемсишем, щеоп шб бмъй шеей, щеоп шеей ебрреъ дйе 4 дшлйбйн щжеде бозчш дшащеп, аемн бозчш дщрй ма роца чщш оебдч бйрйдн мбйп дсйлеп мсшип дщзмеъ.
тн жаъ, боид-армйжд щлммд ръерйн ощрй дозчшйн роца лй цшйлд вбедд щм щеоп шеей, мтеоъ роелд, дййъд омеед бсйлеп вбед бл-20% мсшип дщзмеъ.
http://www.ncbi.nlm.nih.gov/pubmed/2660793
озчш (оай 2016) дбегч аъ дчщш бйп осфш гфесй ъжерд мбйп дсйлеп мсшип чемешчимй. дзечшйн оцййрйн лй ъжерд еаешз зййн одеейн вешой сйлеп бдъфъзеъ сшип чемешчимй аемн орвреп ддщфтд айре бшеш мвошй.
босвшъ дозчш щртшк бйшгп, дзечшйн асфе ръерйн мвбй гфес дъжерд щм 220 земй сшип чемешчимй ещм 281 ощъъфйн бшйайн бтмй оафййрйн сецйе-гоевшфййн геойн.
орйъез лмм дръерйн дзечшйн жйде щмещд гфесй ъжерд тйчшййн: "ъжерд бшйад" (доаефййръ бтйчш бцшйлъ фйшеъ ейшчеъ), "ъжерд тъйшъ селш еъд" (доаефййръ бтйчш бцшйлъ селш еъд) е"ъжерд отшбйъ" (доаефййръ бтйчш бцшйлъ бщш аген, гврйн, бйцйн егвйн).
роца лй гфес щм "ъжерд отшбйъ" дйд чщеш бсйлеп вбед бл-88% мдъфъзеъ сшип чемешчимй, лащш бщрй дгфесйн дазшйн жедд сйлеп оефзъ щайре оебдч сиийсийъ.
http://www.ncbi.nlm.nih.gov/pubmed/27206698
озчш (фбшеаш 2015) дбезп аъ ойгъ дщйоещ едаоереъ бйзс мшфеад ощмйод еайрившийбйъ бчшб дозмйойн омйофеод щайрд дегв'чйп. дозчш обесс тм ръерйн щрасфе ощамерйн щоемае тм йгй 719 оиефмйн 3 щрйн мазш дабзрд.
89% одощйбйн гйеезе лй тще щйоещ ай фтн бшфеад ощмйод еайрившийбйъ, лащш 78% одощйбйн гйеезе тм риймъ ейиойрйн, 54% тм ийфемйн амишрийбййн мсшип е-45% тм щйоещ бцозй ошфа.
роца лй рщйн рие йеъш мтщеъ щйоещ бшфеад ощмйод баефп лммй еоиефмйн обевшйн отм вйм 60 рие йеъш мчзъ ейиойрйн ефзеъ цозй ошфа.
мвбй даоереъ бйзс мщйоещ бшфеад ощмйод, 20% обйп дощъощйн даойре щдщйоещ бшфеад ощмйод осййт мдзмод, 17% даойре щочм тм дъсойрйн, 17% даойре щосфч ъзещъ щмйид, 15% даойре щъеок бийфемйн дазшйн, 15% даойре щовбйш аъ дфтймеъ дзйсерйъ, 4% даойре щошфа сшип е-5% даойре щоерт дъфщиеъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/24745936
бозчш ачшай обечш фмсбе (оай 2017), щртшк тм йгй зечшйн йщшамййн, рбгчд ддщфтд щм ийфем ъшефъй сфцйфй мфрй рйъез тм оггйн сширййн мазш дрйъез бчшб земеъ сшип дщг. дзечшйн осбйшйн лй ооцайн фшд-чмйрййн чегойн оцбйтйн тм лк щмфрй рйъез йщрд тмййд бщзшеш чилемаойрйн (оемйлйн тцбййн лвеп агшрмйп ефшесивмргйрйн), ащш тмемйн мдвбйш ъдмйлйн вшешъййн емдфзйъ аъ ощк ддйщшгеъ.
бозчш дрелзй рлмме 38 оиефмеъ тн сшип щг бщмб оечгн, ащш риме аъ дийфем дъшефъй мощк 11 йен, дзм о-5 йойн мфрй дрйъез. дийфем лмм щймеб щм ъшефд оощфзъ зесой биа (Propranolol) еъшефд ревгъ-гмчъ (etodolac).
роца лй дийфем дъшефъй рсбм дйиб ещйтеш ъефтеъ дмееай дйд геод мчбецъ дфмсбе. дзечшйн ошайн лйцг дийфем дъшефъй ъшн мдфзъъ оггйн дчщешйн бдъфъзеъ ъдмйлйн вшешъййн елп мщйфеш дфтймеъ дзйсерйъ емдфзъъ оггйн гмчъййн. дн ослойн лй ъецаеъ дозчш оцбйтеъ тм лк щзсйоъ дешоерй дмзх едфтймеъ дгмчъйъ мфрй рйъез тщейд мдйеъ асишивйд йтймд мтйлеб осмемйн дчщешйн бдъфъзеъ вшешеъ едйщреъ дозмд бчшб земеъ сшип дщг бщмбйн оечгойн.
https://www.ncbi.nlm.nih.gov/pubmed/28490464
бозчш ъцфйъй (2017) рбгч дчщш бйп ийфем бмтгй бшфеад амишрийбйъ бчшб земй сшип мбйп щйтеш ддйщшгеъ. бозчш рлмме 280 земй сшип - щг, тшоерйъ, шйаеъ ечемешчимй - щайре вшешъй, щма чйбме ийфем арий-сширй чербрцйерамй (лгевоъ лйоеъшфйд, шгйеъшфйд, рйъез е/ае ийфем дешоермй), ама ийфем амишрийбй (девгш бозчш лийфем азш ма оелз, дрйъп тм йгй оифм щайре шефа).
чбецъ ддщееад лммд 560 земй сшип бтмй оафййрйн геойн, щчйбме аъ дийфем дчербрцйерамй. дзечшйн оцййрйн лй сшип щг ае шйаеъ, оцб сецйеачереой вбед йеъш, сшип бщмб 2 ае 3 ешод роелд щм ъзмеад рмеейъ дйе двешойн дчщешйн брийд вбедд йеъш мбзеш бщйоещ бшфеад амишрийбйъ. бдщееад бйп чбецеъ дийфем роца лй баефп лммй щйоещ бшфеад амишрийбйъ дйд чщеш бсйлеп вбед фй 2.5 мъоеъд биеез щм 5 щрйн. бзмечд мфй сев дсшип, дсйлеп дйд вбед фй 5.68 бземеъ сшип дщг, фй 2.17 бземй сшип шйаеъ ефй 4.57 бземй сшип чемешчимй. тбеш земй сшип тшоерйъ дсйлеп дйд вбед б-68% аемн ддбгм ма дйд оебдч сиийсийъ. дзечшйн ослойн лй аеорн огебш босфш очшйн чип, ак щйоещ бмтгй бшфеад амишрийбйъ, мийфем бозмъ сшип дрйъръ мийфем чербрцйерамй, чщеш бсйлеп вбед йеъш мъоеъд.
дтшъ дотшлъ: мгтъйре йщрп осфш бтйеъ бозчш жд -
- деа обцт дщееад бйп чбецеъ бтмеъ вегм щерд, бйзс 1:2, мошеъ щжде оцб очебм бтемн дозчш.
- мцтшйре айп фйшеи щм севй дийфемйн дамишрийбйн щрбгче етемд дъдйд дан рйъп мдщееъ бйп ийфемйн щделзе лощфшйн дйщшгеъ сшип мбйп ийфемйн щма делзе лламд ае бйп ийфем бцозй ошфа, мощм, мийфемйн шезрййн щерйн.
- жде озчш ъцфйъй еайп дъййзсеъ марщйн щдъзйме шфеад амишрийбйъ емазш олп чйбме ийфем шфеай ае мощърйн оътшбйн азшйн.
- дозчш лмм ма оъййзс мшфеад айрившийбйъ (ощембъ) щдйа дщмиъ лйен ббъй дземйн двгемйн бтемн.
https://academic.oup.com/jnci/article/110/1/djx145/4064136/Use-of-Alternative-Medicine-for-Cancer-and-Its
бдъбсс тм ръерйн оозчш течбд (2021) вгем щртшк байшефд дтесч бчщш бйп ъжерд, аешз зййн евешойн сбйбъййн ебйп дсйлеп мдъфъзеъ сшип (EPIC), дзечшйн дтшйле аъ дъфчйг щм вешой ъжерд еаешз зййн бдъййзс мъоеъд осшип.
бдъбсс тм дооцайн о-45 фшсеойн дзечшйн бзре аъ дчщшйн бйп вешой дзщйфд ебйп дсйлеп мъоеъд осшип баефп лммй емфй сев дсшип. вешой дзщйфд рбгче бзмечд машбт чбецеъ:
- ожереъ: фйшеъ ейшчеъ, йшчеъ ишййн, фйшеъ ощеМошйн, бйцйн, чирйеъ, гвйн, щоп жйъ, оецшй змб, бщш аген еотебг еощчаеъ ооеъчйн.
- шлйбйн ъжеръййн: сйбйн, зеоцеъ щеоп, ейиойп C, ейиойп K, ейиойп D, сйгп, овржйен, фмбереайгйн, мйвррйн, ъесфй ойршмйн еейиойрйн.
- оггй ъжерд еаешз зййн: оггйн щерйн лвеп гйаид йн-ъйлерйъ, гйаид гмчъйъ, фмйиъ вжй зоод щм дцшйлд дъжеръйъ етег.
- вешойн ресфйн: фтймеъ вефрйъ, цшйлъ амледем, BMI едщорд бирйъ.
мдмп сйлен дооцайн дтйчшййн:
- двешойн дъжеръййн щдйе чщешйн бсйлеп оефзъ мъоеъд осшип лмме цшйлъ йшчеъ ишййн, цшйлъ сйбйн, гйаид йн-ъйлерйъ егфесй ъжерд ресфйн лвеп цшйлд роелд щм бщш ае ибтереъ ецозереъ, шод вбедд щм ейиойрйн (лемм ейиойп C, ейиойп D еейиойп K2), ецшйлъ чирйеъ.
- фтймеъ вефрйъ едчфгд тм аешз зййн бшйа дйе чщешйн бсйлеп оефзъ мъоеъд осшип.
- двешойн дъжеръййн щдйе чщешйн бсйлеп двбед бйеъш мъоеъд осшип лмме айлеъ ъжерд роелд, цшйлъ амледем еощчаеъ оъечйн ебойгд фзеъд олк цшйлд щм зеоцеъ щеоп осейоеъ (лвеп зеоцд айчесреайъ бдчщш мсшип дтшоерйъ).
- тегу ощчм ещореъ дйе чщешйн бсйлеп оевбш мъоеъд осшип.
дзечшйн ослойн лй дръерйн оозчш EPIC оафщшйн мждеъ одн двешойн дъжеръййн дошлжййн ащш тщеййн мсййт борйтъ дъоеъд осшип.
https://pubmed.ncbi.nlm.nih.gov/34959845/
лзмч оозчш течбд вгем (аевеси 2017), дтесч ббшйаеъ дайщд, бозчш дрелзй рбгч дчщш бйп шоъ дцфйфеъ даршвийъ щм дъжерд мбйп дсйлеп мсшип дчщеш бщореъ.
дцфйфеъ даршвийъ щм ожеп дйрд дйзс бйп дтшк дчмешй мбйп ощчм дожеп еодеед огг майлеъ дъжерд. мгевоа, бщжйу ишй 46 чмешйеъ мтеоъ 240 чмешйеъ бщжйу ойебщ (тбеш 100 вшн), олап щбаефп бмъй ъмей блоеъ дрцшлъ дцфйфеъ даршвийъ щм щжйу ойебщ вбедд баефп рйлш ожаъ щм щжйу ишй.
бозчш рлмме 92,295 рщйн бвймай 50-79, лащш бъчефъ отчб ооецтъ щм 14.6 щрйн аебзре 9,565 очшйн щм сшип дчщеш бщореъ (щг, чемешчимй, щзмеъ, шзн, лмйеъ, лйс ошд, еещи ембмб).
одръерйн темд лй рщйн щцшле ъжерд бтмъ цфйфеъ аршвийъ вбедд, бдщееад мроелд, дйе бтмеъ BMI едйчу оеърййн вбедйн йеъш. баефп лммй, роца лй цфйфеъ аршвийъ вбедд дййъд чщешд бсйлеп вбед б-10% мсшип дчщеш бщореъ олм сев. брйъез щм ъъй чбецеъ, роца лй рщйн бощчм ъчйп, щцшле ъжерд бтмъ цфйфеъ аршвийъ вбедд йеъш дйе бсйлеп вбед б-10-18% мсшип дчщеш бщореъ, бдщееад мрщйн бощчм ъчйп тн ъжерд бтмъ цфйфеъ аршвийъ роелд. ма роцае чщшйн оебдчйн бдъййзс мрщйн тн тегу ощчм ае щореъ.
дзечшйн ослойн лй ъжерд бтмъ цфйфеъ аршвийъ вбедд тмемд мъшен мсйлеп мдъфъзеъ сшип дчщеш бщореъ, бойезг бчшб рщйн бощчм ъчйп лк щщйфеш айлеъ дъжерд тщейд мъшен мдфзъъ дсйлеп мсшип бчшб рщйн мазш вйм дотбш.
https://www.ncbi.nlm.nih.gov/pubmed/28826845
лзмч оозчш дбшйаеъ доъчййн бсйрвфеш (Singapore Chinese Health Study) рбгч дчщш бйп фтймеъ вефрйъ мбйп дсйлеп мсшип чемешчимй. дозчш дйре озчш течбд вгем, обесс аелмесййд (ребобш 2017), длемм 63,257 обевшйн ооеца сйрй, щдйе бвймай 45-74 бъзймъ дозчш бйп дщрйн 1993-1998. дзечшйн осбйшйн лй бсйрвфеш змд тмййд бщлйзеъ земй сшип чемешчимй б-40 дщрйн дазшереъ, лащш тгейеъ оозчшйн щртшле байшефд еашд"б ошайн лй шод роелд щм фтймеъ вефрйъ еаешз зййн йещбрй одеейн вешн сйлеп мсшип чемешчимй. бъзймъ дозчш, дощъъфйн гйеезе аегеъ дфтймеъ двефрйъ еощк жоп дйщйбд бщрд дазшерд.
лащш ботчб щртшк тг мщръ 2014 аебзре 1,994 очшйн щм сшип чемешчимй. орйъез дръерйн темд лй бдщееад мощъъфйн щма бйцте лмм фтймеъ вефрйъ, ощъъфйн щгйеезе тм лм фтймеъ бтцйоеъ вбедд роцае бсйлеп роек б-15% мсшип чемешчимй. фтймеъ бтцйоеъ бйрерйъ дййъд чщешд бйшйгд бсйлеп мсшип чемешчимй - шч тбеш ощъъфйн щгйеезе тм цфййд ооещлъ бимеейжйд (отм 3 щтеъ мйен).
https://www.ncbi.nlm.nih.gov/pubmed/28542077
бщрй оаошйн, (2019) щфешсое тм йгй зечшйн чргййн, офешийн ооцай счш, щртшк бчшб шефайн риешефъййн дзбшйн башвеп Oncology Association of Naturopathic Physicians, бревт масишивйеъ ийфем риешефъйеъ бщъй чбецеъ щм земйн аерчемевййн. боаош дшащеп оецвйн дооцайн бдъййзс мийфем бсшип бчшб ймгйн ебоаош дщрй бдъййзс мийфем бземйн тн вйгемйн ббйъ дзжд едшйаеъ.
дийфем бсшип бчшб ймгйн: босвшъ дсчш дощйбйн дъбчще мфши аъ ддомцеъ башбтд ъзеойн: оецшйн ибтййн, ъжерд, ийфем вефрй еъойлд оримйъ ешвщйъ. дъчбме 99 отрйн, доаефййрйн бщереъ вгемд бдъййзс мрйсйеп дчмйрй ебйлемъ дийфем бймгйн тн сшип.
- ошбйъ дощйбйн (52.5%) бзше ма мифм бймгйн земй сшип, ецййре лй дсйбеъ дтйчшйеъ млк дйе дтгш гшйщд цйбешйъ, овбмеъ оесгйеъ ае чмйрйеъ, есйбеъ айщйеъ ае резеъ.
- тщшъ доецшйн дибтййн дщлйзйн бйеъш, щцййре дощйбйн лтщеййн мъшен мийфем дйе: щоп гвйн, ейиойп D, фшебйеийчд, омиерйп, ейиойп C, ашрйчд деоаефийъ, лешлен, вмеиойп, асишвмес ефишййъ чешйемес.
- зощ ддомцеъ дъжеръйеъ дщлйзеъ бйеъш дйе: гйаид арий-гмчъйъ, двбмъ оецшй дзмб, гйаид йн-ъйлерйъ, двбмъ двмеип егйаид чиеврйъ.
- зощ ддомцеъ дщлйзеъ бйеъш мийфем вефрй дйе: фтймеъ вефрйъ, гйчеш, рчегеъ мзйцд, ийфем чшрйе счшам ейевд.
- зощ ддомцеъ дщлйзеъ бйеъш мийфем оримй ешвщй дйе: огйицйд, ийфем баеореъ, дфзъъ оъзйн баоцтеъ оййргфемрс, ийфем боежйчд егойеп оегшк.
дзечшйн ослойн лй счш жд огвйщ овееп дътшбейеъ риешефъйеъ бтмеъ феирцйам мийфем бймгйн земй сшип, еосфч бсйс мдощк дозчш бъзен.
дийфем бвйгемй бйъ дзжд едшйаеъ: босвшъ дсчш дощйбйн дъбчще мфши аъ ддомцеъ мфрй еазшй дийфем дрйъезй башбтд ъзеойн: оецшйн ибтййн, ъжерд, ийфем вефрй еъойлд оримйъ ешвщйъ. лое лп, дъбчще мцййп одп доишеъ дийфемйеъ едъвебеъ ддггйеъ дафщшйеъ бйп дийфем дайрившийбй мийфем дчербрцйерамй. дъчбме 44 отрйн (щйтеш ъвебд щм 12.5%), лемн сййое аъ мйоегйдн боесг ачгой баошйчд дцферйъ еошбйън дйе збшйн б-American Board of Naturopathic Oncology.
дощйбйн домйце баефп оебдч тм йеъш дътшбейеъ мазш рйъез бдщееад мдътшбейеъ ишен-рйъезйеъ.
ддътшбейеъ дщлйзеъ бйеъш лмме: фчийп офйшеъ дгш, ашрйчд, аеовд 3, ейиойп D, фшебйеийчд, фтймеъ вефрйъ, гйчеш, огйицйд, дфзъъ сишс, гйаид бтмъ айргчс вмйой роек егйаид йн-ъйлерйъ.
тщейеъ мдйеъ овееп ъвебеъ дггйеъ тн дийфем дчербрцйерамй - длемм рйъез, лйоеъшфйд ешгйеъшфйд - лъмеъ бсев ддътшбеъ ебоецшйн дибтййн бдн ртщд щйоещ.
дзечшйн ослойн лй ооцайн амд огвйщйн дътшбейеъ риешефъйеъ, бдп ртщд щйоещ босвшъ дийфем бземйн тн вйгемй бйъ дзжд едшйаеъ, елйцг ддътшбеъ дайрившийбйъ оеъаоъ мщмб дийфем дчербрцйерамй.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6769230/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142094/
бозчш отбгд (аечиебш 2017) фешх гшк, щртшк тм оегм щм щошйн, ошайн дзечшйн оде дорвреп дазшай млк щцшйлъ селш вбедд овбйшд цойзъ вйгемйн сширййн (ъефтъ ешбешв). ъефтъ ешбешв дйрд ъефтд бйелйойъ, щбд ъдмйк двмйчемйжд бъайн сширййн рощк вн бсбйбд шеейд бзоцп, бщерд одоибемйжн щм ъайн швймйн, бдн чцб двмйчемйжд йешг брелзеъ шоеъ зоцп вбедеъ. дзечшйн осбйшйн лй ъай щошйн олймйн змберйн оощфзъ Ras, бгеод мъайн сширййн, еблк оафщшйн мзчеш аъ дчщш бйп дфтймеъ щм змберйн амд, дотеггйн змечъ ъайн сширййн, мбйп дтмййд боибемйжн щм вмечиж. дн ошайн лй ъецш дфйшеч щм вмечеж, Fructose 1,6-bisphosphate, овбйш аъ дфтймеъ щм змберйн амд елъецад олк йщрд тмййд бчцб дзмечд щм ъайн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/29030545
бсчйшд (йерй 2016) ослойн дзечшйн аъ дтгейеъ дчййоеъ бревт мщйреййн дафйвриййн дчщешйн бъдмйлйн сширййн ебъдмйлй дджгчреъ, лемм дцвъ ддщфтд дойийбд щм ийфемйн ъжеръййн бгвщ тм двбмд чмешйъ - ащш тщейд мдвбйш аъ йтймеъ дийфем дарий-сширй емтлб ъдмйлй джгчреъ - елп ддщфтд щм шлйбйн цозййн щерйн лвеп EGCG, семфешфп, лешлеойп, шжбшишем, в'рйсиайп, чеешцийп ечилйрйн.
https://www.ncbi.nlm.nih.gov/pubmed/26667209
бозчш, добесс тм ръерйн ъцфйъййн (аечиебш 2017), дзечшйн дтшйле оде щйтеш еосфш очшй дсшип баесишмйд бщръ 2013 аеън рйъп мййзс м-20 вешой аешз зййн дрйърйн мщйрей. дзечшйн чйбце аъ двешойн м-8 чбецеъ: ибч (тйщеп етйщеп фасйбй), ъжерд (цшйлд роелд щм фйшеъ, йшчеъ есйбйн ецшйлд вбедд щм бщш аген еотебг), дщорд, цшйлъ амледем, дтгш фтймеъ вефрйъ, зщйфд мчшйръ дщощ, жйдеойн евешойн дчщешйн ботшлъ дшбййд (дтгш дрчд, щйоещ бийфем дешоермй змйфй ериймъ вмемеъ морйтъ дшйеп).
дзечшйн тще щйоещ боегм сиийсий, ащш лемм ръерйн мвбй ойгъ дзщйфд щм даелмесййд мвешойн еамд еръерйн мвбй дсйлеп дйзсй щм лм вешн. тм сок ръерйн амд, ддтшлд дйа щрйъп мййзс л-38% олмм очшй дъоеъд осшип ел-33% олмм очшй дсшип баесишмйд бщръ 2013 мвешой аешз зййн амд. двешн доебйм мсшип дйд тйщеп ибч (23% оочшй дъоеъд е-13% олмм дочшйн), лащш двешойн дтйчшййн дресфйн дйе вешойн ъжеръййн (5% / 5%), дщорд (5% / 4%) ежйдеойн (5% / 3%). бресу, дзечшйн отшйлйн лй севй дсшип бтмй феирцйам дорйтд двбед бйеъш дйрн сшип шйаеъ, чемешчимй еомреод. тм фй ръерйн амд, л-16,700 очшй ъоеъд осшип ел-41,200 очшй сшип рйърйн морйтд баесишмйд огй щрд баоцтеъ дчфгд тм зщйфд м-20 вешой аешз дзййн бдъан мдомцеъ дчййоеъ тм оръ мцоцн аъ дсйлеп мсшип.
https://www.ncbi.nlm.nih.gov/pubmed/28983918
бдъбсс тм дръерйн ощрй озчшй течбд вгемйн (йреаш 2018), бозчш дрелзй рбгч дчщш бйп ъжерд фше-гмчъйъ мбйп дсйлеп мсшип чемешчимй. босвшъ дозчш ртшк отчб щм л-26 щрйн азш л-120,000 ощъъфйн. тм бсйс щамерй ъжерд щдощъъфйн оймае лм 4 щрйн, дзечшйн бгче дан цшйлъ ъжерд фше-гмчъйъ, щдетшлд тм фй догг EDIP (ебщое дома: empirical dietary inflammatory pattern), дййъд чщешд бсйлеп оевбш мсшип чемешчимй. бъчефъ дотчб ъетге 2,699 очшйн щм сшип чемешчимй.
бчшб дощъъфйн тн цйерй EDIP дроелйн бйеъш роца лй щйтеш очшй дсшип дчемешчимй (млм 100,000 щреъ агн) дйд 113 мвбшйн е-80 мрщйн, еайме бчшб дощъъфйн тн дцйерйн двбедйн бйеъш щйтеш дочшйн дйд 151 мвбшйн е-92 мрщйн. лмеош, осфш очшй дсшип дчмешчимй дйд вбед б-38 еб-12 очшйн, бчшб вбшйн ерщйн бдъаод, щцшле шод вбедд, бдщееад мроелд, щм ъжерд фше-гмчъйъ. ръерйн амд обиайн сйлеп вбед б-44% тбеш вбшйн еб-22% тбеш рщйн (сйлеп вбед б-32% тбеш вбшйн ерщйн йзг).
брйъез мфй ъъй-чбецеъ, роца лй чщшйн амд дйе оещфтйн оцшйлъ амледем еоощчм, лк щдсйлеп дйд вбед йеъш бчшб ощъъфйн щайрн цешлйн амледем, бчшб вбшйн тн тегу ощчм ае щореъ ебчшб рщйн бощчм роек. лмеош, дътшбейеъ мщйфеш гфесйн щм ъжерд фше-гмчъйъ морйтъ сшип чемешчимй тщейеъ мдйеъ дйтймеъ бйеъш бчбецеъ амд. бдъййзс мцшйлъ амледем, дзечшйн оцййрйн лй баефп лммй шоъ цшйлд вбедд щм амледем чщешд бсйлеп оевбш мсшип чемешчимй, аемн рйлш лй дорвреп бе амледем ощфйт тм дъфъзеъ сшип чемешчимй айре чщеш бъдмйлйн гмчъййн. дзечшйн оцйтйн лй тм оръ мдфзйъ аъ ойгъ дгмчъйеъ ботй оеомх млмем бъжерд тмйн йшечйн, йшчеъ лъеойн-цдебйн, чфд еъд емдотйи ббщш аген еотебг, гврйн щайрн омайн еощчаеъ ооеъчйн.
https://www.ncbi.nlm.nih.gov/pubmed/29346484
бозчш, щртшк бчшб тлбшйн (фбшеаш 2018), роца лй мзййгчйн оджп Staphylococcus epidermidis доцеййн бтеш дщфтд овйрд офрй дъфъзеъ сшип дтеш.
https://www.ncbi.nlm.nih.gov/pubmed/29507878
бозчш ачшай обечш фъез (фбшеаш 2018) детшлд дйтймеъ щм фмсбе лийфем бземщд бчшб оиефмйн дозмйойн осшип. бозчш рлмме 74 оиефмйн, щдщмйое аъ дийфем ревг дсшип 6 зегщйн тг 10 щрйн мфрй ъзймъ дозчш егйеезе тм шод бйрерйъ мфзеъ щм земщд (цйеп вбед о-4 бсемн щм 0-10). дощъъфйн земче ачшайъ мчбмъ фмсбе ае мдощк дийфем дшвйм щмдн мощк 21 йен. дощъъфйн бчбецъ дфмсбе, щчйбме дгшлд едйе оегтйн млк щогебш блоесеъ фмсбе (щдлйме microcrystalline cellulose), дерзе мйием 2 лоесеъ фтоййн бйен.
роца лй бдщееад мчбецъ дийфем дшвйм, бчшб ощъъфйн щриме фмсбе рцфд щйфеш вбед б-29% богг FSI (ебщое дома: Fatigue Symptom Inventory) мдтшлъ ойгъ дземщд, евбед б-39% богг MFSI (ебщое дома: Multidimensional Fatigue Symptom Inventory) дойетг мдтшйк аъ дойгд бд дземщд февтъ байлеъ дзййн щм доиефм.
бсйен ъчефъ дозчш, дзечшйн бйцте ъчефъ отчб щм 21 йойн ресфйн, бдн дощъъфйн бчбецъ дийфем дшвйм йлме мбзеш мчбм фмсбе, лащш дооцайн щдъчбме бъчефъ дотчб дресфъ дйе геойн тн щйфеш щм 23% е-35% бщрй доггйн бдъаод. дзечшйн ослойн лй дийфем бфмсбе роца йтйм мдчмд тм ъсойрй земщд емщйфеш айлеъ дзййн щм оиефмйн дозмйойн осшип.
https://www.ncbi.nlm.nih.gov/pubmed/29426869
боаош (2017) оцйтйн дзечшйн освшъ мщймеб щм аерчемевйд айрившийбйъ лзмч одийфем бозмъ дсшип мщйфеш айлеъ дзййн емийфем бъсойрйн.
боаош оецвъ двйщд дотшбйъ, мтеоъ двйщд досешъйъ, мдбръ озмъ дсшип еасишивйеъ айрившийбйеъ мийфем, лащш двйщд дорзд дйа дщвъ айжеп. бдъййзс мъжерд, оегвщъ дзщйбеъ щм ъжерд добессъ тм дцеоз едфзъъ дцшйлд щм змбеп одзй едъфчйг дошлжй щм фмешъ дотй. бдощк офеши дийфем дайрившийбй бъефтеъ дмееай дщлйзеъ щм дийфем дчербрцйерамй, лвеп бзймеъ, тцйшеъ, зшгд етег, ъек дгвщъ дщйоещ бчрбйреайгйн. бресу, йщрд дъййзсеъ мийфем бдеоаефъйд, шфеаъ цозйн сйрйъ, ц'й-черв, щдййд бибт, ийфемй веу-рфщ, оййргфемрс ейевд.
дзечшйн ослойн лй бочбйм мийфем дчербрцйерамй, мземй сшип йщрд афщшеъ мщмб ийфемйн айрившийбййн тм оръ мщфш аъ оцбн двефрй, дшвщй, дрфщй едшезрй.
https://www.ncbi.nlm.nih.gov/pubmed/28501232
бозчш течбд фшесфчийбй рбгч дан дчфгд тм ддомцеъ щм авегъ дсшип даошйчайъ бреща ъжерд рлерд ефтймеъ вефрйъ (ACS guidelines) чщешд бощк дйщшгеъ ашек йеъш бчшб оиефмйн дозмйойн осшип дотй двс щаебзп бщмб 3.
ддомцеъ леммеъ: 1) щойшд тм ощчм веу бшйа; 2) бйцет фтймеъ вефрйъ; 3) ъжерд длеммъ йшчеъ, фйшеъ егврйн омайн едфзъъ бщш аген. бозчш рлмме 992 оиефмйн, брй 60 бооецт, ащш дщъъфе бозчш ачшай дтесч бийфем длйоеъшфй бйп дщрйн 1999-2001, лащш рйъез дръерйн дрелзй ртшк бйп дщрйн 2016-2017. лм ощъъу чйбм цйеп бйп 0-6, дощчу аъ ойгъ ддчфгд тм ддомцеъ маешз зййн бшйа бодмк е-6 зегщйн азшй дийфем длйоеъшфй, елп цйеп бйп 0-8 доъййзс вн мцшйлъ амледем, лащш цйеп вбед йеъш обиа дърдвеъ бшйад йеъш. бодмк ъчефъ отчб щм л-7 щрйн, ъетге 335 очшйн щм дйщреъ дозмд е-299 очшй ъоеъд (оъелн 43 очшй ъоеъд мма дйщреъ дозмд). роца лй бдщееад мощъъфйн тн цйеп щм 0 ае 1, бчшб ощъъфйн тн цйеп щм 5 ае 6 дсйлеп мъоеъд дйд роек б-42%. лащш рмчзд бзщбеп цшйлъ амледем, роца лй бчшб ощъъфйн тн дцйерйн двбедйн бйеъш (6 тг 8) дсйлеп мъоеъд дйд роек б-51%. бресу, бчшб ощъъфйн амд ощк ддйщшгеъ мма озмд дйд вбед йеъш.
ръерйн амд обиайн сйлейй дйщшгеъ б-5 дщрйн мазш дозмд щм 85% мтеоъ 76% бчшб ощъъфйн тн дчфгд вбедд мтеоъ роелд тм аешз зййн бшйа, лмеош сйлеп абсемеий роек б-9% мъоеъд. дзечшйн ослойн земй сшип дотй двс дочфйгйн тм ддомцеъ маешз зййн бшйа тщеййн мщфш аъ сйлейй ддйщшгеъ м-5 щрйн щмдн.
https://www.ncbi.nlm.nih.gov/pubmed/29710284
бозчш ъцфйъй (аевеси 2017) рбгч дщйоещ бшфеад ощмйод бчшб огвн оййцв щм оиефмйн бцшфъ щръййн мазш абзеп озмъ дсшип.
босвшъ дозчш 4,349 оиефмйн дщйбе тм счш имферй, дтесч бсевй дийфемйн бдн дщъоще боетг дсчш. обйп лмм дощъъфйн, 16.4% гйеезе лй дн тещйн щйоещ бщйиеъ щереъ щм шфеад ощмйод, лащш 45.3% одн ма тще щйоещ бшфеад ощмйод мфрй абзеп озмъ дсшип.
дщйиеъ дщлйзеъ бйеъш дйе деоаефъйд (64%), гйчеш (22.1%), аесиаефъйд (15.1%), шфеаъ цозйн (8.1%), ъжерд (7.3%) еийфемйн аршвиййн (5.8%). доафййрйн дтйчшййн щм доиефмйн щдщъоще бшфеад ощмйод дйе вйм цтйш, рщйн ешоъ дщлмд вбедд. тег роца лй дщйоещ бшфеад ощмйод дйд боцбйн щм дъчгоеъ дозмд, фвйтд байлеъ дзййн ешоъ лаб вбедд.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм лк щдйгшгшеъ доцб дбшйаеъй дйре вешн ощотеъй бщйоещ бшфеад ощмйод. дн чешайн мдтмаъ шоъ доегтеъ щм доиефмйн бревт мафщшейеъ дщйоещ бшфеад ощмйод.
https://www.ncbi.nlm.nih.gov/pubmed/28150122
бсчйшд очйфд, (ошх 2018) длеммъ счйшеъ щйиъйеъ еоид-армйжеъ щм озчшйн ъцфйъййн, рбгче ддщфтеъ дбшйаеъйеъ дчщешеъ бцшйлъ сйбйн ъжеръййн. бсчйшд рлмме 18 оид-армйжеъ, добессеъ тм 298 озчшйн ъцфйъййн фшесфчийбййн, ащш бзре 21 ъецаеъ бшйаеъйеъ, лемм вйгемйн сширййн еишен-сширййн, ъзмеад чшгйеесчемшйъ, ъоеъд, селшъ сев 2 еозмъ чшедп.
баефп лммй, роца лй бдъййзс мщщ одъецаеъ щрбгче (29%) дооцайн дйе оебдчйн, лмеош, цшйлъ сйбйн ъжеръййн дйъд чщешд бдфзъъ дсйлеп мъзмеад еъоеъд чшгйеесчемшйъ, ъоеъд олм вешн, озмъ мб лмймйъ, сшип дмбмб есшип дчйбд. бдъбсс тм щйиъ гйшев аойреъ дтгейеъ дозчшйеъ, дзечшйн оцае лй щмещ одъецаеъ дйе бшоъ дбйизеп двбедд бйеъш (гшвд 1) – сшип мбмб еъоеъд олм вешн ае овешойн чшгйеесчемшййн – ещъййн одъецаеъ дйе бшоъ бйизеп вбедд (гшвд 2) – ъзмеад чшгйеесчемшйъ еозмъ мб лмймйъ.
дзечшйн ослойн лй йщрп тгейеъ обессеъ млк щцшйлъ сйбйн вбедд чщешд бсйлеп чшгйеесчемшй роек йеъш, бтйчш озмъ мб лмймйъ еъоеъд дчщешд байшетйн чшгйеесчемшййн, елп тщейд мъшен мдфзъъ дсйлеп мозмеъ лшерйеъ щереъ.
https://www.ncbi.nlm.nih.gov/pubmed/29566200
бозчш зък, (оай 2017) щртшк бошлж шфеай бчешйад, рбгч дщйоещ бшфеад ощмйод бчшб 216 оиефмйн тн вйгем сширй елп рбгч дчщш бйп дщйоещ бшфеад ощмйод мбйп оггйн щм зшгд, гйлаеп еайлеъ зййн.
обйп лмм доиефмйн, л-60% гйеезе тм щйоещ бшфеад ощмйод, лащш дийфем дщлйз бйеъш дйд цозй ошфа (68% обйп дощъощйн), ащш лмм бйп дщаш щйоещ бвЧйрсрв чешйарй аген (Panax ginseng) ефишйеъ ошфа.
доафййрйн щм оиефмйн амд дйе вйм цтйш йеъш, шоъ дщлмд вбедд йеъш, шоъ длрсд вбедд йеъш, риййд фзеъд мзфщ ййтех мвбй шфеад ощмйод одшефа доифм евйгем бщмб оъчгн йеъш тн вшешеъ ошезчеъ йеъш. тег роца лй дощъощйн бшфеад ощмйод дйе бтмй шоъ зшгд егйлаеп роелд йеъш баефп оебдч, баефп бмъй ъмей бощърйн лое ойп е-BMI.
ма роцае дбгмйн оебдчйн бйзс майлеъ дзййн.
https://www.ncbi.nlm.nih.gov/pubmed/28453297
бсчйшд оецвеъ дтгейеъ, бтйчш оозчшйн фшд-чмйрййн, (ошх 2017) мвбй дфтймеъ дарий-сширйъ щм шлйбйн ибтййн щерйн еддщфтд дсйршвйсийъ щмдн - бгвщ тм шлйбйн амчмеайгйн, фмбереайгйн есаферйрйн доефчйн оовееп цозйн.
https://www.ncbi.nlm.nih.gov/pubmed/28304343
бозчш ъцфйъй (ошх 2017) оъашйн дзечшйн аъ севй дийфем даерчемевй дайрившийбй, щрйъп тм йгй шефайн риешефъйн м-324 земеъ сшип дщг бошлж аерчемевй башд"б (еещйрвиеп).
бдъбсс тм дъйчйн дшфеаййн щм доиефмеъ, роца лй бщръ дийфем дшащерд рйъре йеъш о-72 ийфемйн щерйн, ббмйтд ае бщйоещ зйцерй:
ъжерд, цозй ошфа, фишйеъ ошфа ефшебйеийчд.
фишййъ чешйемес (Trametes versicolor) рйърд м-63% одоиефмеъ, ийфемй веу-рфщ деомце м-45% одоиефмеъ егйчеш м-49% одоиефмеъ.
бресу, 26% одоиефмеъ чйбме ийфем щрйъп бжшйчд, лемм щймеб щм гбчеп (Viscum) ечеофмчс ейиойрй B й(12%) , ейиойп Cй (12%), аъ дъшефд artesunate й (7%) ае джрд ережмйн (4%).
тмеъ дийфем ртд бйп 1600$ мщрд тбеш земеъ бщмб 1 етг 6200$ мщрд тбеш земеъ бщмб 4, лащш доиефмеъ щймое баефп фший тм л-21% отмеъ дийфем.
https://www.ncbi.nlm.nih.gov/pubmed/27230757
бозчш ъцфйъй,(йерй 2017) щртшк бвшорАйд, рбгч дщйоещ бшфеад ощмйод бчшб оиефмйн тн омреод ербгчд дайришачцйд тн овееп дийфемйн дшфеаййн дчййойн.
дозчш ртшк баоцтеъ щамерйн, щоемае тм йгй мотмд о-1,000 оиефмйн бщбтд ошлжйн шфеаййн. бдъан мойгт щрасу бщамерйн, дзечшйн сйееве аъ дсйлеп майришачцйд щм щйиеъ дшфеад дощмйод машбт чивешйеъ: ма сбйш, афщшй, сбйш еайп ръерйн. роца лй 41% олмм доиефмйн гйеезе тм щйоещ бщйиеъ щереъ щм шфеад ощмйод, одн 63% риме ъесфй ъжерд щерйн (лемм ейиойрйн еойршмйн) ецозй ошфа. обйп 335 доиефмйн ащш очбмйн ае щчйбме бтбш ийфемйн арий-сширййн чербрцйермйн щерйн, 28% гйеезе тм щйоещ бъесфйн.
дзечшйн огеезйн лй бдъан моегм щм дсйлеп майришачцйд, 24% одоиефмйн дочбмйн ийфем арий-сширй е-85% одоиефмйн щреимйн ъесфйн бочбйм, роцайн бсйлеп осейн майришачцйеъ. дзечшйн ослойн лй тм оръ мщфш аъ йтймеъ ебийзеъ дийфем бомреод тм доиефмйн мййгт аъ даерчемев бревт мщйоещ бъесфйн, еайме аерчемевйн цшйлйн мдлйш аъ дтгейеъ емдгшйк аъ доиефмйн мвбй щйоещ биез бъесфйн.
дтшъ отшлъ: бозчшйн чегойн лбш дегвн лй дтшлеъ дсйлеп дп вбедеъ одчййн бфетм, шае лап.
https://www.ncbi.nlm.nih.gov/pubmed/28252553
бозчш ъцфйъй вмебмй шзб,(йерй 2018) щртшк б-195 огйреъ, оцйвйн дзечшйн аъ довоеъ бочшй дъзмеад едъоеъд осшип. баефп лммй, змд тмййд щм 28% бочшй дсшип бтемн бйп дщрйн 2006-2016, тн тмййд ощотеъйъ йеъш богйреъ тн огг сецйе-гоевшфй роек йеъш.
https://www.ncbi.nlm.nih.gov/pubmed/29860482
боаош, (йерй 2018) щфешсн оитн давегд даошйчайъ маерчемевйд чмйрйъ (ASCO), ъеолйн длеъбйн бдрзйеъ давегд маерчемевйд айрившийбйъ (SIO) мщймеб ийфемйн айрившийбййн бодмк ае мазш дийфем дчербрцйерамй бсшип дщг.
ддрзйеъ оъййзсеъ мщйоещ бийфемйн айрившийбййн мдчмд тм дъсойрйн етм ъефтеъ дмееай, лемм зшгд, сишс, дфштеъ оцб шез, тййфеъ, фвйтд байлеъ дзййн, бзймеъ едчаеъ тм шчт лйоеъшфйд, мйофагод, рейшефъйд дйчфйъ тм шчт лйоеъшфйд, лаб едфштеъ щйрд. щйиеъ дийфем леммеъ илрйчеъ веу-рфщ, шлйбйн ибтййн ещйрейй аешз зййн. бдъбсс тм счйшд щйиъйъ щм озчшйн ачшаййн обечшйн, роцад ъойлд мдомцеъ дбаеъ:
- мдчмд тм зшгд есишс: ийфем боесйчд, огйицйд, илрйчеъ мрйдем сишс ейевд.
- мдчмд тм гйлаеп едфштеъ оцб шез: огйицйд, илрйчеъ дшвтеъ, йевд, тйсей еийфем боесйчд.
- мщйфеш айлеъ дзййн: огйицйд ейевд.
- мдфзъъ бзймеъ едчаеъ тм шчт лйоеъшфйд: гйчеш ерчегеъ мзйцд.
- ацийм-м-чшрйийп айре оеомх морйтъ рейшефъйд дйчфйъ тм шчт лйоеъшфйд бщм сйлеп мдщфтеъ щмймйеъ.
- айп осфйч тгейеъ обессеъ бревт мщйоещ бшлйбйн ибтййн мдфзъъ ддщфтеъ дщмймйеъ щм дийфем дарий-сширй.
https://www.ncbi.nlm.nih.gov/pubmed/29889605
зжшд мъзймъ дозчшйн
вешой сйлеп
лммй | дщСоръ йъш | сеМлшъ | вДйм дотбш | озмеЙъ отшлъ дтйлем
вешой сйлеп - лммй
боиа армйжд щм озчшй течбд фшесфчийбйн (2019) детшле 80,110 очшй сшип згщйн едчщш щмдн мъжерд ъъ-аефийомйъ. роца лй бтбеш сшип дотй двс, щйтеш дочшйн дчщешйн мъжерд ъъ аефийомйъ дйд двбед бйеъш (n=52,225, 38.3%). цшйлд роелд щм гврйн омайн (n=27,763, 1.8%) еоецшй змб (n=17 692, 1.2%) ецшйлд вбедд щм бщшйн отебгйн (n=14 524, 1.0%) ъшое мтеос/рим двбед бйеъш. вбшйн, бвйм дтойгд (45-64 щрйн) еойтеийн вжтййн / аърййн (щзешйн щайрн дйсфрййн, дйсфрйн еазшйн) дйе бщйтеш двбед бйеъш щм сшип дчщеш мгйаид бдщееад мчбецеъ вйм, ойп ечбецеъ вжт / аърйеъ азшеъ.
https://www.ncbi.nlm.nih.gov/pubmed/31360907
бозчш очшд-бчшд, (2019) ащш обесс тм ръерйн оозчш ачшай обечш вгем, щртшк бсйп, рлмме 229 ощъъфйн тн абзрд згщд щм сшип, амйдн деъаод чбецъ бйчешъ щм 229 ощъъфйн мма сшип. роца лй:
- шод вбедд йеъш бгн щм ейиойп E дййъд чщешд бсйлеп оефзъ мсшип ботшлъ дтйлем.
- шоъ ейиойп E вбедд дййъд чщешд бсйлеп оефзъ мсшип баефп лммй бчшб ощъъфйн тн шоъ смрйен вбедд, ак бсйлеп оевбш мсшип бчшб ощъъфйн тн шоъ смрйен роелд.
https://www.ncbi.nlm.nih.gov/pubmed/30713028
озчш очшд-бчшд шишесфчийбй (гцобш 2015) ащш ретг мбзеп дан чййн чщш бйп щйоещ бимч бажеш айбшй дойп мбйп дсйлеп мсшип дщзмеъ. бозчш рлмме 2,041 рщйн тн сшип дщзмеъ ечбецъ дщееад щм 2,100 рщйн бшйаеъ бтмеъ оафййрйн геойн. дзечшйн зйщбе аъ "щреъ дщйоещ" бимч баефп йщйш ае баефп тчйу баоцтеъ фгйн, иоферйн ае ъзъерйн тбеш лм айщд.
баефп лммй роца лй щйоещ бимч дйд омеед бсйлеп вбед бл-33% мсшип дщзмеъ, лащш шоъ дсйлеп тмъд бщйоещ ооещк йеъш. дзечшйн офшийн лй рщйн ащш дщъоще бимч рие мдйеъ обевшеъ йеъш, щореъ йеъш, тн риййд масъод емщйоещ бощллй лабйн.
лое лп, роца лй щйоещ бимч овбйш аъ дсйлеп мсевйн осейойн щм сшип дщзмеъ елй дчщш ъмей вн бтйщеп, дщорд, вйм дайщд (мфрй ае азшй вйм дфешйеъ) ещйоещ бийфем дешоермй змйфй.
дзечшйн оцйтйн лй имч тмем мдщфйт тм дфтймеъ ддешоермйъ едъвебд дзйсерйъ едгмчъйъ еблк мдвбйш аъ дсйлеп мсшип дщзмеъ.
http://www.ncbi.nlm.nih.gov/pubmed/26689397
озчш очшд-бчшд (ошх 2016) щретг мдтшйк аъ дчщш бйп догг едтеос двмйчой мбйп шоъ дселш мазш дашезд едсйлеп мсшип дшйаеъ бчшб аелмесййд мбрд.
бозчш рлмме 1,905 земйн тн абзрд згщд щм сшип шйаеъ ечбецъ бчшд щм 2,413 ощъъфйн бшйайн.
роца лй цшйлд щм ъжерд бтмъ айргчс етеос вмйчой вбед йеъш дййъд омеед бтмййд щм л-48% бсйлеп мсшип шйаеъ (зойщеп тмйеп мтеоъ ъзъеп). чщш жд дйд беми йеъш тбеш ма отщрйн, тбеш сшип шйаеъ осев SCC етбеш ощъъфйн тн фзеъ о-12 щреъ мйоег.
озчш жд оцбйт тм лк щцшйлъ фзойоеъ фщеиеъ еселшйн тмемд мдвбйш аъ дсйлеп мсшип шйаеъ щайре лъецад отйщеп емъшен мвйбещ асишивйеъ морйтъ дозмд.
http://www.ncbi.nlm.nih.gov/pubmed/26944871
бозчш течбд фшесфчийбй,(2020) бе рлмме л-8,000 обевшйн отм вйм 45 оашд"б, роца лй жоп ооещк йеъш щм дърдвеъ йещбрйъ дйд чщеш бсйлеп оевбш мъоеъд осшип, лащш дзмфъ дърдвеъ йещбрйъ бфтймеъ вефрйъ дййъд чщешд бдфзъъ дсйлеп.
https://pubmed.ncbi.nlm.nih.gov/32556069/
бозчш течбд, (2018) щлмм аъ ръерй цшйлъ дамледем едтйщеп щм обевшйн отм вйм 15 баесишмйд бйп дщрйн 1935-2014, роца лй дфзъд щм л-1 мйиш бцшйлъ дамледем дщръйъ ещм 1 ч"в ибч магн бщрд чщешд бйшйгд щм 3.9% ещм 16%, бдъаод, бщйтеш дъоеъд осшип - маешк ъчефд щм л-20 щрд.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2687388
бозчш течбд (ошх 2017) рбгч дан ъжерд гмчъйъ бъчефъ вйм ддъбвшеъ чщешд бсйлеп мсшип дщг бвйм обевш йеъш.
дозчш дрелзй обесс тм дръерйн щм л-45,000 рщйн, щдщъъфе бозчш течбд вгем ("озчш дазйеъ дщрй"). гфес дъжерд детшк мшащерд бщръ 1991, лащш дощъъфеъ дйе бреъ 27-44, ебецт отчб лм 4 щрйн. бщръ 1998, лащш дощъъфеъ дйе бреъ 33-52, дп дъбчще мгеез аегеъ гфес дъжерд щмдп бъчефъ дъйлеп. тм бсйс щамерй дъжерд, дзечшйн дтшйле аъ шоъ дгмчъйеъ щм дъжерд тбеш лм ощъъфъ. бъчефъ отчб щм л-22 щрд аебзре 1,477 очшйн щм сшип дщг.
роца лй рщйн щаефййре бгфес ъжерд гмчъйъ бвйм цтйш дйе бсйлеп вбед йеъш щм тг 40% мдъфъзеъ сшип дщг мфрй вйм дотбш, ак ма азшй вйм дотбш. дзечшйн ослойн лй ооцайн амд оцбйтйн тм лк щъжерд бвйм цтйш, доаефййръ бцшйлд вбедд щм ощчаеъ ооеъчйн еощчаеъ гйаи, гврйн ма омайн, бщш аген, бщш отебг еошвшйрд, ебцшйлд роелд щм тмйн йшечйн, йшчеъ оцмйбйн ечфд чщешд бсйлеп вбед йеъш мсшип дщг мфрй вйм дотбш.
https://www.ncbi.nlm.nih.gov/pubmed/28249935
озчш течбд вгем (йемй 2016) щртшк бдемрг ретг мдтшйк аъ дсйлеп ашек диеез мдъфъзеъ сшип дщг бчшб рщйн ащш тбше ийфемй фешйеъ IVF.
бозчш рлмме 19,158 рщйн, ащш дзме ийфемй IVF бйп дщрйн 1983-1995 е-5,950 рщйн ащш дзме ийфемй фешйеъ азшйн бйп дщрйн 1980-1995. дотчб ртшк тг 2013 лащш двйм дзцйерй щм дрщйн бсеу ъчефъ дотчб дйд 53.8 бчбецъ д-IVF е-55.3 бчбецъ ддщееад. ръерй дозчш расфе баоцтеъ дшщеоеъ дшфеайеъ ещамерйн щрщмзе мощъъфеъ бгеаш. бъчефъ отчб щм л-21 щрд аебзре 839 очшйн щм сшип щг вшешъй е-109 очшйн щм сшип щг ма фемщрй.
ма роца дбгм бсйлеп мсшип дщг бйп чбецъ д-IVF мбйп дсйлеп брщйн щтбше ийфемй фешйеъ азшйн ае мсйлеп баелмесййд длммйъ бдемрг, лащш дщлйзеъ доцибшъ мсшип дщг бвйм 55 дййъд 3.0% бчбецъ д-IVF мтеоъ 2.9% бчбецъ ддщееад.
тег роца лй дсйлеп дйд роек йеъш бл-45% бчшб рщйн щтбше 7 озжешй IVF ае йеъш, мтеоъ рщйн щтбше 1-2 озжешйн. лое лп, роца сйлеп роек бл-23% бчшб рщйн тн ъецаеъ роелеъ бийфем дшащеп (фзеъ о-4 мтеоъ 4 еотмд бйцйеъ щрасфе).
дзечшйн ослойн лй дооцайн оцбйтйн тм лк щрщйн дтебшеъ ийфемй IVF айрп роцаеъ бсйлеп оевбш мсшип дщг бдщееад мийфемй фешйеъ азшйн ае бдщееад маелмесйд длммйъ.
http://www.ncbi.nlm.nih.gov/pubmed/27434442
бозчш течбд (ошх 2016) щлмм л-50,000 рщйн йфрйеъ азшйдп бецт отчб щм л-14 щрд роца лй гфес ъжерд отшбй дйд омеед бсйлеп оевбш мсшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/26997498
озчш течбд фшесфчийбй (оай 2016) щретг мдтшйк аъ дчщш бйп вешойн щерйн щм аешз зййн мбйп ъзмеад еъоеъд осшип (олм дсевйн омбг сшип дтеш, сшип оез, сшип мйофъй, сшип доиемевй евйгемйн бтшоерйъ щайрн вешойн мъоеъд).
дръерйн обессйн тм щрй озчшй течбд вгемйн бдн дщъъфе л-135,000 арщй очцет оъзен дбшйаеъ етм ръерй дъзмеад едъоеъд оозмеъ дсшип башд"б.
мцешк дозчш дзечшйн двгйше аешз зййн бшйа лтйщеп щм тг 5 щреъ-чефсд, дйортеъ оамледем ае цшйлд оъерд щм амледем (тг ощчд азг мйен тбеш рщйн етг 2 ощчаеъ мйен тбеш вбшйн), BMI биеез щм 18.5-27.5 ебйцет фтймеъ айшебйъ щбетйъ щм мфзеъ 75 гчеъ бтцйоеъ вбедд ае 150 гчеъ бтцйоеъ бйрерйъ.
л-28,000 рзчшйн, щтоге блм 4 дърайн, девгше лчбецъ дсйлеп дроек елм щаш дрзчшйн ,107,000 босфш, девгше лчбецъ дсйлеп двбед.
дзечшйн зйщбе аъ дсйлеп дойезс маелмесйд* баоцтеъ дщееад бйп ръерй дъзмеад едъоеъд бчбецъ дсйлеп дроек мбйп чбецъ дсйлеп двбед еоцае лй дсйлеп дойезс мъзмеад дйд 25% мрщйн е-33% мвбшйн едсйлеп дойезс мъоеъд дйд 48% мрщйн е44% мвбшйн. ръерй сйлеп вбедйн йеъш роцае бдщееаъ чбецъ дсйлеп дроек маелмесййд дмбрд длммйъ даошйчайъ.
дзечшйн ослойн лй 20-40% оъзмеаъ дсшип елозцйъ оъоеъъ дсшип баелмесййд рйъръ морйтд баоцтеъ дчфгд тм аешз зййн бшйа.
*дтшъ дотшлъ: сйлеп ойезс маелмесйд (population-attributable risk) оцййп аъ азеж дочшйн щма дйе земйн/оъйн ан дйе щеЙошйн тм аешз зййн бшйа лй щдевгш бозчш.
http://www.ncbi.nlm.nih.gov/pubmed/27196525
озчш течбд вгем шб-ошлжй (ошх 2016) ащш ретг мдтшйк аъ дчщш бйп дсъййгеъ дтешчйн длмймййн мбйп дсйлеп мозмеъ щайрп чшгйеесчемшйеъ.
бозчш рлмме 6,814 ощъъфйн о-6 ошлжйн щерйн азшйдн бецт отчб щм л-10 щрйн мдтшлъ дсйлеп мсшип, гмчъ шйаеъ, COPD, озмъ лмйеъ лшерйъ, фччъ ешйгйн еъсзйу шйаъй, щбш бйшк егорцйд ъек дъаод сиийсийъ мвешойн сецйе-гоевшфййн ебшйаеъййн емдшвмй зййн.
роца лй бдщееад мощъъфйн мма дсъййгеъ бтешчйн длмймййн, амд тн дсъййгеъ дйе бсйлеп вбед йеъш мсшип (153%), мозмъ лмйеъ лшерйъ (170%), мгмчъ шйаеъ (197%), м- COPD, озмъ шйаеъ зсйоъйъ лшерйъ (271%) емщбш бйшк (429%).
дзечшйн ослойн лй аелмесййд щайрд себмъ одсъййгеъ дтешчйн длмймййн роцаъ бсйлеп роек йеъш мъзмеад дчщешд бвйм обевш едн олерйн "ожгчрйн бшйайн".
http://www.ncbi.nlm.nih.gov/pubmed/26970999
осчйшд очйфд (йреаш 2016) щм дсфшеъ дозчшйъ щфешсод бйп дщрйн 2006-2014 бйзс мчщш бйп 10 вешойн ъжеръййн мбйп дсйлеп мсшип, темд лй дфзъъ цшйлъ амледем, дчфгд тм ъжерд оаежръ еовееръ ебйцет фтймеъ вефрйъ дн щмещъ двешойн дощотеъййн бйеъш борйтъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/26811140
счйшд (йемй 2016) щретгд мдтшйк аъ дтгейеъ доцбйтеъ тм амледем лвешн мдъфъзеъ севйн щерйн щм сшип.
мщн лк бгчд дзечшъ аъ дооцайн оозчшйн афйгойемевййн ебйемевййн еаъ тецоъ дтгейеъ доафщшеъ мдцбйт тм амледем лвешн мсшип, жаъ мошеъ дтгейеъ доцбйтеъ тм ддщфтд довйрд щм амледем офрй ъзмеад чшгйеесчемшйъ.
дзечшъ иетръ лй дтгейеъ дафйгойемевйеъ дчййоеъ ъеолеъ блк щамледем одеед вешн мосфш севйн щм сшип: мет евшеп, ещи, лбг, отй, фй дибтъ ещг.
дооцайн оъчбмйн тм дгтъ обзйрд бйемевйъ ейщрп тгейеъ дошаеъ лй бочшйн осейойн доцб дйре дфйк тн дфсчъ цшйлъ дамледем.
тн жаъ, олйееп щогебш бозчшй течбд, ддщфтд даойъйъ тщейд мдйеъ чирд ае вгемд йеъш оддтшлеъ.
шоъ дсйлеп ощърд бдъан мсев дсшип, мгевоа, бцшйлд щм 50 вшн еотмд амледем мйен дсйлеп тбеш сшип мет еещи вгем фй4-7, бдщееад мдйортеъ оамледем, етбеш сшип отй, лбг ещг дсйлеп вгем фй 1.5.
дзечшъ ослоъ лй йщрп тгейеъ обессеъ млк щцшйлъ амледем одеед вешн мдъфъзеън щм 7 севй сшип, еллм дршад вн мсевйн ресфйн. ддтшлд дйа щщйтеш очшй дсшип лъецад оцшйлъ амледем одеед 5.8% оск очшй дъоеъд осшип бтемн. дйа оцййръ лй жйдей дорврерйн дбйемевййн айре длшзй тм оръ мдсйч тм чщш сйбъй бйп амледем едъфъзеъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/27442501
счйшд (йемй 2016) доцйвд аъ вешой дсйлеп мдъфъзеъ сшип дмбмб, сшип двешн мщйтешй ъоеъд вбедйн.
аелмесййд бвйм обевш йеъш, ооеца афше-аошйчай, бтмй оеицйеъ врийъ дчщешеъ бсшип дмбмб, гмчъ мбмб лшерйъ (овешойн ъешщъййн ае азшйн), селшъ ебтмй сев гн щайре O роцайн бсйлеп вбед йеъш мдъфъзеъ сшип дмбмб.
вешой сйлеп дрйърйн мщмйид емщйрей леммйн тйщеп, щореъ, вешойн ъжеръййн лое цшйлд вбедд щм бщш ещеорйн езщйфд мштмйн.
дзечшйн ослойн лй баоцтеъ асишивйеъ орйтд бшоъ даелмесййд елп баоцтеъ ълрйъ абзеп мчбецеъ бсйлеп, рйъп мщфш аъ дабзеп доечгн емдфзйъ аъ дъзмеад бсшип дмбмб.
http://www.ncbi.nlm.nih.gov/pubmed/27461582
лзмч офшейчи шзб дйчу щм вефй озчш бйрмаеоййн дтесч борйтъ сшип баоцтеъ щойшд тм аешз зййн бшйа, фешсн мазшерд ге"з (2016) ащш оцбйт тм вешой дсйлеп мдъфъзеъ сшип дчйбд. дге"з обесс тм рйъез щм 89 озчшйн ошзбй дтемн длеммйн л-17.5 оймйеп обевшйн ел-77,000 очшйн щм сшип дчйбд.
дзечшйн ослойн лй йщрп тгейеъ обессеъ дошаеъ лй цшйлд щм 3 еотмд ощчаеъ амледемййн мйен, щм ожереъ дощеМошйн бомз (лвеп зоецйн егвйн омезйн), щм бщш отебг елп тегу ощчм едщоръ йъш одеейн вешой сйлеп мдъфъзеъ сши дчйбд.
бресу, йщрп тгейеъ оевбмеъ доцбйтеъ тм лк щцшйлъ бщшйн егвйн цмеййн едйортеъ ае цшйлъ лоеъ роелд щм фйшеъ вн овбйшйн аъ дсйлеп мсшип дчйбд, бтег щцшйлъ фйшеъ дгш чщешд бсйлеп оефзъ.
http://www.wcrf.org/sites/default/files/Stomach-Cancer-2016-Report.pdf
бозчш (оай 2017), добесс тм ръерйн оашбтд озчшй течбд щртшле байшефд ебдн л-3,000 ощъъфйн, роца лй цшйлъ ъд ак ма чфд - бчшб рщйн, ак ма бчшб вбшйн - дййъд чщешд бщйреййн босфш врйн щдйрн бтмй дщфтд тм доибемйжн щм асишгйем едъфъзеъ сшип.
https://www.ncbi.nlm.nih.gov/pubmed/28535255
оаош (ошх 2016) бе оецвеъ ъецаеъ о-10 щреъ отчб ресфеъ щм озчш течбд фшесфчийбй бе рбгч дчщш бйп ъгйшеъ дщфйлд мбйп дсйлеп мсшип дтшоерйъ.
бъзймъ дозчш бщръ 1992 л-32,000 вбшйн дъбчще мтреъ тм щамеп мдтшлъ ъгйшеъ дщфйлд дзегщйъ б-3 рчегеъ жоп - бвйм 20-29, 40-49 ебщрд мфрй оймей дщамеп.
бодмк 18 щреъ отчб 3,839 одощъъфйн аебзре тн сшип дтшоерйъ. роца лй ъгйшеъ щфйлд двбедд о-21 фтойн бзегщ, мтеоъ 4-7 фтойн бзегщ бвйм 20-29 дййъд омеед бсйлеп оефзъ мсшип дтшоерйъ щм л-19% ещм л-22% бвйм 40-49. лмеош, ъгйшеъ щфйлд вбедд йеъш бодмк дзййн тщейд мдееъ вешн овп офрй дъфъзеъ сшип дтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/27033442
оегм щретг мдтшйк аъ дсйлеп мсшип дщг бдъййзс мдбгмйн вриййн щлйзйн (single nucleotide polymorphisms) емвешой сйлеп афйгойемевййн (оай 2016).
доегм обесс тм ръерйн ощрй озчшйн вгемйн, озчш очшд бчшд длемм 17,171 рщйн тн сшип дщг е-19,862 рщйн бшйаеъ еогвн ресу щм 5,879 рщйн щдщъъфе бсчш дбшйаеъ дмаеой.
рйбей дсйлеп дабсемеий мсшип дщг тбеш рщйн аошйчайеъ мбреъ обесс тм ръерйн айщййн, щйтеш дщлйзеъ баелмесййд, вешой сйлеп афйгойемевййн ещйтешн баелмесййд елп ръерйн бйзс м-24 дбгмйн вриййн щроцае бозчшй течбд едтшлеъ сйлеп щфешсое бйзс м-68 дбгмйн вриййн ресфйн.
тбеш лм айщд рбгче доафййрйн двриййн, дйсиешйд ощфзъйъ, оггйн аръшефеоишййн, вешойн дчщешйн бозжеш деесъ ебфешйеъ евешой аешз зййн.
боегм ма рлмме рщйн тн оеицйд бвп BRCA ащш чщешд бсйлеп оевбш ощотеъйъ мсшип дщг едщзмеъ.
тм фй доегм, дсйлеп дооецт щм айщд аошйчайъ мбрд бъ 30 мдъфъзеъ сшип щг вшешъй тг мвйм 80 дйре 11.3%, лащш бдъййзс млмм двешойн, дсйлеп рт бйп 4.4% м-23.5%.
обйп дрщйн дроцаеъ бсйлеп вбед бщм вешойн щайрн рйърйн мщйрей (врийчд, дйсиешйд ощфзъйъ, вебд евешойн дчщешйн бозжеш ебфешйеъ), амд щщоше тм дшвмй зййн бшйайн (BMI роек, дйортеъ отйщеп, цшйлд оъерд щм амледем едйортеъ оийфем дешоермй змйфй мазш вйм дотбш) дйе бсйлеп геод майщд ооецтъ баелмесййд длммйъ.
дзечшйн ослойн лй бтжшъ доегм рйъп мждеъ аелмесйеъ бсйлеп вбед ащш ълрйеъ мщойшд тм аешз зййн бшйа тщейеъ мдйеъ йтймеъ бойезг тбешп.
http://www.ncbi.nlm.nih.gov/pubmed/27228256
оаош чцш (гцобш 2016) дтесч бщамд дан чййн чщш бйп дшлб дзййгчйн бщъп мбйп дсйлеп мсшип щмфезйъ дщъп. дзечш осбйш лй сшип щмфезйъ дщъп щлйз фй 2-4 бчшб вбшйн мтеоъ рщйн, ръеп щрдев мдсбйше баоцтеъ щйтеш тйщеп вбед йеъш бчшб вбшйн. тн жаъ, ооцайн тглрййн оцбйтйн тм лк щдщъп айрре сишймй лфй щрдев дйд мзщеб, еолйм аелмесййъ зййгчйн овееръ. дшлб дзййгчйн щерд бйп вбшйн мрщйн, лащш рщйн оаефййреъ бшод вбедд йеъш щм зййгчйн оощфзъ Actinomycetes.
жшйчеъ BCG (ебщоп дома: Bacillus Calmette–Guérin) долймеъ зййгчйн оощфзъ Actinomycetes ощощеъ лзйсеп морйтъ щзфъ, ак вн мийфем бсшип щмфезйъ дщъп. олап, аелмесййъ зййгчйн бтмъ дшлб вбед щм зййгчйн оощфзъ Actinomycetes тщейд мдееъ дсбш афщшй мщйтеш роек йеъш щм сшип щмфезйъ дщъп бчшб рщйн.
дзечш ослн лй маеш вймей чйен зййгчйн бщъп, ргшщъ дтшлд озегщъ бревт мвешой дсйлеп мсшип щмфезйъ дщъп еасишивйеъ морйтъе.
https://link.springer.com/article/10.1007%2Fs10654-016-0213-z
бозчш ъцфйъй (йерй 2017) рбгч дчщш бйп дрчд мбйп дсйлеп мсшип дшзн. дозчш обесс тм ръерйн щрасфе б-17 озчшйн (3 озчшй течбд е-14 озчшй очшд-бчшд), лзмч ощйъеу фтемд озчшй бреща дафйгойемевйд щм сшип дшзн (Epidemiology of Endometrial Cancer Consortium).
брйъез дръерйн рлмме 8,981 рщйн тн сшип дшзн емазш мйгд азъ мфзеъ, ечбецъ бйчешъ щм 17,241 рщйн мма сшип дшзн. роца лй дрчд баефп лммй дййъд чщешд бсйлеп роек б-11% мсшип дшзн, лащш ощк дрчд ашек йеъш млм ймг дйд чщеш бйшйгд вгемд йеъш бшоъ дсйлеп, тн дъоъреъ дчщш мазш 6-9 зегщйн. дчщш щроца дйд бмъй ъмей босфш дмйгеъ, б-BMI ае бсев ддйсиемевй щм двйгем. дсбш афщшй млк деа щдрчд оглаъ ййцеш асишевп ащш отешб бдъфъзеъ сшип дшзн.
https://www.ncbi.nlm.nih.gov/pubmed/28486362
бозчш, щртшк бчшб тлбшйн (йреаш 2017), оцйвйн дзечшйн оегм мзчш вешойн сбйбъййн, дчщешйн бдъфъзеъ сшип бзмм дфд едмет - лвеп ибч, амледем еейшес дффймеод - елп огвйойн аъ ддщфтд дойийбд щм фим щзеш морйтъ дъфъзеъ ъдмйлйн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/28092946
лзмч оозчш течбд айшефай вгем, дтесч бчщш бйп сшип еъжерд (EPIC), бозчш дрелзй (йемй 2016) рбгч дчщш бйп айлеъ дъжерд (тм фй тщшд оггйн щерйн) мбйп дсйлеп мъоеъд биеез щм 10 щрйн. бозчш рлмме л-450,000 ощъъфйн бшйайн, азшйдн дзечшйн тчбе мъчефд щм л-12.8 щрйн.
айлеъ дъжерд детшлд баоцтеъ тщшд оггйн щерйн, аеън рйъп мсеев мщмещ чивешйеъ:
- оггйн добессйн тм ддрзйеъ дъжеръйеъ длммйеъ:
Diet Quality Index International (DQI-I), Healthy Eating Index 2010 (HEI-2010), WHO Healthy Diet Indicator (WHO HDI),еHealthy Lifestyle Index (HLI).
- оггйн доъййзсйн мдрзйеъ ъжеръйеъ тбеш оцб шфеай осейн:
WCRF/AICR guideline score for the prevention of cancer, Dietary Approaches to Stop Hypertension (DASH).
- оггйн доъййзсйн мдъаод мгфес гйаид осейн:
Mediterranean Diet Score (MDS), relative Med diet score (rMED), Mediterranean Style Dietary Pattern Score (MSDPS), Healthy Nordic Food Index (HNFI).
ошбйъ доггйн мечзйн бзщбеп аъ айлеъ дъжерд бмбг, бтег щщрййн одоггйн оъййзсйн мвешойн ресфйн – догг HLI ощчмм вн BMI, фтймеъ вефрйъ етйщеп, едогг морйтъ сшип ощчмм вн BMI, фтймеъ вефрйъ едрчд.
дзечшйн огеезйн лй мазш 10 щреъ отчб 15,200 одощъъфйн рфише, 3,761 одн лъецад овешн чшгйеесчемшй е-7,475 одн лъецад осшип. бдъййзс млм азг одоггйн брфшг, роца лй айлеъ ъжерд вбедд йеъш дййъд чщешд бсйлеп роек йеъш мъоеъд олм вешн елп бсйлеп роек йеъш мъоеъд овешн чшгйеесчемшй ае осшип. боегм ощемб длемм дъаод сиийсийъ мвйм, ойп, тйщеп, BMI, дщлмд, фтймеъ вефрйъ еойчен вйаевшфй, роца лй дощъъфйн тн дцйерйн двбедйн бйеъш, мтеоъ дроелйн бйеъш, роцае бсйлеп роек б-12-25% мъоеъд олм вешн, сйлеп роек б-16-24% мъоеъд овешн чшгйеесчемшй, ебсйлеп роек б-9-22% мъоеъд осшип.
дзечшйн ослойн лй оггй айлеъ дъжерд, бщймеб вешой дсйлеп дщлйзйн, оафщшйн мрба бцешд иебд аъ дсйлеп мъоеъд.
https://www.ncbi.nlm.nih.gov/pubmed/27409582
брййш тогд (ребобш 2017) оцдйшд давегд даошйчайъ маерчемевйд чмйрйъ (ASCO) лй цшйлъ амледем одеед вешн сйлеп оебдч, ак дфйк, мдъфъзеъ севйн щерйн щм ооайшейеъ (лемм фд емет, ещи, вшеп, лбг, щг ечемешчимй).
митръ цееъ доеозйн, рчйиъ тогд фшеачийбйъ лрвг цшйлъ амледем оефшжъ дйрд бтмъ ъшеод зщебд морйтъ сшип, лащш оишеъ досок дйрп:
- мтегг фшсен дрзйеъ мцйбеш бревт мсйлерйн длшелйн бцшйлъ амледем оефшжъ бдчщш мдъфъзеъ севйн осейойн щм сшип.
- ъойлд богйрйеъ мдфзъъ дсйлеп мсшип баоцтеъ асишивйеъ обессеъ шайеъ морйтъ цшйлъ амледем оефшжъ.
- мсфч дрзйеъ моифмйн аерчемевййн бревт мдщфтд щм цшйлъ амледем оефшжъ тм дсйлеп мсшип етм дсйбелйн дрмеейн мийфем, лемм дбдшъ тгейеъ сеъшеъ.
- жйдей ъзеойн мозчшйн тъйгййн бревт мчщш бйп цшйлъ амледем едсйлеп мсшип.
босвшъ доаош оецвйн ръерйн афйгойемевййн мвбй цшйлъ амледем, офешиеъ ддомцеъ дрелзйеъ, оецвйн дооцайн бревт мчщш бйп амледем мсшип емдщфтд щм амледем тм ъецаеъ дийфем бсшип. бресу, грйн дзечшйн басишивйеъ мдвбмъ емдфзъъ цшйлъ дамледем лзмч одогйрйеъ дцйбешйъ.
https://www.ncbi.nlm.nih.gov/pubmed/29112463
бозчш течбд обесс аелмесййд (гцобш 2017), щртшк бщбгйд, роца лй вбшйн щсбме оачрд бвйм ддъбвшеъ дйе бтмй сйлеп вбед б-43% мдъфъзеъ сшип дтшоерйъ. дзечшйн ощтшйн лй жйден зййгчй тмем мдвбйш ъдмйлйн гмчъййн додеейн бсйс мдъфъзеъ ооайшеъ. дсбш афщшй ресу деа фтймеъ дешоермйъ аргшеврйъ дотешбъ бщъй дфъемевйеъ догебшеъ.
https://www.ncbi.nlm.nih.gov/pubmed/29205339
бозчш, щртшк бчшб тлбшйн (йреаш 2018), ошайн дзечшйн лйцг амледем отмд аъ дсйлеп мфвйтд б-DNA бъай двжт, еблк ъешн мдсбш лйцг цшйлъ амледем чщешд бсйлеп оевбш мсшип.
https://www.ncbi.nlm.nih.gov/pubmed/29323295
бозчш течбд ршзб (йреаш 2018), щртшк ббшйирйд, рбгч дчщш бйп зщйфд маеш бщтеъ дмймд мбйп дсйлеп мсшип дщг. дзечшйн осбйшйн лй чййоъ дщтшд млк щдфштд мщтеп дбйемевй тчб зщйфд маеш бщтеъ дмймд одеед вешн сйлеп мдъфъзеъ сшип дщг, аемн дооцайн оозчшйн ачемевййн еоозчшй очшд-бчшд щртшле бтбш айрн тчбййн.
бозчш дрелзй рлмме дръерйн щм л-100,000 рщйн мма дйсиешйд щм сшип дщг, лащш бодмк ъчефъ отчб щм л-6 щрйн аебзре 1,775 очшйн щм сшип дщг. дощъъфеъ дъбчще мгеез тм гфесй дщйрд етм ойгъ даеш бзгш дщйрд бъзймъ дозчш ебвйм 20.
баефп лммй, ма роца чщш бйп ойгъ дзщйфд маеш бщтеъ дмймд мбйп дсйлеп мсшип дщг. дооцайн дйе бмъй ъмеййн бсев дсшип едйе геойн тбеш рщйн мфрй ае азшй вйм дотбш. бресу, дооцайн ма дйе ъмеййн бщйрд бщтеъ ма щвшъйеъ ае бдйсиешйд щм тбегд бщтеъ дмймд. дзечшйн оцййрйн лй роца щрщйн тн дйсиешйд щм дмйлд оъек щйрд езщйфд маеш бщреъ д-20 щмдп дйе бсйлеп роек йеъш мсшип дщг мфрй вйм дотбш, ооца дгешщ бйшеш ресу.
https://www.ncbi.nlm.nih.gov/pubmed/29360812
бозчш течбд фшесфчийбй обесс аелмесййд (фбшеаш 2018), щртшк бсйп, рбгч дан щъййъ ъд шеъз чщешд бсйлеп оевбш мсшип деещи, лащш омеед бцшйлъ амледем етйщеп - щдйрн вешой сйлеп обессйн. бозчш рлмме л-450,000 ощъъфйн бвймай 30-79, ащш гйеезе бъзймъ дозчш (бщръ 2004) тм дшвмй цшйлъ дъд еаешз дзййн. бъчефъ отчб щм л-9 щрйн, аебзре 1,731 очшйн щм сшип деещи.
баефп лммй роца лй щъййъ ъд шеъз, бщймеб тн цшйлъ амледем ае тйщеп, дййъд чщешд бсйлеп вбед йеъш баефп ощотеъй мсшип деещи - мтеоъ щъййъ ъд бмбг. ощъъфйн щцшле отм 15 вшн амледем евн ъд шеъз огй йен дйе бтмй дсйлеп двбед бйеъш мсшип деещи, сйлеп двбед фй 5 бдщееад мощъъфйн щцшле ъд мтйъйн шзечеъ ефзеъ о-15 вшн амледем мйен. сйлеп вбед фй 2 роца тбеш ощъъфйн дотщрйн евн цешлйн ъд шеъз огй йен.
дзечшйн ослойн лй цшйлъ ъд шеъз чщешд бсйлеп оевбш мсшип деещи, ак шч лащш омеед бцшйлъ амледем вбедд ае бтйщеп. олап рйъп мдсйч лй щъййъ ъд тмемд мдвбйш аъ ддщфтд дожйчд щм амледем етйщеп тм ъай деещи.
дтшъ отшлъ: досчрд дргшщъ дйа лй йщ мдфсйч тйщеп емдфзйъ цшйлъ амледем, блгй мдорт одсйлерйн дшбйн щйщ бщрй дшвмйн амд. цшйлъ ъд шеъз лщмтцод лршад айрд двешн дтйчшй бдъфъзеъ сшип деещи.
https://www.ncbi.nlm.nih.gov/pubmed/29404576
бозчш течбд фшесфчийбй (йреаш 2018), щртшк биайееап тн отчб азш л-400,000 ощъъфйн бощк 8.7 щрйн бооецт, роца лй ъзмеад лшерйъ лвеп селшъ еозмеъ шйад, елп оггйн мъзмеад лвеп мзх гн есйреп лмййъй, одеейн вешн сйлеп ощотеъй мдъфъзеъ сшип, бойгд дгеод мвешой аешз зййн.
https://www.ncbi.nlm.nih.gov/pubmed/29386192
https://www.medscape.com/viewarticle/892089?src=wnl_edit_tpal&uac=205542DG
бозчш течбд обесс аелмесййд (фбшеаш 2018), щртшк бцшфъ, детшк дчщш бйп цшйлъ ожеп отебг мбйп дсйлеп мдъфъзеъ сшип. бозчш рлмме л-105,000 ощъъфйн брй 43 бооецт, лащш дзечшйн дтшйле аъ шоъ дцшйлд щм л-3,300 ожереъ щерйн баоцтеъ йеорй алймд щоймае дощъъфйн. дожереъ дщерйн сееве мфй щйиъ NOVA машбт чивешйеъ бдъан мгшвъ дтйбег щм дожеп.
бозчш дрелзй дъочге дзечшйн бчивешйд щм ожереъ отебгйн оаег, длеммйн мзойн ашежйн бййцеш доерй, зийфйн оъечйн еомезйн, ооъчйн ечйрезйн ътщййъййн, ощчаеъ оевжйн еооеъчйн, оецшй бщш отебгйн еощеЙошйн, ошчйн еаишйеъ мдлрд одйшд, ашезеъ чфеаеъ еожереъ ресфйн бтмй ълемд вбедд щм селш оесу, щеорйн ае шлйбйн ътщййъййн азшйн. дн бгче аъ дчщш бйп шоъ дцшйлд щм ожереъ амд мбйп дсйлеп мсшип баефп лммй елп мсшип дщг, дтшоерйъ ечемешчимй.
роца лй цшйлд щм ожереъ отебгйн оаег дййъд чщешд бсйлеп оевбш мсшип баефп лммй елп мсшип дщг, лащш тмййд щм 10% бщйтеш щм цшйлъ ожереъ амд бъжерд длммйъ дййъд чщешд бтмййд щм 11-12% бшоъ дсйлеп мсшип. дзечшйн ослойн лй ргшщйн озчшйн ресфйн тм оръ мдбйп иеб йеъш аъ ддщфтд дйзсйъ щм дйбийн щерйн бтйбег дожеп тм дтмййд бъдмйлйн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/29444771
бсчйшд щйиъйъ еоид-армйжд (йреаш 2018) рбгче дтгейеъ бревт мчщш бйп вешой аешз зййн - лемм BMI, ъжерд, ъесфй ъжерд ефтймеъ вефрйъ - мбйп дфшеврежд щм сшип щмфезйъ дщъп.
бсчйшд рлмме 31 озчшйн ъцфйъййн еобечшйн, бдн рбгч дчщш бйп вешой аешз дзййн мбйп дйщреъ, дъчгоеъ ещйтешй ъоеъд бчшб земй сшип щмфезйъ дщъп. роца лй бчшб оиефмйн тн сшип осев NMIBC (ебщое дома: non-muscle invasive bladder cancer), тегу ощчм ещореъ дйе чщешйн бсйлеп вбед б-29% е-82% мдйщреъ, бдщееад мощчм ъчйп.
ма роца чщш бйп BMI мбйп дъчгоеъ дозмд. дооцайн мвбй ъжерд ещйоещ бъесфйн ма дйе тчбййн ема роцае озчшйн дбезрйн аъ ддщфтд щм фтймеъ вефрйъ бсшип щмфезйъ дщъп. дзечшйн ослойн лй дтгейеъ мвбй вешой аешз зййн бсшип щмфезйъ дщъп дп оевбмеъ ергшщйн озчшйн ресфйн тм оръ мвбщ дрзйеъ обессеъ шайеъ бъзен жд.
https://www.ncbi.nlm.nih.gov/pubmed/29430510
бдъбсс тм ръерйн щрасфе бщрй озчшй течбд вгемйн, щртшле башд"б, бозчш дрелзй (афшйм 2018) детшк дчщш бйп цшйлъ дщеоп бъжерд мбйп дсйлеп мсевйн щерйн щм сшип теш.
бозчш азг, щдзм бщръ 1976, рлмме л-120,000 рщйн бвймай 30-55 (озчш дазйеъ) ебозчш дщрй, щдзм бщръ 1986, рлмме л-50,000 вбшйн бвймай 40-75 (озчш арщй очцетеъ дбшйаеъ). цшйлъ дщеоп бъжерд детшлд баоцтеъ щамерй ъжерд огй 4 щрйн тг мщръ 2010. бъчефъ дозчш аебзре 794 очшйн щм омреод, 2,223 очшйн щм SCC (ебщое дома: squamous cell carcinoma) е-17,556 очшйн щм BCC (ебщое дома: basal cell carcinoma) бозчш дазйеъ е-736, 1,756 е-13,092 очшйн, бдъаод, бозчш арщй очцетеъ дбшйаеъ.
бщрй дозчшйн ма роца чщш бйп ск цшйлъ дщеоп мбйп дсйлеп мсшип теш. тн жаъ, роца лй бдщееад мцшйлд дроелд бйеъш, ощъъфйн тн шоъ дцшйлд двбедд бйеъш щм зеоцеъ щеоп шб бмъй шеейеъ дйе бсйлеп вбед б-16% м-SCC еб-6% м-BCC. баефп сфцйфй, цшйлд вбедд йеъш щм аеовд 6 дййъд чщешд бсйлеп вбед йеъш млм севй сшип дтеш ецшйлд вбедд йеъш щм аеовд 3 дййъд чщешд бсйлеп вбед йеъш м-BCC бмбг. ма роца чщш бйп цшйлъ щеорйн осевйн азшйн мбйп дсйлеп момреод едовод дййъд геод тбеш рщйн евбшйн.
https://www.ncbi.nlm.nih.gov/pubmed/29636341
бдъбсс тм ръерй озчш течбд щртшк ббшйирйд (ошх 2018), бозчш дрелзй рбгч дчщш бйп гфес дъжерд мбйп дсйлеп мсшип чемешчимй.
бозчш дрелзй рлмме л-32,000 рщйн, азшйдп бецт отчб бощк л-17 щрд бооецт. бдъбсс тм щамерй ъжерд, дзечшйн сйееве аъ дощъъфеъ м-4 гфесйн ъжеръййн: цозерй, гвйн, теу ебщш аген. бъчефъ дотчб аебзре 462 очшйн щм сшип чемешчимй, одн 335 очшйн щм сшип ботй двс (172 фшечсйомй е-119 гйсимй) е-152 очшйн щм сшип бшчиен.
бдщееад мъжерд длеммъ бщш аген, гфесй ъжерд щайрн леммйн бщш аген дйе чщешйн бсйлеп роек б-14% мсшип чемешчимй еб-23% мсшип дотй двс, аемн ооцайн амд ма дйе оебдчйн сиийсийъ. тн жаъ, брйъез ресу роца лй ощъъфйн щма цшле бщш аген дйе бсйлеп роек б-44% мсшип отй вс гйсимй. ма роца чщш ощотеъй бйп гфес дъжерд мбйп дсйлеп мсшип бшчиен. ооцайн амд оцбйтйн тм лк щцшйлъ бщш аген тмемд мдвбйш аъ дсйлеп мдъфъзеъ сшип ботй двс дгйсимй, аемн йщ мащщ аъ дооцайн бчшб осфш вгем йеъш щм ощъъфйн.
https://www.ncbi.nlm.nih.gov/pubmed/29516512
бозчш ъцфйъй,(2019) добесс тм оавшй ръерйн маеоййн ббшйирйд, роца лй бчшб ма-отщрйн, цшйлъ бчбеч ййп азг бщбет дййъд чщешд бтмййд бсйлеп абсемеий мсшип бодмк дзййн - щм 1% бчшб вбшйн ещм 1.4% бчшб рщйн. тмййд же бсйлеп щееъ тшк мтйщеп 5 сйвшйеъ бщбет бчшб вбшйн е-10 сйвшйеъ бщбет бчшб рщйн.
https://www.ncbi.nlm.nih.gov/pubmed/30917803
брйъез щйиъй щм ръерйн вмебмййн (2017) детшлд ддщфтд щм цшйлд ъъ-ойибйъ щм ожереъ ешлйбй ъжерд тйчшййн тм ъзмеад еъоеъд оозмеъ ма огбчеъ (озмеъ чшгйеесчемшйеъ, селшъ есшип). бозчш рлмме дръерйн о-195 огйреъ бйп дщрйн 1990-2017. баоцтеъ оегмйн сиийсиййн, дзечшйн дтшйле аъ дрим дйзсй мъзмеад щм лм вешн ъжеръй бчшб обевшйн отм вйм 25. дн ошайн лй бщръ 2017 рйъп мййзс 11 оймйеп очшй ъоеъд (22% оск очшй дъоеъд) е-255 оймйеп щреъ рлеъ (15% оск щреъ дрлеъ) мвешойн ъжеръййн. вешой дсйлеп доебймйн богйреъ шбеъ дйе цшйлд вбедд щм ръшп, цшйлд роелд щм гврйн омайн ецшйлд роелд щм фйшеъ. вешойн ресфйн леммйн цшйлд роелд щм авежйн, жштйн, йшчеъ еаеовд 3.
дзечшйн ослойн лй бтег бтщешйн дазшерйн ддъочгеъ дйрд бдщфтеъ щм ъжерд тъйшъ ръшп, селш ещеоп, ооцайн амд осфчйн дбрд шзбд мвбй ддщфтд дафщшйъ щм ъжерд ъъ-ойибйъ тм ъзмеад еъоеъд оозмеъ ма огбчеъ, еблк огвйщйн аъ зщйбеъ щйфеш айлеъ дъжерд бшод двмебмйъ. ръерйн амд тщеййн мсййт бдиотъ дътшбейеъ ъжеръйеъ обессеъ шайеъ емдееъ бсйс мбйцет дтшлд оъощлъ щм дщАфтъп тм доцб дбшйаеъй.
дозчш оеоп тм йгй чшп бйм еомйргд вййис.
https://www.ncbi.nlm.nih.gov/pubmed/30954305
баоцтеъ оегм сиийсий (2019) отшйлйн дзечшйн аъ рим дсшип башд"б дчщеш бъжерд мчейд. доегм обесс тм ръерйн маеоййн щм дцшйлд дъжеръйъ, щм щйтеш очшй дсшип ещм дчщш бйп дъжерд едсйлеп мсшип бдъан мозчшй течбд фшесфчийбййн. тм фй ръерйн амд, дзечшйн отшйлйн аъ осфш ещйтеш очшй дсшип дзгщйн аеън рйъп мййзс мцшйлд ма осфчъ щм щбтд вешойн ъжеръййн бчшб обевшйн отм вйм 20.
мдмп сйлен дооцайн:
- рйъп мййзс мъжерд мчейд л-80,000 оочшй дсшип дзгщйн, додеейн 5.2% оочшй дсшип дзгщйн башд"б бщръ 2015. оъек очшйн амд, 4.4% рйъп мййзс баефп йщйш мвешойн ъжеръййн е-0.82% баефп тчйу лъецад ощореъ.
- бдъййзс мсевй дсшип дщерйн, сшип чемешчимй дйд чщеш бойгд двбедд бйеъш мвешойн ъжеръййн.
- рйъп мййзс л-5% оочшй дсшип мвешойн ъжеръййн, лащш рим дсшип дощотеъй бйеъш роца тбеш цшйлд роелд щм гврйн омайн (1.8%) ещм оецшй змб (1.2%), ецшйлд вбедд щм бщш отебг (1%). вешойн ресфйн леммйн цшйлд роелд щм йшчеъ ефйшеъ, цшйлд вбедд щм бщш аген ецшйлд вбедд щм ощчаеъ ооеъчйн.
- рим дсшип дчщеш бвешойн ъжеръййн дйд вбед бойезг бчшб вбшйн, бчшб аелмесййд бвймай 45-64 ебчшб чбецеъ ойтеи аърйеъ.
https://www.ncbi.nlm.nih.gov/pubmed/31360907
зжшд мъзймъ дозчшйн
вешой сйлеп - дщСоръ йъш
бозчш течбд шб-ошлжй (2020) рбгч дан BMI вбед чщеш бщйтеш дйщшгеъ вбед йеъш бчшб земй сшип, лъмеъ бойп ебвйм. дзечшйн осбйшйн лй мтегу ощчм емщореъ дщфтд бшйаеъйъ ожйчд, аемн йщрп тгейеъ мфйдп бчшб аелмесййд обевшъ тегу ощчм ещореъ чщешйн гееча бдашлъ ъезмъ дзййн, ооца долерд "фшгечс ддщорд". бдчщш щм сшип, дчщш бйп тегу ощчм ещореъ мбйп ъоеъд дйре оешлб йеъш бщм йшйгд ощотеъйъ бощчм.
бозчш рлмме 2,071 земй сшип (дщлйзйн бйеъш дйе сшип чемешчимй есшип щг) отм вйм 70 о-10 ошфаеъ аерчемевйеъ вшйаишйеъ бажеш фшйж. дзечшйн сйееве аъ дощъъфйн бдъан м- BMI боетг дабзрд, елп мщмещ чивешйеъ бдъан мйшйгд бощчм бщщъ дзегщйн дазшерйн: ойрйомйъ (тг 5%), оъерд (5-10%) ае зоешд (отм 10%).
мдмп дооцайн дтйчшййн:
-
бчшб рщйн тн йшйгд ойрйомйъ бощчм, рщйн тн щореъ дйе бсйлеп роек б-44% мъоеъд биеез щм 60 зегщйн бдщееад мрщйн бощчм ъчйп.
-
рщйн тн тегу ощчм ае щореъ, ейшйгд оъерд ае зоешд бощчм, дйе бсйлеп геод мъоеъд лое рщйн бощчм ъчйп ейшйгд ойрйомйъ бощчм.
-
ма роца чщш бйп BMI бчшб вбшйн мбйп дсйлеп мъоеъд, баефп бмъй ъмей бойгъ дйшйгд бощчм.
дзечшйн ослойн лй бчшб земеъ сшип обевшеъ, щореъ дййъд чщешд бсйлеп оефзъ мъоеъд бдщееад мрщйн бощчм ъчйп, шч лащш дйшйгд бощчм дййъд ойрйомйъ.
https://pubmed.ncbi.nlm.nih.gov/32889525
бозчш течбд обесс аелмесййд, (2020) щртшк бйщшам, рбгч дчщш бйп BMI бвйм 17 мбйп дсйлеп мдъфъзеъ сшип емъоеъд осшип. дозчш обесс тм ръерйн щм 2,458,170 ощъъфйн, щрасфе ббгйчеъ мфрй вйес бйп дщрйн 1967-2010. бодмк ъчефъ дотчб аебзре 26,353 очшй сшип бчшб вбшйн е-29,488 очшйн бчшб рщйн.
мдмп дооцайн дтйчшййн (бдщееад м-BMI базежеп 5 тг 49):
-
щйтеш очшй дсшип тмд бдгшвд тн дтмййд бчивешйеъ д-BMI.
-
бчшб вбшйн тн щореъ бвйм ддъбвшеъ дсйлеп мдъфъзеъ сшип дйд вбед б-26%.
-
бчшб рщйн ма роца чщш оебдч бйп щореъ мбйп дсйлеп мсшип, лъецад очщш дфек бйп щореъ мбйп сшип цееаш дшзн есшип дщг. тн жаъ, лащш щрй севй сшип амд децае одрйъез, роца лй бчшб рщйн тн щореъ бвйм ддъбвшеъ дсйлеп мдъфъзеъ сшип дйд вбед б-27%.
-
бчшб ощъъфйн ощрй дойрйн, BMI вбед (отм мазежеп д-85) дйд чщеш бсйлеп оевбш мсшип мазш 10 щрйн. чщш жд дйд ощотеъй йеъш бщрйн доаезшеъ йеъш щм дозчш.
-
тмййд б-BMI дййъд чщешд бсйлеп оевбш мъоеъд осшип, лащш дсйлеп дойезс м-BMI вбед деа 5.1% тбеш вбшйн е-5.7% тбеш рщйн.
дзечшйн ослойн лй дтмййд бщйтешй дщореъ бвйм ддъбвшеъ, едчщш дафщшй бйп BMI бвйм ддъбвшеъ мбйп дсйлеп мсшип тмемйн мдвбйш аъ дрим дтъйгй щм очшй сшип тм шчт щореъ. дн огвйщйн лй BMI бчшб оъбвшйн тщей мдееъ йтг зщеб мдътшбеъ боишд мдфзйъ аъ щйтеш очшй дсшип баелмесййд.
https://pubmed.ncbi.nlm.nih.gov/32027851/
бозчш течбд (ошх 2016) щлмм л-50,000 рщйн йфрйеъ азшйдп бецт отчб щм л-14 щрд роца лй гфес ъжерд отшбй дйд омеед бсйлеп оевбш мсшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/26997498
озчш течбд (ошх 2016) щретг мбзеп аъ дчщш бйп ощк цен дмймд мбйп щйтеш ддйщреъ едъоеъд бчшб рщйн тн сшип дщг, елп жйдей вешой дсйлеп мъецаеъ щмймйеъ афщшйеъ, лемм ощч дселш (HbA1c), гмчъ отшлъйъ (CRP), дщорд еощк дщйрд.
ъецаеъ озчшйн чегойн, щбецте бзйеъ отбгд, дшае лй цен ооещк бодмк дщйрд дйд бтм дщфтд ойийбд тм дфзъъ ъдмйлйн сширййн еъдмйлйн оибемййн дчщешйн бсшип дщг.
бозчш дрелзй рлмме ръерйн щм 2,413 земеъ сшип дщг бщмбйн оечгойн, щайрп земеъ селшъ, бреъ 27-70 бтъ дабзеп. дзечшйн дтшйле аъ ощк цен дмймд баоцтеъ йеорй алймд щм 24 щтеъ щрасфе бъзймъ дозчш, мазш щрд емазш 4 щрйн.
одъецаеъ темд лй цен мймд щм фзеъ о-13 щтеъ дйд омеед бсйлеп вбед бл-36% мдйщреъ сшип дщг бдщееад мрщйн щцое 13 щтеъ еотмд.
ма роца чщш бйп ощк цен дмймд мбйп дсйлеп мъоеъд. бресу, роца лй цен мймд ооещк йеъш дйд омеед бшоеъ роелеъ йеъш щм доевмебйп оселшш HbA1C ебощк щйрд ашек йеъш.
дзечшйн ослойн лй дашлъ цен дмймд тщейд мдееъ асишивйд фщеид мдфзъъ дсйлеп мдйщреъ сшип дщг, лащш ййълп ещйфеш байжеп дселш ебощк дщйрд дйрн дорврерйн дтеогйн ббсйс дчщш бйп ощк цен дмймд мбйп дфшеврежд мсшип дщг.
дтшъ дотшлъ: ъецаеъ озчш жд озжчеъ ъецаеъ озчшйн чегойн бреща цен есшип.
http://www.ncbi.nlm.nih.gov/pubmed/27032109
лзмч оозчш ачшай обечш (оай 2017), бозчш дрелзй рбгч дчщш бйп дщйрей босъ дщеоп длммйъ ае дбирйъ мбйп оггй сйлеп мсшип дщг.
бозчш рлмме 243 рщйн мазш вйм дотбш тн тегу ощчм, ащш дщъъфе бълрйъ дойетгъ мйшйгд щм 5-6 ч"в бощчм баоцтеъ гйаид бмбг (дфзъд щм 3,500 чмешйеъ мщбет) ае баоцтеъ гйаид бщймеб фтймеъ вефрйъ (4 щтеъ щбетйеъ – щтъййн айоеп олщйшйн ещтъййн дмйлд решгйъ бтцйоеъ бйрерйъ тг вбедд тн децад аршвийъ щм л-2,500 чмешйеъ мщбет едфзъд ъжеръйъ щм л-1,700 чмешйеъ мщбет). йтймеъ дълрйъ детшлд мазш 16 щбетеъ баоцтеъ огйгъ шоъ дешоерй дойп, оггйн гмчъййн, осъ дщеоп длммйъ (рбгчд ббгйчъ DEXA) еосъ дщеоп дбирй, дтешй едъек-бирй (рбгче ббгйчъ MRI), тн отчб мазш щрд осйен дозчш.
бозчш дрелзй роца лй щйфеш бшоъ дасишгйем дзефщй, SHBG (ебщое дома: sex hormone binding globulin), мфийп еагйферчийп дйе чщешйн бйшйгд босъ дщеоп длммй; щйфеш бшоъ дисиесишеп дзефщй дйд чщеш бйшйгд бшоъ дщеоп дбирй дъъ-тешй; ещйфеш боггй дгмчъ CRP е- IL-6 дйд чщеш бйшйгд бшоъ дщеоп дъек-бирй (дчщшйн тбеш агйферчийп е- IL-6 дйе чирйн ема оебдчйн сиийсийъ).
олап, аеорн йгет лй дщеоп дбирй чщеш бсйлеп оевбш мосфш озмеъ лшерйеъ, аемн ооцай дозчш ошайн лй гееча йшйгд бщеоп длммй бвеу дйрд ощотеъйъ йеъш мщйфеш дфшефйм ддешоермй дчщеш бдъфъзеъ сшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/28512158
рйъез шишесфчийбй щм ръерй озчш обечш (сфиобш 2015) ащш ретг мбзеп аъ дчщш бйп ойгъ ддщорд мбйп сйлейй ддйщшгеъ бчшб 3,754 земеъ сшип щг оечгн дроцаеъ бсйлеп вбед.
йгет лй мземеъ тн дщоръ йъш фшеврежд фзеъ иебд бдщееад мземеъ бощчм ъчйп аемн айп тгейеъ мвбй ддщфтд щм ойгъ ддщорд. дзечшйн бзре аъ дчщш бйп BMI мбйп щйтеш ддйщшгеъ длммй ещйтеш ддйщшгеъ мма озмд.
роца лй щйтеш ддйщшгеъ дйд вшет йеъш брщйн тн дщоръ йъш зоешд (BMI отм 40), бойезг брщйн тн сшип щмймй мчемирйн дешоермййн. ма роца дбгм бщйтешй ддйщшгеъ бйп рщйн тн дщоръ йъш етегу ощчм мбйп рщйн бощчм ъчйп еъъ-ощчм.
http://www.ncbi.nlm.nih.gov/pubmed/26385214
озчш аешк (аевеси 2016) щретг мдтшйк дан чййн чщш бйп осфш щреъ тегу дощчм едщореъ мбйп дсйлеп мсшип бчшб рщйн. бдъбсс тм ръерйн щрасфе босвшъ озчш течбд вгем дтесч ббшйаеъ дайщд, бозчш дрелзй рлмме л-74,000 рщйн мазш вйм дотбш, щма дйе земеъ бсшип бъзймъ дозчш етбешп чййойн ръерй BMI омфзеъ 3 рчегеъ жоп.
дзечшйн дтшйле тбеш лм айщд аъ ощк дщрйн доцибш щм тегу дощчм едщореъ ъек дъййзсеъ мойгън (бгеод мзйщеб щм "щреъ чефсд" бдъййзс мтйщеп). тм бсйс ръерйн амд оцае дзечшйн лй рщйн тн йеъш щреъ тегу ощчм дйе бсйлеп вбед йеъш мсевй сшип дчщешйн бдщорд, лемм отй, фй дибтъ, лбг, лйс ошд, мбмб, щг, шзн, щзмеъ, лмйеъ ебмеиъ дъшйс.
баефп сфцйфй роца лй дсйлеп дйд вбед б-7% тбеш лм 10 щреъ тегу ощчм (5% бдъййзс мсшип дщг е-17% бдъййзс мсшип дшзн, тн сйлеп вбед йеъш ллм щойгъ ддщорд дййъд вбедд йеъш). дсйлеп дйд ощотеъй йеъш бчшб рщйн щотемн ма риме ийфем дешоермй. мошеъ щогебш бозчш ъцфйъй щайре оафщш мдсйч тм сйбъйеъ ае мвбщ домцеъ чмйрйеъ, ооцайн амд оцбйтйн тм лк щщойшд тм ощчм ъчйп тщейд мдйеъ ощотеъйъ борйтъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/27529652
босвшъ озчш ъцфйъй вгем (фбшеаш 2017) дтесч ббшйаеъ дайщд, бозчш дрелзй бгче дзечшйн аъ дчщш бйп йшйгд бощчм мбйп дсйлеп мсшип дшзн.
бозчш рлмме 36,794 рщйн мазш вйм дотбш бвймай 50-79, лащш дръерйн даръшефеоишййн рогге бъзймъ дозчш емазш 3 щрйн. дзечшйн сйееве аъ дощъъфеъ м-3 чивешйеъ бдъан мщйрей бощчм бъчефд же: ощчм йцйб (тг 5% щйрей), йшйгд бощчм (йшйгд щм отм 5%) ае тмййд бощчм (тмййд щм отм 5%) едщйрей девгш л"олееп" ае "бмъй олееп" бдъан мгйеез дощъъфеъ. бъчефъ отчб ресфъ щм 11.4 щрйн бооецт, 566 одрщйн аебзре тн сшип дшзн.
роца лй бдщееад мрщйн тн ощчм йцйб, рщйн щйшге бощчм дйе бсйлеп роек б-29% мсшип дшзн. дйшйгд бсйлеп дййъд бемиъ бойезг бчшб рщйн тн щореъ, ащш йшге бощчм баефп олееп. тмййд бощчм (отм 4.5 ч"в) дййъд чщешд бсйлеп вбед йеъш, бойезг бчшб рщйн щайрп реимеъ ийфем дешоермй.
https://www.ncbi.nlm.nih.gov/pubmed/28165909
бозчш ъцфйъй (йреаш 2017) рзчш дчщш бйп аешз дзййн едъжерд мбйп дъсоеръ доибемйъ бчшб земй сшип чемешчимй.
бозчш рлмме 143 земйн, ащш сееве мщъй чбецеъ - тн ае бмй дъсоеръ доибемйъ. орйъез ръерй аешз дзййн едъжерд щм дощъъфйн темд лй дземйн тн дъсоеръ доибемйъ рие мдйеъ цтйшйн йеъш, бтмй BMI вбед йеъш емцшек шод вбед йеъш щм чмешйеъ, змбеп, щеорйн, сйгп ежшзп ешод роелд йеъш щм биа-чшеип, ейиойп C езеоцд фемйъ.
брйъез сиийсий, ошайн дзечшйн лй шод вбедд йеъш щм BMI ещм цшйлъ амледем, щеорйн ещеоп шеей чщешд бсйлеп вбед йеъш мъсоеръ доибемйъ, бтег щцшйлъ сйбйн, ейиойп C езеоцд фемйъ чщешд бсйлеп роек йеъш. дзечшйн ослойн лй боишд морет дъфъзеъ ъсоеръ оибемйъ емщфш аъ оцбн дбшйаеъй щм земй сшип чемешчимй, оеомх мдгвйщ аъ дзщйбеъ щм щойшд тм ощчм ъчйп еъжерд оаежръ.
https://www.ncbi.nlm.nih.gov/pubmed/28168180
бсчйшд (фбшеаш 2017) очйфд щм счйшеъ щйиъйеъ еоид-армйжеъ добессеъ тм озчшйн ъцфйъййн, отшйлйн дзечшйн аъ зежч еъечу дтгейеъ бревт мчщш бйп дщорд мбйп дсйлеп мъзмеад ае мъоеъд осшип.
бсчйшд рлмме 204 оид-армйжеъ бдп рбгче дчщшйн бйп щбтд оггйн щерйн щм дщорд мбйп дсйлеп мъзмеад емъоеъд о-36 севй сшип. тм бсйс ръерйн амд ослойн дзечшйн лй йщрп тгейеъ зжчеъ бшоъ бйизеп вбедд, дъеолеъ блк щчййн чщш бйп дщорд мбйп азг тщш севй сшип: еещи, ойамеод рфецд, чйбд, отй, фй дибтъ, гшлй дошд, мбмб, щг, шзн, щзмеъ елмйеъ. чщшйн ресфйн щроцае айрн бшоъ бйизеп осфчъ тм оръ мчбет осчрд зг ощотйъ.
https://www.ncbi.nlm.nih.gov/pubmed/28246088
бге"з озчшй (2017), щфешсн тм йгй щрй вефй озчш вгемйн дтесчйн бзчш озмъ дсшип, оецвеъ дтгейеъ дтглрйеъ бревт мчщш бйп ъжерд, фтймеъ вефрйъ еоггйн аръшефеоишййн мбйп сшип дщг.
длеъбйн оцййрйн лй сшип дщг дйре дсшип дщлйз бйеъш бчшб рщйн, лащш б-2012 аебзре бшзбй дтемн 1.7 оймйеп очшйн згщйн, додеейн лшбт олмм очшй дсшип бчшб рщйн. осчреъ дгез обессеъ тм 119 озчшйн щртшле бшзбй дтемн длеммйн мотмд о-12 оймйеп рщйн ейеъш о-260,000 очшй сшип дщг.
дооцайн дтйчшййн бдъййзс мсшип дщг мфрй вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: дчфгд тм фтймеъ вефрйъ рошцъ, тегу ощчм ае щореъ бвйм цтйш (18-30) ебъчефъ дбвшеъ (тегу ощчм бъчефъ дймгеъ ебвйм ддъбвшеъ чщеш бцойзд айийъ йеъш ебшод роелд йеъш щм вешн вгймд елп вешн мдъоййреъ оечгоъ щм шчоъ дщг щреид фзеъ мъдмйлйн сширййн. бресу тегу ощчм чщеш бшоеъ роелеъ йеъш щм дешоерйн щзмъййн) едрчд; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: цшйлъ амледем евешойн дъфъзеъййн доебймйн мчеод вбедд емощчм мйгд вбед йеъш.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - ER negative), цшйлъ ожереъ долймйн чшеиреайгйн, цшйлъ оецшй змб, цшйлъ ъжерд тщйшд бсйгп ещойшд тм аешз зййн фтйм.
дооцайн дтйчшййн бдъййзс мсшип дщг мазш вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: щойшд тм аешз зййн фтйм (лемм дчфгд тм фтймеъ вефрйъ рошцъ), дрчд етегу ощчм ае щореъ бвймай 18-30; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: тегу ощчм ае щореъ бъчефъ дбвшеъ мфрй вйм дотбш, тмййд бощчм бъчефъ дбвшеъ, вешойн дъфъзеъййн доебймйн мчеод вбедд ецшйлъ амледем.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - (ER negative, цшйлъ ожереъ долймйн чшеиреайгйн ецшйлъ ъжерд тщйшд бсйгп.
дзечшйн оцййрйн лй ооцай дге"з айрн леммйн аъ двешойн дбайн щроцае чщешйн бсйлеп оевбш мдъфъзеъ сшип дщг:
- айшетй зййн дчщешйн бзщйфд вбедд йеъш масишевп ефшевсишеп лемм: дефтъ озжеш деесъ мфрй вйм 12, лрйсд мвйм дотбш мазш вйм 55, ай-дбаъ ймгйн мтемн едшйеп шащеп мазш вйм 30.
- зщйфд мчшйрд бодмк ийфемйн шфеаййн, бойезг бвйм ддъбвшеъ.
- ийфем дешоермй змйфй ещйоещ бвмемеъ морйтъ дшйеп.
ддомцеъ длммйеъ дтемеъ одге"з дйрп щойшд тм ощчм ъчйп, дчфгд тм аешз зййн фтйм, цшйлъ ъжерд бшйад едвбмъ цшйлъ амледем.
http://www.aicr.org/continuous-update-project/breast-cancer.html
рййш тогд (аевеси 2016) щфешсн тм йгй фарм оеозйн оитн дшщеъ дбйрмаеойъ мзчш дсшип (IARC) дтесч бчщш бйп дщорд едсйлеп мсшип. ддтшлд дйа лй бщръ 2013-2014, бшод двмебмйъ, 10.8% одвбшйн, 14.9% одрщйн е-5.0% одймгйн сбме одщоръ йъш (BMI>30).
доеозйн оцййрйн лй дщорд етмййд бощчм маешк дзййн ъмеййн бойгд шбд бвешойн дрйърйн мщмйид ещйрей, бйрйдн шоъ дцшйлд дчмешйъ ебйцет фтймеъ вефрйъ. доеозйн айщще аъ дооцайн дчегойн ощръ 2002, дошайн лй мщойшд тм ощчм ъчйп ъфчйг борйтъ зойщд севй сшип: отй, ещи, лмйеъ, щг (мазш вйм дотбш) ешзн.
брййш дтогд дрелзй, добесс тм мотмд о-1,000 озчшйн афйгойемевййн, оесйфйн доеозйн тег 8 севй сшип мшщйод же: чйбд, лбг, лйс ошд, мбмб, щзмеъ, бмеиъ дъшйс, оез (орйрвйеод) еойамеод рфецд. бресу, йщрп тгейеъ мвбй дчщш м-3 севй сшип ресфйн: тшоерйъ, щг (бвбшйн) емйофеод.
дн ослойн лй дтгш щеоп веу тегу офзйъ аъ дсйлеп мошбйъ севй дсшип. бресу, оозчшйн фшд-чмйрййн темд лй йшйгд олееръ бощчм тщейд мдйеъ бтмъ дщфтд овйрд офрй дъфъзеъ сшип аемн ргшщйн озчшйн чмйрййн ббрй агн тм оръ мащщ ооцайн амд.
http://www.ncbi.nlm.nih.gov/pubmed/27557308
бозчш врий (ошх 2016) щлмм ръерйн щм л- 22,000 земй сшип дтшоерйъ мтеоъ чбецъ дщееад щм л-22,000 ощъъфйн бшйайн роцад ъойлд роелд млк щшоеъ вбедеъ йеъш щм LDL еишйвмйцшйгйн овбйшеъ аъ дсйлеп мсшип тшоерйъ авшсйбй.
http://www.ncbi.nlm.nih.gov/pubmed/26992435
оозчшйн афйгойемевййн дбезрйн аъ дчщш бйп цшйлъ щеоп едщорд мбйп дсйлеп мсшип дщг темйн ооцайн сеъшйн. млп, дозчш дрелзй (аечиебш 2013) бецт тм тлбшй отбгд, гбш доафщш мбзеп аъ ддщфтд щм гйаид тъйшъ щеоп баефп бмъй ъмей бдщорд ебдъфъзеъ ъсоеръ оиабемйъ. чбецъ тлбшйн азъ чйбмд гйаид гмъ щеоп (12% одчмешйеъ) едчбецд дщрййд чйбмд гйаид тъйшъ щеоп (60% одчмешйеъ). ъецаеъ дозчш ошаеъ лй цшйлд вбедд щм щеорйн, вн ан айрд омеед бдщорд, вешоъ мтмййд бъдмйлйн гмчъййн ебщйреййн вриййн ббмеиеъ дзмб ащш тщеййн мдайх дъфъзеъ ъдмйлйн сширййн бщмб оаезш йеъш. дзечшйн оцййрйн лй дщфтд же тщейд мдйеъ чбетд еашелъ иеез, вн мазш отбш мгйаид гмъ щеоп бщмб оаезш йеъш. аеорн ргшщйн озчшйн чмйрййн тм оръ мбсс аъ дооцайн, ак озчш жд ощотеъй бдгвщъ ддщмлеъ ашелеъ диеез бцшйлд тегфъ щм щеорйн бвйм цтйш.
http://www.ncbi.nlm.nih.gov/pubmed/24156623
бозчш (2020) щртшк бчшб олшсойн, роца лй ъжерд тъйшъ щеоп ещореъ оебймд мщйреййн оибемййн бъайн сширййн, еблк февтъ бъфчег отшлъ дзйсеп еоайцд аъ дъфъзеъ двйгем дсширй.
https://pubmed.ncbi.nlm.nih.gov/33301708/
озчш (оай 2016) ащш безп одн дорврерйн дбйемевййн дтеогйн ббсйс ддщфтд щм дщорд тм дъфъзеъ сшип дмбмб баоцтеъ щйоещ боегмйн щм зйеъ отбгд еббгйчеъ чмйрйеъ щм земй сшип дмбмб.
озчшйн чегойн ошайн лй ъдмйлй гсоефмжйд (дйеецшеъ тегфъ щм шчоъ зйбеш боишйцд дзех-ъайъ) дйрн вешн довбйш дъфъзеъ ъайн сширййн еовбйш тойгеъ млйоеъшфйд.
бозчш дрелзй рбгч лйцг дщорд овбйшд ъдмйлйн гмчъййн егсоефмжйд. босвшъ дозчш дзечшйн бгче аъ ддщфтд щм дщорд тм оафййрй двйгем едъфщиеъе етм дъвебд мийфем боегмйн щм тлбшйн тн сшип дмбмб осев PDAC еайщще аъ дооцайн тм йгй рйъез шчоеъ сширйеъ щм земй сшип дмбмб.
дн ошайн лйцг дайришачцйд бйп ъай дщеоп, ъайн зйсерййн еъай шчоъ зйбеш бземйн тн дщоръ йъш йецшъ сбйбд доафщшъ дъфъзеъ щм двйгем дсширй езесоъ аъ лрйсъ длйоеъшфйд мъайн, еоцйтйн лй баоцтеъ ийфем арий-фйбшеий еарий-гмчъй рйъп мщфш аъ дъвебд мийфем бземй сшип мбмб осев PDAC тн дщоръ йъш.
http://www.ncbi.nlm.nih.gov/pubmed/27246539
озчш (фбшеаш 2016) щртшк тм зйеъ отбгд дбезп одн дорврерйн бдн дщорд оайцд ъдмйлйн сширййн.
дзечшйн осбйшйн лй дщоръ йъш чщешд бдъфъзеъ одйшд йеъш щм сшип дмбмб есшип дщг аемн дорврерйн дтеогйн ббсйс чщш жд айрн бшешйн.
бозчш дрелзй рбгч дъфчйг щм вешой двгймд PlGF/VEGFR-1 беейсеъ дчщш бйп дщорд еъдмйлйн сширййн.
боегм тлбшйн ебгвйоеъ ъайн арещййн роца лй дщоръ йъш двбйшд згйшд щм очшефавйн дчщешйн бвйгемйн (TAM), дъфщиеъ двйгем едъфъзеъ вшешеъ, лащш орйтъ дфтймеъ щм VEGFR-1 тцшд дщфтд жаъ едвбйшд аъ дфтймеъ дарий-сширйъ.
тег ошайн дзечшйн лй дщоръ йъш омеед бшоеъ оевбшеъ щм PlGF ещйоещ боифешойп ъшн майжеп шоеъ дайрсемйп емдвбшъ дфтймеъ дзйсерйъ дарий-сширйъ.
дзечшйн осйчйн лй тм йгй дщфтд тм дфтймеъ щм вешой двгймд рйъп мдщфйт тм дсбйбд дзйсерйъ щм двйгем еморет дацъ ъдмйлйн сширййн дчщешйн бдщорд.
http://www.ncbi.nlm.nih.gov/pubmed/26861455
озчш отбгд (йреаш 2016) дошад лй шчоъ дщеоп дочйфд аъ бмеиъ дтшоерйъ овбйшд аъ ддъфщиеъ щм ъайн сширййн озех мтшоерйъ емлп сшип дтшоерйъ тмем мдйеъ авшсйбй йеъш бземйн тн дщоръ йъш.
http://www.ncbi.nlm.nih.gov/pubmed/26756352
боид-армйжд (оай 2017) рбгч дчщш бйп щореъ ефйжеш дщеоп бвеу мбйп дъфъзеъ сшип дчщеш бщореъ (лемм сшип щг мазш вйм дотбш, чемешчимй, еещи ъзъеп, чйбд тмйерд, лбг, лйс ошд, мбмб, шйшйъ дшзн, щзмеъ елмйеъ).
бозчш рлмме дръерйн ощбтд озчшй течбд щбецте байшефд, бдн 18,688 вбшйн е-24,751 рщйн бвйм 62 е-63 бооецт. бодмк ъчефъ отчб щм л-12 щрд аебзре 1,656 очшйн щм сшип дчщеш бщореъ.
брйъез лемм щм дръерйн роца лй тмййд боггйн даръшефеоишййн - BMI, дйчу оеърййн, дйчу йшлййн ейзс оеърййн мйшлййн - дййъд чщешд бсйлеп вбед йеъш мсшип (сйлеп вбед б-11%, 13%, 9% е-15%, бдъаод, тбеш лм тмййд щм сиййъ ъчп азъ). бдъййзс мсшип чемешчимй, дщереъ бйп дозчшйн дййъд роелд ероца лй тмййд б-BMI, дйчу оеърййн, дйчу йшлййн ейзс оеърййн мйшлййн дййъд чщешд бсйлеп вбед б-16%, 21%, 15% е-20%, бдъаод. бдъййзс мсшип дщг мазш вйм дотбш, роца лй дчщш дйд ъмей бийфем дешоермй змйфй, лк щрщйн щотемн ма риме ийфем дешоермй дйе бсйлеп вбед йеъш.
дзечшйн ослойн лй баефп лммй ооцай дозчш огвйщйн аъ дзщйбеъ щм щойшд тм ощчм веу ъчйп морйтъ сшип, баефп бмъй ъмей бвйм ае бойп.
https://www.ncbi.nlm.nih.gov/pubmed/28441380
бгез (2017) оитн дошлж даошйчай мбчшъ озмеъ (CDC) огеез лй баефп лммй щйтеш очшй дсшип дчщешйн бщореъ (омбг сшип чемешчимй) роца бовоъ тмййд оаж щръ 2005, жаъ мошеъ дйшйгд длммйъ бщйтеш очшй дсшип.
https://www.cdc.gov/mmwr/volumes/66/wr/mm6639e1.htm?s_cid=mm6639e1_e
бозчш ъцфйъй (ребобш 2017) шзб дйчу бгче дзечшйн оде щйтеш очшй дсшип бшзбй дтемн аеъе рйъп мййзс мселшъ емтегу ощчм. бозчш ртщд щйоещ бръерйн о-175 огйреъ бдъййзс м-12 севй сшип, тм оръ мдтшйк оде щйтеш очшй дсшип бщръ 2012 аеъе рйъп мййзс мдйоцаеъ селшъ етегу ощчм (BMI отм 25) 10 щрйн оечгн йеъш.
дзечшйн отшйлйн лй рйъп мййзс л-5% олм очшй дсшип бщръ 2012 мдщфтд щм дйоцаеъ селшъ ещм тегу ощчм бщръ 2002, ръеп щеед тшк м-627 тг 793 аму очшй сшип згщйн. бдъййзс мсевй сшип сфцйфййн, мдтшлъ дзечшйн рйъп мййзс 24.5% оочшй сшип длбг е-38.4% оочшй сшип дшзн мщрй вешой сйлеп амд.
брйъез щрй вешой дсйлеп баефп бмъй ъмей, ддтшлд дйа щтегу ощчм чщеш бфй 2 очшй сшип бдщееад мселшъ. бресу, дзечшйн ошайн лй рйъп мййзс 26.1% оочшй дсшип дчщешйн бселшъ е-31.9% оочшй дсшип дчщешйн бтегу ощчм мовоъ дтмййд бочшй дселшъ етегу дощчм бйп дщрйн 1980-2002. дзечшйн ослойн лй рйъп мййзс змч рйлш оочшй дсшип мселшъ емтегу ощчм, емлп тн дтмййд бдйоцаеъ вешой сйлеп амд йщ мбзеп лйцг рйъп бшод дчмйрйъ ебшоъ бшйаеъ дцйбеш мждеъ одп асишивйеъ дорйтд едабзеп дп бшоъ даелмесййд длммйъ едп бшоъ доиефм дфширй.
http://www.thelancet.com/journals/landia/article/PIIS2213-8587(17)30366-2/fulltext
зжшд мъзймъ дозчшйн
вешой сйлеп - сеМлшъ
озчш течбд (ошх 2016) щретг мбзеп аъ дчщш бйп ощк цен дмймд мбйп щйтеш ддйщреъ едъоеъд бчшб рщйн тн сшип дщг, елп жйдей вешой дсйлеп мъецаеъ щмймйеъ афщшйеъ, лемм ощч дселш (HbA1c), гмчъ отшлъйъ (CRP), дщорд еощк дщйрд.
ъецаеъ озчшйн чегойн, щбецте бзйеъ отбгд, дшае лй цен ооещк бодмк дщйрд дйд бтм дщфтд ойийбд тм дфзъъ ъдмйлйн сширййн еъдмйлйн оибемййн дчщешйн бсшип дщг.
бозчш дрелзй рлмме ръерйн щм 2,413 земеъ сшип дщг бщмбйн оечгойн, щайрп земеъ селшъ, бреъ 27-70 бтъ дабзеп. дзечшйн дтшйле аъ ощк цен дмймд баоцтеъ йеорй алймд щм 24 щтеъ щрасфе бъзймъ дозчш, мазш щрд емазш 4 щрйн.
одъецаеъ темд лй цен мймд щм фзеъ о-13 щтеъ дйд омеед бсйлеп вбед бл-36% мдйщреъ сшип дщг бдщееад мрщйн щцое 13 щтеъ еотмд.
ма роца чщш бйп ощк цен дмймд мбйп дсйлеп мъоеъд. бресу, роца лй цен мймд ооещк йеъш дйд омеед бшоеъ роелеъ йеъш щм доевмебйп оселшш HbA1C ебощк щйрд ашек йеъш.
дзечшйн ослойн лй дашлъ цен дмймд тщейд мдееъ асишивйд фщеид мдфзъъ дсйлеп мдйщреъ сшип дщг, лащш ййълп ещйфеш байжеп дселш ебощк дщйрд дйрн дорврерйн дтеогйн ббсйс дчщш бйп ощк цен дмймд мбйп дфшеврежд мсшип дщг.
дтшъ дотшлъ: ъецаеъ озчш жд озжчеъ ъецаеъ озчшйн чегойн бреща цен есшип.
http://www.ncbi.nlm.nih.gov/pubmed/27032109
бозчш ъцфйъй (йреаш 2017) рзчш дчщш бйп аешз дзййн едъжерд мбйп дъсоеръ доибемйъ бчшб земй сшип чемешчимй.
бозчш рлмме 143 земйн, ащш сееве мщъй чбецеъ - тн ае бмй дъсоеръ доибемйъ. орйъез ръерй аешз дзййн едъжерд щм дощъъфйн темд лй дземйн тн дъсоеръ доибемйъ рие мдйеъ цтйшйн йеъш, бтмй BMI вбед йеъш емцшек шод вбед йеъш щм чмешйеъ, змбеп, щеорйн, сйгп ежшзп ешод роелд йеъш щм биа-чшеип, ейиойп C езеоцд фемйъ.
брйъез сиийсий, ошайн дзечшйн лй шод вбедд йеъш щм BMI ещм цшйлъ амледем, щеорйн ещеоп шеей чщешд бсйлеп вбед йеъш мъсоеръ доибемйъ, бтег щцшйлъ сйбйн, ейиойп C езеоцд фемйъ чщешд бсйлеп роек йеъш. дзечшйн ослойн лй боишд морет дъфъзеъ ъсоеръ оибемйъ емщфш аъ оцбн дбшйаеъй щм земй сшип чемешчимй, оеомх мдгвйщ аъ дзщйбеъ щм щойшд тм ощчм ъчйп еъжерд оаежръ.
https://www.ncbi.nlm.nih.gov/pubmed/28168180
бозчш ъцфйъй (афшйм 2017), добесс тм ръерйн щрасфе бйп дщрйн 1998-2010, ошайн дзечшйн лй земй селшъ сев 2 дйе бсйлеп вбед бл-30% мсшип чемешчимй, бойезг бщщъ дзегщйн щмазш абзеп дселшъ. дсйлеп дйд вбед бойезг (фй 2) бчшб вбшйн тг вйм 55, лмеош мфрй двйм бе рдев мбцт бгйчеъ счш.
https://www.ncbi.nlm.nih.gov/pubmed/28436468
бозчш ъцфйъй (ребобш 2017) шзб дйчу бгче дзечшйн оде щйтеш очшй дсшип бшзбй дтемн аеъе рйъп мййзс мселшъ емтегу ощчм. бозчш ртщд щйоещ бръерйн о-175 огйреъ бдъййзс м-12 севй сшип, тм оръ мдтшйк оде щйтеш очшй дсшип бщръ 2012 аеъе рйъп мййзс мдйоцаеъ селшъ етегу ощчм (BMI отм 25) 10 щрйн оечгн йеъш.
дзечшйн отшйлйн лй рйъп мййзс л-5% олм очшй дсшип бщръ 2012 мдщфтд щм дйоцаеъ селшъ ещм тегу ощчм бщръ 2002, ръеп щеед тшк м-627 тг 793 аму очшй сшип згщйн. бдъййзс мсевй сшип сфцйфййн, мдтшлъ дзечшйн рйъп мййзс 24.5% оочшй сшип длбг е-38.4% оочшй сшип дшзн мщрй вешой сйлеп амд.
брйъез щрй вешой дсйлеп баефп бмъй ъмей, ддтшлд дйа щтегу ощчм чщеш бфй 2 очшй сшип бдщееад мселшъ. бресу, дзечшйн ошайн лй рйъп мййзс 26.1% оочшй дсшип дчщешйн бселшъ е-31.9% оочшй дсшип дчщешйн бтегу ощчм мовоъ дтмййд бочшй дселшъ етегу дощчм бйп дщрйн 1980-2002. дзечшйн ослойн лй рйъп мййзс змч рйлш оочшй дсшип мселшъ емтегу ощчм, емлп тн дтмййд бдйоцаеъ вешой сйлеп амд йщ мбзеп лйцг рйъп бшод дчмйрйъ ебшоъ бшйаеъ дцйбеш мждеъ одп асишивйеъ дорйтд едабзеп дп бшоъ даелмесййд длммйъ едп бшоъ доиефм дфширй.
http://www.thelancet.com/journals/landia/article/PIIS2213-8587(17)30366-2/fulltext
зжшд мъзймъ дозчшйн
вешой сйлеп - вДйм дотбш
озчш (йемй 2016), добесс тм ръерйн щрасфе бозчш течбд бшйий ршзб, дтшйк аъ дсйлеп мсшип дщг бчшб рщйн мазш вйм дотбш, тбешп йщрн ръерйн огейчйн мвбй длрйсд мвйм дотбш. лое лп, дозчш безп одй ойгъ ддийд бозчшйн бдн айп ръерйн огейчйн бревт мщйоещ бийфем дешоермй емлрйсд мвйм дотбш.
оъек дрщйн щвейсе мозчш бйп дщрйн 2003-2009, бъчефъ отчб щм 6 щрйн, 58,148 рщйн рлрсе мвйм дотбш, лащш оъек 39,183 рщйн, щмвбйдп йщ ръерйн огейчйн мвбй длрйсд мвйм дотбш, 775 аебзре тн сшип дщг.
роца лй дсйлеп дйзсй мсшип дщг, бчшб рщйн щриме ийфем дешоермй (асишевп + фшевсишеп) бдщееад мрщйн щма риме ийфем дешоермй, дйд 2.74 тбеш щйоещ щм л-5.4 щрйн, есйлеп йзсй щм 3.74 тбеш щйоещ щм 15 щрд еотмд.
дзечшйн отшйлйн лй йщрд дтшлъ зсш щм 53% бшоъ дсйлеп бозчшйн бдн ма бецт тглеп мвбй дщйоещ бийфем дешоермй бодмк дозчш, дтшлъ зсш щм 13% бозчшйн бдн рлмме рщйн мма ръерйн огейчйн мвбй длрйсд мвйм дотбш едтшлъ зсш щм 59% бозчшйн бдн щрй ощърйн амд ма дйе отеглрйн ае огейчйн.
осчръ дозчш дйа щтм фй ръерйн амд, щйоещ бийфем дешоермй длемм шч асишевп ма роца чщеш мсйлеп мсшип дщг ещйоещ бийфем дешоермй длемм асишевп ефшевсишеп чщеш бтмййд бсйлеп мсшип дщг бойгд вбедд оже щрдев мдтшйк, лащш дсйлеп вбед йеъш ллм щдщйоещ ооещк йеъш.
http://www.ncbi.nlm.nih.gov/pubmed/27467055
озчш аешк (аевеси 2016) щретг мдтшйк дан чййн чщш бйп осфш щреъ тегу дощчм едщореъ мбйп дсйлеп мсшип бчшб рщйн. бдъбсс тм ръерйн щрасфе босвшъ озчш течбд вгем дтесч ббшйаеъ дайщд, бозчш дрелзй рлмме л-74,000 рщйн мазш вйм дотбш, щма дйе земеъ бсшип бъзймъ дозчш етбешп чййойн ръерй BMI омфзеъ 3 рчегеъ жоп.
дзечшйн дтшйле тбеш лм айщд аъ ощк дщрйн доцибш щм тегу дощчм едщореъ ъек дъййзсеъ мойгън (бгеод мзйщеб щм "щреъ чефсд" бдъййзс мтйщеп). тм бсйс ръерйн амд оцае дзечшйн лй рщйн тн йеъш щреъ тегу ощчм дйе бсйлеп вбед йеъш мсевй сшип дчщешйн бдщорд, лемм отй, фй дибтъ, лбг, лйс ошд, мбмб, щг, шзн, щзмеъ, лмйеъ ебмеиъ дъшйс.
баефп сфцйфй роца лй дсйлеп дйд вбед б-7% тбеш лм 10 щреъ тегу ощчм (5% бдъййзс мсшип дщг е-17% бдъййзс мсшип дшзн, тн сйлеп вбед йеъш ллм щойгъ ддщорд дййъд вбедд йеъш). дсйлеп дйд ощотеъй йеъш бчшб рщйн щотемн ма риме ийфем дешоермй. мошеъ щогебш бозчш ъцфйъй щайре оафщш мдсйч тм сйбъйеъ ае мвбщ домцеъ чмйрйеъ, ооцайн амд оцбйтйн тм лк щщойшд тм ощчм ъчйп тщейд мдйеъ ощотеъйъ борйтъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/27529652
бге"з озчшй (2017), щфешсн тм йгй щрй вефй озчш вгемйн дтесчйн бзчш озмъ дсшип, оецвеъ дтгейеъ дтглрйеъ бревт мчщш бйп ъжерд, фтймеъ вефрйъ еоггйн аръшефеоишййн мбйп сшип дщг.
длеъбйн оцййрйн лй сшип дщг дйре дсшип дщлйз бйеъш бчшб рщйн, лащш б-2012 аебзре бшзбй дтемн 1.7 оймйеп очшйн згщйн, додеейн лшбт олмм очшй дсшип бчшб рщйн. осчреъ дгез обессеъ тм 119 озчшйн щртшле бшзбй дтемн длеммйн мотмд о-12 оймйеп рщйн ейеъш о-260,000 очшй сшип дщг.
дооцайн дтйчшййн бдъййзс мсшип дщг мфрй вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: дчфгд тм фтймеъ вефрйъ рошцъ, тегу ощчм ае щореъ бвйм цтйш (18-30) ебъчефъ дбвшеъ (тегу ощчм бъчефъ дймгеъ ебвйм ддъбвшеъ чщеш бцойзд айийъ йеъш ебшод роелд йеъш щм вешн вгймд елп вешн мдъоййреъ оечгоъ щм шчоъ дщг щреид фзеъ мъдмйлйн сширййн. бресу тегу ощчм чщеш бшоеъ роелеъ йеъш щм дешоерйн щзмъййн) едрчд; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: цшйлъ амледем евешойн дъфъзеъййн доебймйн мчеод вбедд емощчм мйгд вбед йеъш.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - ER negative), цшйлъ ожереъ долймйн чшеиреайгйн, цшйлъ оецшй змб, цшйлъ ъжерд тщйшд бсйгп ещойшд тм аешз зййн фтйм.
дооцайн дтйчшййн бдъййзс мсшип дщг мазш вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: щойшд тм аешз зййн фтйм (лемм дчфгд тм фтймеъ вефрйъ рошцъ), дрчд етегу ощчм ае щореъ бвймай 18-30; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: тегу ощчм ае щореъ бъчефъ дбвшеъ мфрй вйм дотбш, тмййд бощчм бъчефъ дбвшеъ, вешойн дъфъзеъййн доебймйн мчеод вбедд ецшйлъ амледем.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - (ER negative, цшйлъ ожереъ долймйн чшеиреайгйн ецшйлъ ъжерд тщйшд бсйгп.
дзечшйн оцййрйн лй ооцай дге"з айрн леммйн аъ двешойн дбайн щроцае чщешйн бсйлеп оевбш мдъфъзеъ сшип дщг:
- айшетй зййн дчщешйн бзщйфд вбедд йеъш масишевп ефшевсишеп лемм: дефтъ озжеш деесъ мфрй вйм 12, лрйсд мвйм дотбш мазш вйм 55, ай-дбаъ ймгйн мтемн едшйеп шащеп мазш вйм 30.
- зщйфд мчшйрд бодмк ийфемйн шфеаййн, бойезг бвйм ддъбвшеъ.
- ийфем дешоермй змйфй ещйоещ бвмемеъ морйтъ дшйеп.
ддомцеъ длммйеъ дтемеъ одге"з дйрп щойшд тм ощчм ъчйп, дчфгд тм аешз зййн фтйм, цшйлъ ъжерд бшйад едвбмъ цшйлъ амледем.
http://www.aicr.org/continuous-update-project/breast-cancer.html
зжшд мъзймъ дозчшйн
вешой сйлеп - озмеЙъ отшлъ дтйлем
счйшд щйиъйъ еоид армйжд очйфд длеммъ 24 озчшйн (йреаш 2016) оцбйтд тм лк щземйн щтбше ийфем мойвеш дзййгч дмйчебчиш фймешй дйе бсйлеп оефзъ мдъфъзеъ сшип дчйбд.
http://www.ncbi.nlm.nih.gov/pubmed/26836587
бозчш очшд-бчшд, (2019) ащш обесс тм ръерйн оозчш ачшай обечш вгем, щртшк бсйп, рлмме 229 ощъъфйн тн абзрд згщд щм сшип, амйдн деъаод чбецъ бйчешъ щм 229 ощъъфйн мма сшип. роца лй:
- шод вбедд йеъш бгн щм ейиойп E дййъд чщешд бсйлеп оефзъ мсшип ботшлъ дтйлем.
- шоъ ейиойп E вбедд дййъд чщешд бсйлеп оефзъ мсшип баефп лммй бчшб ощъъфйн тн шоъ смрйен вбедд, ак бсйлеп оевбш мсшип бчшб ощъъфйн тн шоъ смрйен роелд.
https://www.ncbi.nlm.nih.gov/pubmed/30713028
дфешоемд Shenling Baizhu San (бчйцеш: SBS) дйа фешоемд доелшъ бшфеад дсйрйъ мийфем бдфштеъ тйлем лбш оаеъ щрйн. дфешоемд олймд 10 цозй ошфа: Panax ginseng, Atractylodes macrocephala, Wolfiporia extensa, Glycyrrhiza glabra, Dioscorea opposite, Dolichos lablab, Nelumbinis Nucifera, Coix lacryma-jobi, Amomum, Platycodon grandifloras.
бозчш дрелзй (афшйм 2015), ащш ртшк бчшб зйеъ отбгд, оцйвйн дзечшйн одн орврерй дфтймеъ бдн дфешоемд ъешоъ мдфзъъ дъоеъд едъфъзеъ вйгемйн сширййн ботй лсйбек щм чемйийс.
http://www.ncbi.nlm.nih.gov/pubmed/25897964
зжшд мъзймъ дозчшйн
цшйлъ шлйбйн сфцйфййн
лммй | фйшеъ ейшчеъ | сйбйн ъжеръййн | гврйн омайн | ожеп оп дзй | аеЙовд 3 божеп | фДйиеасишеврйн
цшйлъ шлйбйн сфцйфййн - лммй
бсчйшд очйфд ощръ 2025 детшле дтгейеъ осчйшеъ щйиъйеъ щтсче бщйоещ лгбщ морйтд емийфем боечежйийс бфд тм шчт ийфемйн аерчемевййн.
дсчйшд лммд 12 счйшеъ щйиъйеъ щдъбссе тм сд"л 31 озчшйн чмйрййн, бдн дщъъфе обевшйн, брй ретш еймгйн.
ддътшбейеъ бозчшйн лмме щйоещ бгбщ осевйн щерйн, лийфем йзйг ае бщймеб ийфем ъшефъй.
бшеб дозчшйн дщйоещ ртщд лщийфъ фд бойреп щм 20 о"м, ан лй дйе дбгмйн бъгйшеъ, лащш бзмч одозчшйн ддътшбеъ рйърд мфрй еазшй ийфем дчшйрд, ебазшйн рйърд вн орд мфрй дщйрд ае щщ щтеъ мазш ийфем дчшйрд.
чбецеъ дбйчешъ чйбме ийфем сиргший, фмсбе ае ма чйбме дътшбеъ.
дооцайн оцбйтйн тм лк щщйоещ бгбщ тщей мдфзйъ аъ щйтеш ддефтд щм оечежйийс зоеш, мдчм тм лаб дозййб щйоещ бощллй лабйн, емцоцн аъ ддфштеъ бодмк дийфем даерчемевй.
тн жаъ, ма роцад тгеъ тчбйъ мйтймеъе бдфзъъ оечежйийс блмм гшвеъ дзеошд. дфтшйн бйп ъецаеъ дозчшйн тщеййн мрбет одбгмйн баелмесйеъ дрбгчеъ, бсевй дгбщ, бъжоеп ебощк ддътшбеъ.
лое лп, ма жедъд тгеъ оебдчъ мйтймеъ дгбщ боечежйийс дрвшн олйоеъшфйд, бтйчш бщм овбмеъ оъегемевйеъ.
дзечшйн ослойн лй ау щщйоещ бгбщ тщей мъшен бдфзъъ оечежйийс зоеш, бдчмъ лаб ебцоцен дфштеъ мийфем бчшб обевшйн дтебшйн ийфемй чшйрд, дтгейеъ мйтймеъе длммйъ айрп зг-ощотйеъ. ргшщйн озчшйн тъйгййн байлеъ вбедд, ъек щйоещ бфшеиечемйн азйгйн, едъййзсеъ мгшвъ оечежйийс, вйм доиефмйн есев дийфем даерчемевй.
https://pubmed.ncbi.nlm.nih.gov/40456333/
бсчйшд щйиъйъ еоид-армйжд ощръ 2025 детшк дчщш бйп цшйлъ ййп мбйп дсйлеп мдъфъзеъ сшип, ъек бзйръ ддбгмйн бйп ййп аген мййп мбп.
дзечшйн оцййрйн лй бтег щцшйлъ амледем роцад чщешд бсйлеп оевбш мсшип, йщрп тгейеъ дотйгеъ тм дщфтд ойийбд афщшйъ щм ййп аген. тн жаъ, дооцайн бревт мдбгмйн бйп ййп аген мййп мбп айрн тчбййн. дсчйшд лммд 42 озчшйн, одн 20 озчшй течбд е-22 озчшй очшд-бйчешъ.
дзечшйн бзре аъ дчщш бйп цшйлъ ййп мсйлеп мсшип бдщееад бйп дощъъфйн тн шоъ дцшйлд двбедд бйеъш щм цшйлъ ййп мбйп дшод дроелд бйеъш.
бдъбсс тм дръерйн щм 95,923 ощъъфйн, ма роца чщш оебдч бйп цшйлъ ййп баефп лммй мбйп дсйлеп мдъфъзеъ сшип, лащш дъецаеъ дйе геоеъ тбеш ййп аген еййп мбп брфшг. тн жаъ, роца лй цшйлъ ййп мбп дййъд чщешд бсйлеп вбед б-26% мсшип бчшб рщйн, елп бсйлеп вбед б-12% лащш рлмме озчшй течбд бмбг. брйъез мфй севй сшип щерйн, ддбгм дбеми бйп ййп аген мййп мбп роца бдчщш мсшип дтеш: цшйлъ ййп мбп дййъд чщешд бсйлеп вбед б-22%, бтег щмвбй ййп аген ма роца чщш оебдч. осчръ дзечшйн дйа лй баефп лммй ма роца дбгм ощотеъй бйп ййп аген мййп мбп бдчщш мсйлеп мсшип, ооца щоаъвш аъ дъфйсд дшеезъ мфйд ййп аген бшйа йеъш. тн жаъ, йщ мдощйк ембзеп аъ дсйлеп доевбш щроца бцшйлъ ййп мбп, бтйчш бчшб рщйн ебозчшй течбд.
https://pubmed.ncbi.nlm.nih.gov/39940392/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2020) детшлд ддщфтд щм цшйлъ авежй омк тм оггйн аръшефеоишййн. бсчйшд рлмме 27 озчшйн, бдн дщъъфе оъргбйн бшйайн ае ощъъфйн тн овееп оцбйн бшйаеъййн - лемм ъсоеръ оибемйъ, йъш щеорйн бгн, сшип, щореъ еселшъ сев 2. бозчшйн амд рбгчд ддщфтд щм ъесфъ авежй омк бойреп щрт бйп 15 м-108 вшн мйен мощк ъчефъ дътшбеъ щм щбетййн тг щръййн.
брйъез лемм щм дръерйн ма роцад дщфтд оебдчъ мцшйлъ авежй омк тм дйчу доеърййн, дощчм, д-BMI ае осъ дщеоп. брйъез ойреп-ъвебд роцае тгейеъ оевбмеъ млк щойреп щм тг 35 вшн мйен дйд омеед бйшйгд оебдчъ бощчм ебдйчу доеърййн. дзечшйн ослойн лй баефп лммй ма роцае тгейеъ обессеъ мдщфтд щм авежй омк тм доггйн даръшефеоишййн.
https://pubmed.ncbi.nlm.nih.gov/32444054/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ъцфйъййн,(2020) детшк дчщш бйп цшйлъ гврйн омайн еомеищйн ебйп дсйлеп мдъфъзеъ сшип. бсчйшд рлмме 17 оаошйн бдн ртшле оид-армйжеъ щм ръерйн оозчшй течбд еозчшй очшд-бчшд.
мдмп дооцайн дтйчшййн:
-
бдъййзс мъоеъд осшип: ръерйн ощбт оид-армйжеъ щм озчшй течбд, ошайн щцшйлд вбедд щм гврйн омайн чщешд бсйлеп роек б-6% тг 12% бдщееад мцшйлд роелд, ебсйлеп роек б-3% тг 20% тбеш ойреп щм 15-90 вшн/йен.
-
цшйлъ гврйн омайн роцад чщешд баефп тчбй бсйлеп роек йеъш мдйаштеъ щм сшип осев чемешчимй, отй, чйбд, мбмб еещи.
-
дтгейеъ бдъййзс мцшйлъ гврйн омеищйн дйрп оевбмеъ. мфй дтгейеъ дчййоеъ, цшйлд вбедд щм гврйн омеищйн чщешд бсйлеп оевбш мсшип отй ечйбд. йзг тн жаъ, боид-армйжд бд рбгч дчщш ойреп-ъвебд роца лй лм цшйлд щм 90 вшн/йен чщешд бсйлеп роек б-6% мсшип баефп лммй. дзечшйн оцййрйн лй бшеб дозчшйн ма дййъд дфшгд бйп цшйлъ гврйн омеищйн ложеп (лвеп аешж ае зйид) ебйп цшйлъ ожереъ добессйн тм гврйн омеищйн (лвеп тевеъ етевйеъ), ръеп дочщд тм фйшещ дооцайн.
дзечшйн ослойн лй чййоеъ тгейеъ тчбйеъ млк щцшйлъ гврйн омайн чщешд бсйлеп оефзъ мсшип, ащш ъеолеъ бдомцеъ дъжеръйеъ дотеггеъ цшйлъ гврйн омайн. мцг жд, дооцайн бдъййзс мчщш бйп цшйлъ гврйн омеищйн едсйлеп мсшип айрн тчбййн.
https://pubmed.ncbi.nlm.nih.gov/33297391/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ъцфйъййн, (2021) детшк дчщш бйп цшйлъ фишйеъ бъжерд ебйп дсйлеп мдъфъзеъ сшип олм сев. бсчйшд рлмме 17 озчшйн, одн щйщд озчшй течбд е-11 озчшй очшд-бчшд.
баефп лммй роца лй цшйлд вбедд йеъш щм фишйеъ дййъд чщешд бсйлеп роек йеъш мдъфъзеъ сшип, лк щбдщееад мощъъфйн тн дцшйлд дроелд бйеъш дощъъфйн тн дцшйлд двбедд бйеъш дйе бсйлеп роек б-34% мсшип олм сев. бдъййзс мсевй дсшип, роца чщш оебдч шч бдъййзс мсшип щг (сйлеп роек б-35%), лащш севй сшип азшйн рбгче шч босфш оети щм озчшйн. тег ошайн дзечшйн лй дчщш бйп цшйлъ фишйеъ едсйлеп мсшип дйд ъмей ойреп, лк щтбеш цшйлд вбедд щм 18 вшн/йен дсйлеп дйд роек б-45% бдщееад мдтгш цшйлд.
дзечшйн осбйшйн лй ддщфтд дойийбд щм фишйеъ ребтъ бтйчш офтймеъп ревгъ дзоцеп, бтйчш щм дшлйб дфтйм ergothioneine, елп ошлйбйн ресфйн лое биа-вмечп мдн фтймеъ ревгъ вйгемйн еоеесъъ зйсерйъ.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм дфеирцйам щм фишйеъ бъжерд мдврд офрй дъфъзеъ сшип, ебтйчш сшип дщг.
https://pubmed.ncbi.nlm.nih.gov/33724299/
бсчйшд (2023) оецвеъ дтгейеъ мвбй ддшлб длйой, дтшк дъжеръй едфеирцйам дбшйаеъй щм щоп щеощен. босвшъ дсчйшд дзечшйн офшийн аъ дйчу дййцеш двмебмй щм щеощен ещоп щеощен. бдощк, дн оцйвйн аъ дфшефйм длйой едъжеръй щм щоп щеощен, грйн бдшлб щме бйзс мщорйн цозййн азшйн, еоцйвйн аъ дфеирцйам ревг дзоцеп щме. бзмчд дазшеп щм дсчйшд оецвйн ооцайн бдъййзс мдщфтеъ бшйаеъйеъ ойийбеъ щм щоп щеощен, лемм дщфтд тм шоъ LDL, айжеп вмйчой, бшйаеъ чшгйеесчемшйъ, сшип, жйлшеп еамцдййош, ъдмйлй гмчъ, дврд одщощ едщфтеъ азшеъ.
дзечшйн оцййрйн осфш сйлерйн дчщешйн бцшйлъ щеощен, лвеп ълемд чмешйъ вбедд ащш тмемд мдебйм мтмййд бощчм ештмрйн щерйн ащш тмемйн мтбеш мщоп. дзечшйн ослойн лй мщоп щеощен феирцйам мдщфтд зйебйъ тм бшйаеъ дагн бжлеъ дшлбе дъжеръй дтщйш ефтймеъе ревгъ дзоцеп. дцшйлд щм щоп щеощен, щдйре тщйш бзеоцеъ щеоп бмъй шеейеъ, тщейд мъшен меейсеъ ъдмйлйн зйсерййн егмчъййн бвеу елъецад олк морет озмеъ чшгйеесчемшйеъ еоибемйеъ.
https://pubmed.ncbi.nlm.nih.gov/37377483/
бсчйшд (2021) грйн дзечшйн боафййрйн ебдщмлеъ дбшйаеъйеъ щм ооъйчйн омалеъййн. босвшъ дсчйшд оецвйн овееп дооъйчйн домалеъййн, лемм зойщд ооъйчйн щаещше мщйоещ тм йгй д-FDA: слшйп, селшмеж, асфшин, рйеиан ецйчмои. бдъййзс млм ооъйч, оецвйн дооцайн оозчшйн фшд-чмйрййн ечмйрййн мвбй ддщфтеъ дбшйаеъйеъ щме.
дзечшйн ошайн лй мошеъ дщйоещ дщлйз бооъйчйн амд, дтгейеъ дозчшйеъ оцбйтеъ тм овееп дщфтеъ щмймйеъ, дзм олабй шащ чмйн етг сйлеп оевбш мсшип. озчшйн щерйн ошайн лй дщйоещ бооъйчйн омалеъййн чщеш бървегъ майрсемйп едъфъзеъ селшъ сев 2, дщйоещ басфшин рчщш ббтйеъ чеврйийбйеъ едърдвеъйеъ, еозчшйн азшйн дшае лй дщйоещ бооъйчйн омалеъййн тмем мдебйм мзесш айжеп баелмесййъ зййгчй дотй емдъфъзеъ лбг щеорй.
мфйлк, дзечшйн оомйцйн мдвбйм аъ дцшйлд млоейеъ чиреъ ема мцшек аеън мъчефеъ ооещлеъ отм мшоъ дцшйлд дйеойъ доеъшъ (ADI). дн чешайн мдощйк емдтшйк аъ бийзеъ дщйоещ бооъйчйн амд биеез дашек, елп аъ ддщфтд доибемйъ едбшйаеъйъ щмдн.
http://www.biotech-asia.org/vol18no2/artificial-sweeteners-and-their-health-implications-a-review/
бсчйшд (2020) детшле дтгейеъ бдъййзс мщйоещ бъецшй дгбешд мийфем бозмъ дсшип еморйтъд. босвшъ дсчйшд расфе домцеъ о-129 сфшйн барвмйъ, цшфъйъ ае вшорйъ, щрмчзе ооавшй ръерйн лвеп EBSCO, ак вн сфшйн офмифешоеъ щм шбй олш, мма сйреп щм айлеъ дсфшйн, бдъййзс мщйоещ дийфемй бъецшй дгбешд (Apitherapy) бдчщш мозмъ дсшип. лое лп, ртшлд дщееад бйп домцеъ амд мтгейеъ щрасфе бозчшйн чмйрййн.
мдмп дооцайн дтйчшййн щм дсчйшд:
-
б-18 сфшйн роцад домцд мщйоещ бъецшй дгбешд морйтъ сшип, б-39 сфшйн роцад домцд мщйоещ бъецшй дгбешд лийфем ощмйн бозмъ дсшип, еб-17 сфшйн роцад дъййзсеъ млк щдщйоещ бъецшй дгбешд тщей мъшен мдзмод осшип.
-
бдъййзс морйтъ сшип – обйп 18 дсфшйн, б-6 сфшйн рлммд дъййзсеъ мщйоещ бфемп еб-3 сфшйн мщйоещ бгбщ, аемн бау азг одсфшйн ма рлмм ойгт мвбй ойгъ дйтймеъ.
-
бдъййзс мийфем ощмйн бсшип – обйп 39 дсфшйн, ддомцеъ лмме щйоещ бфемп (6 сфшйн) ебфшефемйс (3 сфшйн), бтйчш мтйшеш дотшлъ дзйсерйъ е/ае мщйфеш доцб дъжеръй бчшб земй сшип.
-
бдъййзс мдзмод осшип – ддомцеъ щроцае бсфшйн дйе мшеб овеереъ ема сфцйфйеъ, елмме щймеб щм овееп шлйбйн.
-
шч бсфшйн отийн рлмм ойгт сфцйфй, ебау азг одсфшйн ма рлмм ойгт осфйч, бдщееад мйгт щрасу босвшъ озчшйн чмйрййн. баефп сфцйфй, ддомцеъ бсфшйн ма лмме ойгт бдъййзс мдщфтд щм ъецшй дгбешд тм дйбийн щерйн щм дийфем бсшип, бгвщ тм ддщфтеъ дщмймйеъ щм лйоеъшфйд ешгйеъшфйд, лвеп оечежйийс бфд, фвйтд тешйъ, тййфеъ етег.
дзечшйн ослойн лй сфшйн дтесчйн бщйоещ дийфемй бъецшй дгбешд айрн одеейн очеш ойгт иеб бдъййзс мийфем бсшип еморйтъе. йзг тн жаъ, ддомцеъ щрасфе оцбйтеъ тм дфеирцйам щм ъецшй гбешд осейойн морйтъ сшип елийфем ощмйн, етщейеъ мдееъ бсйс мдощк дозчш бреща.
https://pubmed.ncbi.nlm.nih.gov/32507447/
бсчйшд (2019) оецвйн дооцайн дфшд-чмйрййн бревт мфтймеъ ревгъ дсшип щм дфмбереайг меиаемйп (Luteolin) еорврерй дфтймеъ дотешбйн.
https://www.ncbi.nlm.nih.gov/pubmed/30798142
бсчйшд (2019) оецвйн дорврерйн дотешбйн бфтймеъ ревгъ дсшип щм гбщ ешлйбйе дфтймйн дтйчшййн – фмбереайгйн (чоффшем, чилйрйн ечеешцийп) езеоцеъ фремйеъ (зеоцд чфайъ езеоцд вамйъ).
https://pubmed.ncbi.nlm.nih.gov/30639116/
бсчйшд (2019) грйн дзечшйн бщйоещ бацеъ лбсйс мфйъез ожереъ еощчаеъ ферчцйермййн, ъек дъочгеъ бдщфтд ревгъ сшип. дзечшйн оцййрйн лй ацеъ дйрп очеш обийз мфйъез щм ожереъ ферчцйермййн, бщм дтещш бтшлйн ъжеръййн - змберйн езеоцеъ аойре, ейиойрйн, фйворийн (лмешефйм, чшеиреайгйн е- фйчебймйфшеиайрйн), зеоцеъ щеоп, фйиесишеЙмйн, фемйслшйгйн ефемйфреЙмйн.
https://www.ncbi.nlm.nih.gov/pubmed/31146462
бсчйшд (2018) офешиеъ дтгейеъ дтглрйеъ бдъййзс мфтймеъ ревгъ дсшип еморврерй дфтемд дотешбйн щм овееп фмбереайгйн - бйрйдн афйврйп, меиаемйп, чеешцийп, дсфшйийп, EGCG, цйарйгйп, врйсиайп егайгжайп.
https://www.ncbi.nlm.nih.gov/pubmed/30424557
бозчш течбд фшесфчийбй (2020) щртшк бцшфъ рбгч дчщш бйп цшйлъ дселш бъжерд мбйп дсйлеп мдъфъзеъ сшип. дзечшйн осбйшйн лй лйен йгет щцшйлъ селш тегфъ одеед вешн сйлеп ошлжй мщореъ, селшъ сев 2 емъзмеад чшгйеесчемшйъ, аемн дтгейеъ мвбй дчщш бйп цшйлъ селш едъфъзеъ сшип айрп тчбйеъ. озчшйн фшд-чмйрййн оцбйтйн тм лк щддщфтд щм селш тм дъфъзеъ сшип дйрд лъецад ощореъ, лащш орврерйн ресфйн тщеййн мдйеъ отешбйн, лвеп ъдмйлй гмчъ, тчд зоцерйъ еървегъ майрсемйп, вн бдтгш тмййд бощчм.
бозчш рлмме дръерйн щм 101,279 ощъъфйн отм вйм 18 (42 бооецт), лащш ощк дотчб дзцйерй дйд л-6 щрйн. цшйлъ дселш дооецтъ дййъд 92.8 вшн мйен, л-20% оск дцшйлд дчмешйъ, лащш дощъъфйн тн дцшйлд дроелд бйеъш (шбтеп ъзъеп) цшле 55.57 вшн/йен едощъъфйн тн дцшйлд двбедд бйеъш (шбтеп тмйеп) цшле 135.31 вшн/йен. цшйлъ дселш доесу бшбтеп дъзъеп едтмйеп дййъд 19.48 е-62.23 вшн/йен, бдъаод.
роца лй дсйлеп мдъфъзеъ сшип баефп лммй дйд вбед б-17% бчшб дощъъфйн тн цшйлъ дселш двбедд бйеъш бдщееад мроелд бйеъш, едсйлеп мсшип щг дйд вбед б-51%.
ъецаеъ амд дйе оебдчеъ сиийсийъ вн мазш дъаод мтмййд бощчм бодмк ъчефъ дотчб. лое лп, роца лй цшйлд вбедд щм селш оесу, селшйн зефщййн (селш оесу еселш ибтй доцей бойцй фйшеъ, гбщ есйшефйн), селшеж, селшйн щочешн ботгрй змб, оецшй змб еощчаеъ ооеъчйн, дййъд чщешд бсйлеп оевбш мдъфъзеъ сшип.
дзечшйн ослойн лй ооцай дозчш оцбйтйн тм лк щцшйлъ селш бъжерд одеед вешн сйлеп дфйк морйтъ сшип, ебтйчш сшип щг, еблк осфчйн ъойлд мгйеп брещай огйрйеъ дчщешд бселш (лвеп ойсей ешвемцйд щйеечйъ).
https://pubmed.ncbi.nlm.nih.gov/32936868/
бозчш течбд фшесфчийбй, (2019) щртшк бцшфъ, рбгч дчщш бйп цшйлъ ощчаеъ оъечйн – ооеъчйн бселш, ойцй фйшеъ 100% еощчаеъ тн ооъйчйн омалеъййн - мбйп дсйлеп мсшип. бозчш рлмме 101,257 ощъъфйн отм вйм 18 (42 бооецт). цшйлъ ощчаеъ оъечйн детшлд баоцтеъ йеорй алймд зежшйн, тн 2-15 гйеезйн тбеш лм ощъъу. бодмк ъчефъ отчб ооецтъ щм л-5 щрйн, аебзре 2,193 очшйн щм сшип, одн 693 очшйн щм сшип щг, 291 очшйн щм сшип тшоерйъ е-166 очшйн щм сшип чемешчимй. дцшйлд дйеойъ дзцйерйъ щм ощчаеъ оъечйн дййъд 90.3 о"м мвбшйн е-74.6 о"м мрщйн, бзмечд щм 45% ойцй фйшеъ, 36% ощчаеъ ооеъчйн бселш е-19% ощчаеъ тн ооъйчйн омалеъййн.
баефп лммй, роца лй цшйлъ ощчаеъ оъечйн дййъд чщешд бсйлеп оевбш мсшип олм сев (тмййд щм 18% бсйлеп тбеш тмййд щм 100 о"м/йен) емсшип дщг (тмййд щм 22% тбеш тмййд щм 100 о"м/йен). цшйлъ ощчаеъ тн ооъйчйн омалеъййн ма дййъд чщешд бсйлеп оевбш мсшип еайме цшйлд щм ойцй фйшеъ дййъд чщешд бсйлеп вбед б-12%.
ооцайн амд оцбйтйн тм лк щцшйлъ ощчаеъ оъечйн, лемм ойцй фйшеъ, одеед вешн сйлеп мсшип дрйъп мщйрей.
https://www.ncbi.nlm.nih.gov/pubmed/31292122
лзмч оозчш течбд (2018) айшефай вгем (EPIC), бозчш дрелзй рбгч дчщш бйп айлеъ дъжерд мбйп дсйлеп мсшип. бшчт мозчш осбйшйн дзечшйн лй азг ддйбийн дошлжййн борйтъ ъзмеад лшерйъ дйре длееръ дцйбеш мбзйшъ ожереъ айлеъййн ебшйайн йеъш, лащш богйреъ шбеъ ртшк ъдмйк диотд щм сйоеп ожереъ бдъан мтшлн дъжеръй. бозчш рлмме дръерйн щм 471,495 ощъъфйн, лащш бъчефъ отчб щм л-15 щрд аебзре 49,794 очшй сшип (одн 12,063 очшйн щм сшип щг, 6,745 очшйн щм сшип тшоерйъ е-5,806 очшйн щм сшип чемешчимй). дцшйлд дъжеръйъ детшлд баоцтеъ щамерй ъжерд, доеъаойн млм огйрд, едайлеъ щм лм фшйи ожеп ае ощчд детшлд бдъан мълемъ дчмешйеъ, селш, щеоп шеей, ръшп, сйбйн, змбеп ейшчеъ/фйшеъ/чирйеъ/авежйн м-100 вшн. дзечшйн зйщбе млм ощъъу цйеп лемм, добиа аъ айлеъ дъжерд дооецтъ щме, лащш цйеп вбед йеъш обиа айлеъ ъжерд роелд йеъш.
роца лй ощъъфйн тн айлеъ дъжерд дроелд бйеъш дйе бсйлеп вбед б-7% мсшип бдщееад мощъъфйн тн айлеъ дъжерд двбедд бйеъш, лащш дсйлеп дабсемеий дйд 81.4 мтеоъ 69.5 очшйн м-10,000 щреъ агн, бдъаод. баефп сфцйфй, роца сйлеп вбед йеъш мсшип чемешчимй, мсшип ботшлъ дтйлем дтмйерд едчйбд, мсшип шйаеъ бчшб вбшйн емсшип лбг есшип щг мазш вйм дотбш бчшб рщйн. дзечшйн ослойн лй ооцайн амд огвйщйн аъ дзщйбеъ щм сйеев айлеъ дожереъ тбеш сйоеп дожереъ етбеш оггйн ъжеръййн азшйн дчщешйн ббшйаеъ дцйбеш.
https://www.ncbi.nlm.nih.gov/pubmed/30226842
озчш очшд-бчшд ощеъу мзечшйн йщшамйн еаошйчайн (афшйм 2016) ащш ретг мбзеп аъ дчщш бйп щъййъ чфд мбйп дсйлеп мсшип чемешчимй.
лзмч оозчш вгем щртшк бйщшам, дозчш дрелзй обесс тм ръерйн щм 5,145 земй сшип чемешчимй ечбецъ дщееад щм 4,097 ощъъфйн бшйайн.
роца лй щъййъ чфд дййъд омеед бсйлеп оефзъ бл-26% мсшип чемешчимй. овод геод роцад вн тбеш щъййъ чфд рием чфайп ечфд щзеш обещм. баефп сфцйфй, бдщееад мощъъфйн дщеъйн фзеъ ооръ чфд мйен, щъййъ 1-2, 2-2.5 еотм 2.5 ореъ чфд мйен дййъд омеед бсйлеп оефзъ мсшип чемешчимй бл-22%, 41% е-54%, бдъаод.
дзечшйн ослойн лй ооцайн аме оцбйтйн лй чфд тщей мдвп тм дотй офрй дъфъзеъ ъдмйлйн сширййн.
дтшъ дотшлъ: дозчш оеоп тм йгй ашвеп дбшйаеъ даошйчай (NIH). зщеб мцййп лй дзсшеп щм озчш осев жд дйа щма рйъп мдсйч бегаеъ тм чщш щм сйбд еъецад.
http://cebp.aacrjournals.org/content/25/4/634.full.pdf+html
озчш (оай 2016) дбегч аъ дчщш бйп осфш гфесй ъжерд мбйп дсйлеп мсшип чемешчимй. дзечшйн оцййрйн лй ъжерд еаешз зййн одеейн вешой сйлеп бдъфъзеъ сшип чемешчимй аемн орвреп ддщфтд айре бшеш мвошй.
босвшъ дозчш щртшк бйшгп, дзечшйн асфе ръерйн мвбй гфес дъжерд щм 220 земй сшип чемешчимй ещм 281 ощъъфйн бшйайн бтмй оафййрйн сецйе-гоевшфййн геойн.
орйъез лмм дръерйн дзечшйн жйде щмещд гфесй ъжерд тйчшййн: "ъжерд бшйад" (доаефййръ бтйчш бцшйлъ фйшеъ ейшчеъ), "ъжерд тъйшъ селш еъд" (доаефййръ бтйчш бцшйлъ селш еъд) е"ъжерд отшбйъ" (доаефййръ бтйчш бцшйлъ бщш аген, гврйн, бйцйн егвйн).
роца лй гфес щм "ъжерд отшбйъ" дйд чщеш бсйлеп вбед бл-88% мдъфъзеъ сшип чемешчимй, лащш бщрй дгфесйн дазшйн жедд сйлеп оефзъ щайре оебдч сиийсийъ.
http://www.ncbi.nlm.nih.gov/pubmed/27206698
счйшд (сфиобш 2015) дослоъ аъ дтгейеъ дозчшйеъ дтглрйеъ мвбй дъшеод дбшйаеъйъ щм лесоъ (Fagopyrum esculentum) ъек дъочгеъ бъфчйг дшлйбйн дфтймйн еорврерй дфтймеъ щмдн.
длеъбйн офшийн щлесоъ дйрд цоз оалм гоей гвп, рием вмеип, ащш тщйш бшлйбйн ъжеръййн ероца лбтм ъшеод мдфзъъ шоеъ длемсишем, мдврд тм дфтймеъ дтцбйъ, моцбй йъш мзх гн ебтм дщфтд арий-сширйъ, арий-гмчъйъ еарий-селМшъДйъ елп бтм фтймеъ фшд-бйеийъ еревгъ зоцеп.
озчшйн фшд-чмйрййн оцбйтйн тм дъфчйг щм дшлйбйн дфтймйн, бйрйдн D-chiro-inositol, дзмберйн едфмбереайгйн шеийп ечеешцийп, бдщфтд дбшйаеъйъ щм лесоъ.
http://www.ncbi.nlm.nih.gov/pubmed/26270637
бсчйшд (2018) оецвйн дооцайн дфшд-чмйрййн бревт мшлйбйн ибтййн ащш отеггйн ъдмйлй фйшеч щм ъайн сширййн (аеиефвйд). босвшъ дсчйшд грйн дзечшйн бзщйбеъ щм ъдмйлй аеиефвйд бсшип, офшийн одн шлйбйн дцозййн ащш отлбйн ае отеггйн ъдмйлйн амд еосбйшйн аъ орврерй дфтемд доемчемшййн.
бйп дшлйбйн доежлшйн бсчйшд рлммйн ойцей аомд (Emblica officinalis), зеоцд мйфеайъ, бшбшйп, деречйем етег. бдощк, оецвйн бфйшеи щмещд шлйбйн цозййн, щроцае лотеггй ъдмйлй аеиефвйд еащш тщеййн мдвбйш ъоеъъ ъайн сширййн - лащш рйърйн бцешъ ъесу: лешлеойп, Polyalthia longifolia едшлйб дфтйм щме HCD доцей бвжт дтх, едшлйб дфтйм Prodigiosin (амчмеайг бтм фйвори аген, дойецш т"й зййгчйн). дзечшйн ослойн лй демлеъ еоцибшеъ дтгейеъ мвбй ддщфтд щм шлйбйн ибтййн босфш севй сшип, аемн ргшщйн озчшйн фшд-чмйрййн ечмйрййн ресфйн лбсйс мфйъез ийфемйн ревгй-сшип згщрййн. .
https://www.ncbi.nlm.nih.gov/pubmed/28671583
озчш отбгд (аечиебш 2015) доцбйт тм шоеъ вбедеъ одъчп дайшефай доеъш щм зеошйн дзщегйн лосширйн бзмч оъесфй дожеп дощеечйн байшефд. йщ мцййп лй огебш бъесфйн бътщййъ дожеп, ема бъесфй ъжерд дролшйн мцшлрйн ббъй ибт еббъй ошчзъ.
http://www.ncbi.nlm.nih.gov/pubmed/26467752
бозчш течбд (2018) бшйий обесс аелмесййд рбгч дчщш бйп щъййъ чфд мъоеъд, еаъ ддщфтд щм оафййрйн вриййн дчщешйн боибемйжн щм чфайп тм чщш жд. дозчш обесс тм оавш ръерйн щм л-9 оймйеп айщ, длемм ръерйн гоевшфййн, дшвмй аешз зййн еойгт врий, лащш бозчш дрелзй рлмме дръерйн щм л-500,000 ощъъфйн. тм бсйс дбгмйн вриййн осейойн, млм ощъъу зещб цйеп врий щм оибемйжн щм чфайп ербгч дчщш бйп щъййъ чфд мбйп ъоеъд бъчефъ отчб щм 10 щрйн.
вйм дощъъфйн дооецт дйд 57 е-78% одн цшле чфд (лемм щзеш, рос ерием чфайп). бодмк ъчефъ дотчб 14,225 одощъъфйн рфише. орйъез дръерйн темд лй баефп лммй цшйлъ чфд чщешд бсйлеп роек йеъш мъоеъд. бдщееад мощъъфйн щма щъе чфд лмм, щъййд щм тг 1, 1, 2-3, 4-5, 6-7, еотм 8 лесеъ мйен дййъд чщешд бсйлеп роек б-6%, 8%, 12%, 12%, 16% е-14% мъоеъд. овод геод роцад тбеш чфд щзеш, рос ае рием чфайп етбеш вешой дъоеъд дщлйзйн, лвеп озмеъ чшгйеесчемшйеъ есшип. ма роцад дщфтд ощотеъйъ мцйеп дврий щм оибемйжн щм чфайп, дотйг тм оибемйжн айий йеъш ае одйш йеъш, тм чщшйн амд. дзечшйн ослойн лй ооцайн амд оцбйтйн тм ъфчйг щм шлйбйн азшйн, омбг чфайп, бчщш бйп цшйлъ чфд мбйп сйлеп оефзъ мъоеъд.
дозчш оеоп т"й дбйе-брч дбшйий ебщйъеу д-NIH
https://www.ncbi.nlm.nih.gov/pubmed/29971434
бсчйшд щйиъйъ еоид-армйжд (оай 2017) рбгч дчщш бйп цшйлъ чфд, лемм чфд рием чфайп, мбйп дсйлеп мсшип длбг.
бсчйшд рлмме 18 озчшй течбд, бдн отм 2 оймйеп ощъъфйн е-2,905 очшйн щм сшип лбг, елп 8 озчшй очшд-бчшд бдн 1,825 земйн е-4,652 ощъъфйн бшйайн. брйъез лмм дръерйн роца лй двгмъ цшйлъ дчфд б-2 лесеъ мйен дййъд чщешд бсйлеп роек б-35% мсшип длбг, лащш дчщш дйд змщ йеъш тбеш озчшй течбд мтеоъ озчшй очшд-бчшд (йшйгд щм 29% бсйлеп мтеоъ 67%). чщш жд ма дйд ъмей бозмеъ лбг, бцшйлъ амледем, тегу ощчм, селшъ сев 2, тйщеп ае дфийийс B ае C. башбтд озчшйн, бдн рбгч дчщш тбеш чфд рием чфайп, роца лй двгмъ цшйлъ дчфд б-2 лесеъ мйен дййъд чщешд бсйлеп роек б-14% мсшип длбг.
овееп орврерй фтемд тщеййн мтоег ббсйс дчщш бйп чфд, ебойезг чфайп, мбйп сшип длбг, лемм дврд офрй дъфъзеъ щзоъ длбг, додеед вешн сйлеп ощотеъй мсшип длбг; дщфтд арий-чшцйреврйъ длеммъ орйтъ щвщев ъай сшип длбг, двбшъ фтймеъ аржйой длбг дощфшъ аъ доибемйжн едфшщъ шлйбйн чшцйреврйн ефтймеъ ревгъ зоцеп довйрд тм д-DNA; тйлеб фтймеъ рвйфйъ (дфийийс); еорйтъ селшъ сев 2.
дзечшйн чешайн мбйцет озчшйн ачшаййн обечшйн тн двгшд бшешд щм цшйлъ чфд тм оръ мъоек бооцайн амд емчбет одй дйтймеъ щм чфд мдврд офрй сшип длбг, бойезг бчшб чбецеъ бсйлеп вбед.
https://www.ncbi.nlm.nih.gov/pubmed/28490552
бозчш зък обесс аелмесййд (йерй 2017), щртшк бвшАорйд, рбгч дчщш бйп цшйлъ бщш мбйп дъфъзеъ фемйфйн ботй. бозчш рлмме 15,950 ощъъфйн отм вйм 55 щтбше бгйчъ чемересчефйд.
бчшб 3,340 одощъъфйн (20.4%) аебзп фемйф осев агреод бщмб шащерй (nonadvanced), бчшб 1,643 одощъъфйн (10%) аебзп фемйф осев агреод бщмб оъчгн (advanced) ебчшб 189 одощъъфйн (1.2%) аебзп сшип чемешчимй.
баефп лммй ма роца чщш бйп цшйлъ бщш аген ае отебг мбйп дсйлеп магреод олм сев. тн жаъ, роца лй цшйлъ бщш отебг дййъд чщешд бсйлеп вбед йеъш магреод бщмб оъчгн бфй дибтъ бмбг. ма роца чщш бйп цшйлъ теу мбйп фемйфйн ботй. дзечшйн огвйщйн лй йщ мащщ аъ дооца мвбй дчщш бйп бщш отебг едсйлеп мфемйфйн бфй дибтъ бозчшй течбд фшесфчийбййн.
https://www.ncbi.nlm.nih.gov/pubmed/28468894
щрй озчшйн, щфешсое мазшерд, тесчйн бчщш бйп цшйлъ чфд ещйтешй дъоеъд бдъййзс маелмесйеъ щереъ.
бозчш дшащеп рбгч дчщш бйп цшйлъ чфд мбйп дсйлеп мъоеъд оечгоъ лзмч оозчш течбд айшефай вгем дтесч бсшип ебъжерд. бозчш дрелзй рлмме дръерйн щм отм м-500,000 ощъъфйн о-10 огйреъ байшефд. бъчефъ отчб щм л-16 щрйн, 41,693 одощъъфйн рфише. бдщееад мощъъфйн щма цшле лмм чфд, роца лй дощъъфйн тн цшйлъ дчфд двбедд бйеъш (отм 3 лесеъ мйен) дйе бтмй сйлеп роек йеъш мъоеъд (роек б-12% тбеш вбшйн еб-7% тбеш рщйн). ма роцае дбгмйн ощотеъййн бйп огйреъ щереъ. тег роца лй цшйлъ чфд вбедд дййъд чщешд бсйлеп роек йеъш баефп ощотеъй мъоеъд лъецад оозмеъ бгшлй дтйлем (роек б-60% тбеш вбшйн еб-40% тбеш рщйн). лое лп, бчшб рщйн, цшйлд вбедд щм чфд дййъд чщешд бсйлеп роек б-22% мъоеъд лъецад оозмеъ есчемшйеъ, бсйлеп роек б-30% мъоеъд лъецад оайшет оезй ебсйлеп вбед б-30% мъоеъд осшип дщзмеъ. бъъ-огвн длемм л-15,000 ощъъфйн роца лй цшйлд вбедд щм чфд дййъд чщешд бшод роелд йеъш щм аржйой длбг ебчшб рщйн бмбг бшод роелд йеъш щм догг дгмчъй CRP ещм доевмебйп оселшш. ооцайн амд оцбйтйн тм лк щмцшйлъ чфд тщейд мдйеъ дщфтд овйрд офрй ъоеъд оечгоъ, бойезг лъецад оозмеъ бгшлй дтйлем еблмй дгн.
бозчш ресу рбгч дчщш бйп цшйлъ чфд едсйлеп мъоеъд оечгоъ бчшб аелмесййд овееръ обзйрд аърйъ. лзмч оозчш течбд, щдзм бйп дщрйн 1993-1996 бмес арв'мс едееай, бозчш дрелзй рлмме л-185,000 ощъъфйн ооеца афше-аошйчай, ймйгй дееай, аошйчайн ооеца йфрй емийрй еаошйчайн мбрйн. бъчефъ отчб щм л-16 щрд, 58,397 одощъъфйн рфише. роца лй бдщееад мощъъфйн щма цшле чфд, цшйлъ чфд дййъд чщешд бсйлеп роек йеъш мъоеъд тн сйлеп роек б-12% тбеш лес чфд 1 мйен, 18% тбеш 2-3 лесеъ мйен е-18% тбеш отм 4 лесеъ мйен. бдъййзс мщййлеъ аърйъ, дооцайн блм дчбецеъ дйе оебдчйн сиийсийъ омбг бчбецд щм ймйгй дееай. овод геод роцад баефп сфцйфй вн бчшб ощъъфйн щотемн ма тйщре, ощъъфйн оъзъ мвйм 55 еощъъфйн мма озмеъ лшерйеъ. дсйлеп мъзмеад роца роек йеъш бдъййзс мозмеъ мб, сшип, озмеъ рщйод, щбх, селшъ еозмъ лмйеъ.
щрй дозчшйн, щоеоре тм йгй вефйн бшйаеъййн оощмъййн, оцбйтйн тм лк щцшйлъ чфд вбедд йеъш чщешд бсйлеп роек йеъш мъоеъд оечгоъ лъецад оосфш вгем щм озмеъ, баефп бмъй ъмей бщййлеъ аърйъ ае вйаевшфйъ емма ъмеъ бтйщеп ае бсев дчфд (олйм чфайп ае рием). дзечшйн осбйшйн лй дчфд олйм дшбд шлйбйн фтймйн, лемм чфайп еъшлебеъ фремйеъ, ащш тщеййн мдщфйт тм дбшйаеъ баоцтеъ орврерйн щерйн, лвеп дфзъъ тчд зоцерйъ, фтймеъ ревгъ сшип, двбшъ дшвйщеъ майрсемйп, щйфеш ъфчег ъай длбг, дфзъъ дцибшеъ щеоп блбг едфзъъ гмчъ лшерйъ. дщфтеъ аме рцфе бозчшйн щбецте бзйеъ отбгд. оазш едчщшйн рцфе вн тбеш дчфд щолйм чфайп евн тбеш дчфд щма олйм чфайп, дзечшйн ощтшйн лй рйъп мййзс аъ ддщфтд мшлйбйн азшйн доцеййн бчфд ема шч мчфайп тцое. лое лп, бдйръп щдчщш мдфзъъ дсйлеп мъзмеад чшгйеесчемшйъ роца бтйчш бдъййзс мрщйн, дзечшйн иетрйн лй ййълп емчфд дщфтд ъмеййъ-ойп тм дфшефйм доибемй едгмчъй. тн жаъ, дзечшйн оцййрйн лй айп дщтшд огет цшйлъ чфд чщешд бсйлеп оевбш мсшип дщзмеъ.
https://www.ncbi.nlm.nih.gov/pubmed/28693038
https://www.ncbi.nlm.nih.gov/pubmed/28693036
бозчш течбд фшесфчийбй обесс аелмесййд (оай 2017), щртшк бйфп, рбгч дчщш бйп гфес дъжерд мбйп дсйлеп мсшип чемешчимй.
бозчш рлмме л-93,000 ощъъфйн, азшйдн бецт отчб дзм одщрйн 1995-1998 етг мщръ 2012. бъчефъ дотчб 2,482 одощъъфйн аебзре тн сшип чемешчимй. тм бсйс щамерй ъжерд, щоемае бъзймъ ъчефъ дотчб, дзечшйн жйде щмещд гфесй ъжерд тйчшййн: гфес щм ъжерд бшйад йзсйъ ("ъжерд щчемд"), ъжерд отшбйъ еъжерд осешъйъ. ъжерд щчемд аефййрд бцшйлд вбедд щм йшчеъ, фйшеъ, аишйеъ, ъфезй агод, оецшй сейд, фишйеъ еацеъ. ъжерд отшбйъ аефййрд бцшйлд вбедд щм бщш аген, бщш отебг, оецшй змб, ойцй фйшеъ, ощчаеъ чмйн, чфд, ъд, шибйн еамледем. ъжерд осешъйъ аефййрд бцшйлд вбедд щм зоецйн, гвйн ефйшеъ йн, теу есачд.
бдщееад бйп дощъъфйн тн дцйерйн двбедйн бйеъш мроелйн бйеъш роца лй гфес щм ъжерд щчемд дйд чщеш бсйлеп роек б-15% мсшип чемешчимй бчшб вбшйн, тн чщш зжч йеъш тбеш сшип ботй дгйсимй, ак бсйлеп вбед йеъш мсшип шчимй бчшб рщйн. гфес щм ъжерд отшбйъ дйд чщеш бсйлеп вбед йеъш мсшип ботй еботй дгйсимй бчшб рщйн. ма роца чщш бйп гфес щм ъжерд осешъйъ мбйп дсйлеп мсшип чемешчимй. дзечшйн ощтшйн лй чщш жд дйре ъецад щм цшйлд вбедд йеъш щм бщш аген еотебг. ооцайн амд оцбйтйн тм дзщйбеъ щм гфес еайлеъ дъжерд ласишивйд морйтъ сшип чемешчимй.
https://www.ncbi.nlm.nih.gov/pubmed/28526274
бгез тглрй (2017), щфешсн бощеъу тм йгй дчшп дтемойъ мзчш дсшип (AICR) едолеп даошйчай мзчш дсшип (WCRF), ослойн цееъ дзечшйн аъ дтгейеъ дозчшйеъ бревт мчщш бйп ъжерд ефтймеъ вефрйъ мбйп сшип чемешчимй.
гез жд, додеед тглеп мгез щфешсн бщръ 2007, лемм 99 озчшйн (щртшле блм дтемн) - бдн л-29 оймйеп ощъъфйн ел-250,000 очшйн щм сшип чемешчимй. тм сок дооцайн щрасфе, дзечшйн ослойн лй чййоеъ тгейеъ обессеъ млк щцшйлъ гврйн омайн (лщмещ ореъ мйен), сйбйн ъжеръййн, оецшй змб (л-500 вш'/йен), риймъ ъесфй сйгп ебйцет фтймеъ вефрйъ ъешойн мдфзъъ дсйлеп мсшип чемешчимй, бтег щцшйлъ бщш аген ебщш отебг, цшйлд щм йеъш ощрй ощчаеъ амледемййн мйен, тегу ощчм, щореъ ечеод вбедд одеейн вешой сйлеп мдъфъзеъ сшип чемешчимй. бресу, дзечшйн ослойн лй чййоеъ тгейеъ осейоеъ мвешой сйлеп ресфйн, ащш чщешйн бсйлеп роек йеъш - лемм цшйлъ ожереъ тщйшйн бейиойп C, цшйлъ гвйн, ейиойп D ериймъ оемий-ейиойрйн, лащш цшйлд роелд (фзеъ о-100 вшн мйен) щм фйшеъ ейшчеъ ма тоймрййн ецшйлъ ожереъ долймйн бшжм осев дн (щочеше бзй) чщешд бсйлеп вбед йеъш мсшип чемешчимй.
ма роцае тгейеъ зг-ощотйеъ бдъййзс мвешойн ъжеръййн ресфйн лвеп гврйн, ъфезй агод, щеоп одзй, теу, фйшеъ йн, дшлб зеоцеъ дщеоп, лемсишем, аеовд 3 щочешд бгвйн, чирйеъ, щен, селш оесу, чфд, ъд, фзойоеъ, тоймрйн, теос вмйчой, зеоцд фемйъ, ейиойп A, ейиойп B6, ейиойп E, смрйен, оъйерйп, биа-чшеип, мйчефп, ск дцшйлд дчмешйъ, ъгйшеъ дашезеъ ае гфес дъжерд.
мдтшлъ дзечшйн л-47% оочшй дсшип дчемешчимй рйърйн морйтд баоцтеъ дчфгд тм ъжерд бшйад, бйцет фтймеъ вефрйъ ещойшд тм ощчм ъчйп.
http://www.aicr.org/continuous-update-project/colorectal-cancer.html
бозчш очшд-бчшд вгем обесс аелмесййд (йемй 2017), длемм 631 рщйн тн сшип дшзн ечбецъ бйчешъ щм 879 рщйн бшйаеъ, роца лй зщйфд вбедд йеъш мчгойен (щрбгчд баоцтеъ бгйчъ щъп) дййъд чщешд бсйлеп вбед б-22% мсшип дшзн, ллм дршад бщм фтймеъ дгеод масишевп. дочешеъ дтйчшййн мчгойен леммйн цшйлъ айбшйн фрйоййн ефйшеъ йн, елп тйщеп.
https://www.ncbi.nlm.nih.gov/pubmed/28742092
бозчш отбгд (аечиебш 2017) фешх гшк, щртшк тм оегм щм щошйн, ошайн дзечшйн оде дорвреп дазшай млк щцшйлъ селш вбедд овбйшд цойзъ вйгемйн сширййн (ъефтъ ешбешв), жаъ баоцтеъ ддщфтд щм селш осев Fructose 1,6-bisphosphate тм змберйн оощфзъ Ras, дотеггйн змечъ ъайн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/29030545
бозчш очшд-бчшд (ребобш 2017), щртшк ббйъ земйн байшап, рбгч дчщш бйп цшйлъ ъд ечфд мбйп дсйлеп мдъфъзеъ вмйеод (вйгем сширй ботшлъ дтцбйн дошлжйъ). бозчш рлмме 128 оиефмйн тн вмйеод ечбецъ бйчешъ щм 256 ощъъфйн - дгеойн боафййрй двйм едойп.
роца лй ощъъфйн тн цшйлъ дъд двбедд бйеъш, мтеоъ дроелд бйеъш, дйе бсйлеп роек бл-67% мвмйеод - вн мазш ришем вешойн ъжеръййн, лемм дцшйлд дчмешйъ едцшйлд щм шлйбй ожеп сфцйфййн лвеп бщш аген еотебг, чирйеъ еавежйн, фйшеъ еомз елп мазш дъаод сиийсийъ м-BMI. тег роца йзс дфек бйп чфд мбйп дсйлеп мвмйеод, лк щощъъфйн тн цшйлъ дчфд двбедд бйеъш дйе бсйлеп роек б-91% мвмйеод бдщееад мощъъфйн тн дцшйлд дроелд бйеъш. брйъез дощмб аъ цшйлъ дъд едчфд щм дощъъфйн, роца лй ощъъфйн тн дцшйлд двбедд бйеъш дйе бсйлеп роек б-65% мвмйеод бдщееад мощъъфйн тн дцшйлд дроелд бйеъш, мазш дъаод сиийсийъ мовееп ощърйн оътшбйн.
https://www.ncbi.nlm.nih.gov/pubmed/29124385
бозчш ачшай обечш ((2017) рбгчд ддщфтд щм гйаид гмъ-щеоп тм дсйлеп мсшип дмбмб. озчш жд дйре змч оозчш дътшбеъй вгем, щртшк башд"б етесч ббшйаеъ дайщд, бе рлмме л-49,000 рщйн мазш вйм дотбш бвймай 50-79. дощъъфеъ земче ачшайъ мчбецъ дгйаид (щретгд мдфзйъ аъ цшйлъ дщеоп емдвбйш аъ дцшйлд щм фйшеъ, йшчеъ егврйн) ае мчбецъ дбйчешъ (мма дътшбеъ) мъчефд щм 7-12 щрйн.
бозчш дрелзй рлмме дръерйн щм 46,200 ощъъфеъ, лащш бъчефъ отчб щм 9 щрйн осйен ддътшбеъ аебзре 92 очшйн щм сшип мбмб бчбецъ дгйаид е-165 очшйн бчбецъ дбйчешъ. ддбгм бйп дчбецеъ, добиа сйлеп роек б-14% ма дйд оебдч сиийсийъ. тн жаъ брйъез мфй ъъй-чбецеъ, роца лй бдщееад мчбецъ дбйчешъ, гйаид гмъ щеоп ъшод мдфзъъ дсйлеп мсшип дмбмб шч тбеш рщйн щдйе бтмеъ тегу ощчм бъзймъ дозчш (BMI отм 25), ак ма мрщйн щдйе бощчм ъчйп. озчш жд оцбйт тм ъшеод афщшйъ щм гйаид гмъ-щеоп мдфзъъ дсйлеп мсшип дмбмб бчшб рщйн мазш вйм дотбш дсебмеъ отегу ощчм.
https://www.ncbi.nlm.nih.gov/pubmed/28922784
бозчш течбд (ребобш 2017) рбгч дчщш бйп цшйлъ чфд мбйп дсйлеп мсшип шйаеъ, лзмч оозчш бшйаеъ дцйбеш щртшк бйфп. озчшйн афйгойемевййн чегойн оцае чщш зйебй бйп цшйлъ чфд есйлеп мсшип шйаеъ, аемн дзечшйн оцййрйн лй ййълп емтйщеп дййъд дщфтд тм дооцайн.
бозчш дрелзй рлмме л-87,000 ощъъфйн бвймай 40-69, лащш бодмк ъчефъ отчб ооецтъ щм л-17 щрд 1,668 одощъъфйн аебзре тн сшип шйаеъ. дзечшйн ошайн лй мошеъ щроца чщш зйебй бйп цшйлъ чфд мбйп дсйлеп мсшип шйаеъ, ощъъфйн тн цшйлъ чфд вбедд рие вн мтщп, лк щчщш жд ма дйд оебдч мазш щбецтд дъаод сиийсийъ мтйщеп. тн жаъ, роца чщш бйп цшйлъ чфд мбйп сйлеп оевбш мсшип шйаеъ осев SCC (дйгет вн л: small cell carcinoma), тн сйлеп вбед фй 3.5 тбеш ощъъфйн щцшле отм 5 лесеъ чфд мйен бдщееад мощъъфйн щма цшле чфд лмм.
дзечшйн ослойн лй баефп лммй ма роца чщш оебдч бйп цшйлъ чфд мбйп дсйлеп мсшип шйаеъ, омбг сйлеп вбед йеъш мсшип шйаеъ осев SCC.
https://www.ncbi.nlm.nih.gov/pubmed/29151475
бозчш течбд фшесфчийбй (ребобш 2017) рбгч дчщш бйп цшйлъ змб мазш абзеп щм сшип дтшоерйъ, мбйп дсйлеп мдйщреъ дозмд. дзечшйн осбйшйн лй чййоеъ тгейеъ млк щцшйлъ оецшй змб тъйшй щеоп, ебойезг змб ома, тмемд мдвбйш аъ дсйлеп мсшип тшоерйъ авшсйбй, аемн ма йгетд одй ддщфтд щм цшйлъ оецшй змб мазш абзеп дозмд.
бозчш рлмме 1,334 вбшйн тн сшип тшоерйъ щайре вшешъй, ащш оймае щамеп ъжерд лщръййн мазш абзеп дозмд. бодмк ъчефъ отчб ооецтъ щм 8 щрйн аебзре 137 очшйн щм дйщреъ дозмд. роца лй вбшйн щцшле отм 4 ореъ мщбет змб ома, бдщееад мвбшйн щцшле 0-3 ореъ мзегщ, дйе бсйлеп вбед б-73% мдйщреъ дозмд. тн жаъ, чщш жд дйд оебдч шч тбеш вбшйн тн BMI вбед, лк щтбеш аеъд шоъ цшйлд вбшйн тн BMI отм 27 дйе бсйлеп вбед фй 3 мдйщреъ. цшйлъ змб гм щеоп ае оецшй змб азшйн ма дййъд чщешд бсйлеп мдйщреъ сшип дтшоерйъ.
https://www.ncbi.nlm.nih.gov/pubmed/29105845
бозчш ъцфйъй шишесфчийбй (2020) рбгч дчщш бйп лоеъ дзмбеп бъжерд мбйп зежч щшйш дйг еощк ддйщшгеъ бчшб чщйщйн земй сшип оъчгн ботшлъ дтйлем. дзечшйн осбйшйн лй ъжерд тъйшъ змбеп отеггъ щйфеш босъ двеу дшжд бчшб чщйщйн мма сшип, аемн ма йгет дан йщ млк дщфтд ойийбд вн бчшб земй сшип.
бозчш рлмме 91 оиефмйн, ащш тебшйн ийфемй чшйрд, лйоеъшфйд ае рйъез. ббйчеш даерчемевй дшащеп рчбт щмб двйгем елп рбгче д-BMI, зежч щшйш дйг едцшйлд дъжеръйъ. дзечшйн сйееве аъ дощъъфйн мщъй чбецеъ бдъан млоеъ дзмбеп бъжерд: вбедд (отм 1.5 вшн/ч"в/йен) ае роелд (тг 1.5 вшн/ч"в/йен). л-30% одоиефмйн гйеезе тм цшйлъ змбеп вбедд, тн цшйлд ооецтъ щм 2.2 вшн/ч"в/йен мтеоъ 0.8 вшн/ч"в/йен бчбецъ дцшйлд дроелд.
роца лй цшйлд вбедд щм змбеп дййъд чщешд бощк дйщшгеъ ашек йеъш бдщееад мцшйлд роелд – 14.7 мтеоъ 7.3 зегщйн бооецт. ма роца чщш оебдч бйп лоеъ дзмбеп бъжерд мбйп зежч щшйш дйг, вн мазш дъаод сиийсийъ мфтймеъ вефрйъ, цшйлъ амледем, тйщеп, овгш, вйм, щмб двйгем, ийфем аерчемевй, BMI, цшйлд чмешйъ, цшйлъ маецйп ае лоеъ дщеорйн бъжерд.
дзечшйн ослойн лй ъжерд тъйшъ змбеп тщейд мщощ ласишивйд мдашлъ ощк ддйщшгеъ бчшб чщйщйн земй сшип ейщ мащщ жаъ бозчшйн ресфйн.
https://pubmed.ncbi.nlm.nih.gov/32919817/
зжшд мъзймъ дозчшйн
цшйлъ шлйбйн сфцйфййн - фйшеъ ейшчеъ
бсчйшд щйиъйъ щм озчшйн ъцфйъййн (2019) детшк дчщш бйп цшйлъ фйшеъ ойебщйн мбйп дсйлеп мсшип. йщрп тгейеъ шбеъ дчещшеъ бйп цшйлд роелд щм фйшеъ ейшчеъ мбйп сйлеп оевбш мдъфъзеъ сшип, аемн ма йгет одй ддщфтд щм цшйлъ фйшеъ ойебщйн. йщрн дбгмйн рйлшйн бдшлб щм фйшеъ ишййн мтеоъ ойебщйн, аемн йщрп тгейеъ мвбй ддщфтд довйрд щм фйшеъ ойебщйн.
бдъбсс тм дръерйн оъщтд озчшй течбд, роцад ъойлд млк щцшйлд щм отм 3 ореъ фйшеъ ойебщйн бщбет (цйоечйн, щжйфйн еъошйн) дййъд чщешд бйшйгд оебдчъ бсйлеп мдъфъзеъ фемйфйн чемешчимййн ишен-сширййн, мсшип тшоерйъ емъоеъд осшип дмбмб б-24%, 49% е-65%, бдъаод. чщш геод бйп цшйлъ фйшеъ ойебщйн мбйп сйлеп оефзъ мсшип роца брйъез дръерйн ощбтд озчшй очшд-бчшд. ооцайн амд дйе геойн, ае зжчйн йеъш, бдщееад мооцайн мвбй цшйлъ фйшеъ ишййн ае мск цшйлъ дфйшеъ. дзечшйн оцййрйн лй аорн осфш дозчшйн еддишеврйеъ двбедд ма оафщшйн мбцт оид-армйжд, ак дооцайн дчййойн осфчйн ъойлд шащерйъ млк щцшйлъ фйшеъ ойебщйн тщейд мдйеъ чщешд бсйлеп оефзъ мдъфъзеъ сшип ае мъоеъд, емъшен морйтъ сшип ботшлъ дтйлем.
https://www.ncbi.nlm.nih.gov/pubmed/31504082
бсчйшд (2018) офешиеъ дтгейеъ дфшд-чмйрйеъ бдъййзс мдщфтд щм шйоеп (Punica granatum) тм севй сшип щерйн, ъек дъййзсеъ мшлйбйн дфтймйн еорврерй дфтемд, елп дтгейеъ доевбмеъ оозчшйн чмйрййн, ащш дгвйое дщфтд ойийбд мойх шйоеп бчшб оиефмйн тн сшип тшоерйъ есшип отй.
https://www.ncbi.nlm.nih.gov/pubmed/29729421
озчш чмйрй лфем-сойеъ обечш фмсбе (йемй 2015) бе рбгчд ддщфтд щм ойцей шйоеп тм жоп ддлфмд щм огг PSA (огг мдтшлъ дфшеврежд) бчшб вбшйн мазш ийфем бсшип дтшоерйъ.
бозчш рлмме 183 оиефмйн ащш земче мчбецъ ддътшбеъ щчйбмд ойцей режмй щм шйоеп долйм 1.6 оймйоем фемйфреЙмйн ае мчбецъ дфмсбе (мцййп лй чбецъ ддътшбеъ лммд фй 2 йеъш рзчшйн очбецъ дфмсбе).
дзечшйн ма оцае дбгм бйп дчбецеъ бйзс мжоп ддлфмд щм PSA, тмййд о-11.1 зегщйн м- 15.6 зегщйн бчбецъ дфмсбе мтеоъ тмййд о-12.9 зегщйн м-14.5 зегщйн бчбецъ ддътшбеъ.
тн жаъ, роца лй ощъъфйн тн вреийф осев MnSOD AA швйщйн йеъш мдщфтд дойийбд щм ойцей шйоеп, лащш бчшб ощъъфйн амд змд тмййд ощотеъйъ бжоп ддлфмд (1.8 зегщйн бчбецъ дфмсбе мтеоъ 12 зегщйн бчбецъ ддътшбеъ).
http://www.ncbi.nlm.nih.gov/pubmed/26169045
бсчйшд (2016) грйн дзечшйн бфеирцйам дарий-сширй дсйршвйсий щм щймеб шлйбйн щерйн доцеййн бтрбйн, мтеоъ дъочгеъ бшлйб бегг лвеп шжбшишем ае чеешцийп.
https://www.ncbi.nlm.nih.gov/pubmed/26829056
озчш чмйрй шащерй (щмб 1) бе рбгчд ддщфтд щм ойцей чмйфеъ трбй оесчгйп (Vitis rotundifolia) бвбшйн тн дйщреъ щм сшип тшоерйъ щайре вшешъй (оай 2015).
бозчш рлмме 14 вбшйн ащш чйбме аъ ойцей дтрбйн бойреп темд, тн ойреп дъзмъй щм 500-4,000 о"в, ойреп ащш роца биез бозчшйн фшд-чмйрййн.
бщм дтгш ойгт тм штймеъ 4,000 о"в дйд дойреп дочсйомй щрйъп блм ъчефъ дозчш.
дзечшйн тчбе азш дощъъфйн мъчефд щм 6-30 зегщйн бдъан моцб дчмйрй.
бъчефъ дозчш ма геез тм ъефтеъ мееай омбг 4 ощъъфйн щсбме одфштеъ чмеъ ботшлъ дтйлем. 6 обйп дощъъфйн децае одозчш бщм дъчгоеъ дсшип еощъъу ресу бщм дъфъзеъ ойасирйд вшбйс (озмд аеиеайоерйъ доъбиаъ бземщъ щшйшйн), щайррд чщешд мсшип.
жоп ддлфмд щм огг PSA тмд б-5.3 зегщйн (дбгм щайре оебдч сиийсийъ, p=0.17), лмеош рцфд щйфеш богг мсшип жд. дзечшйн огеезйн лй лйен ртшк озчш щмб 2 ачшай обечш фмсбе мдтшлъ дйтймеъ щм ойцей чмйфеъ трбйн бойреп роек (500 о"в) евбед (4,000 о"в).
дтшъ отшлъ: дозчш ма лмм чбецъ бйчешъ емлп ддъййзсеъ мъецаеъ озчш жд дйа оевбмъ. йщ мдоъйп мъецаеъ дозчш обечш дфмсбе.
http://www.ncbi.nlm.nih.gov/pubmed/26012728
бозчш течбд еоид-армйжд (2021) детшк дчщш бйп цшйлъ фйшеъ ейшчеъ мбйп дсйлеп мъоеъд.
шащйъ, дзечшйн рйъзе аъ дръерйн ощрй озчшй течбд вгемйн щртшле башд"б: 66,719 рщйн оозчш дазйеъ (1984-2014) е-42,016 вбшйн оозчш арщй очцетеъ дбшйаеъ (1986-2014). лм дощъъфйн дйе мма дйсиешйд щм ъзмеад чшгйеесчемшйъ, сшип ае селшъ бъзймъ дозчш, едъжерд детшлд баоцтеъ щамерйн щоемае бъзймъ дозчш ефтн башбт щрйн. бодмк ъчефъ дотчб ъетге 33,898 очшй ъоеъд.
роца лй мазш дъаод мовееп вешой сйлеп, цшйлд вбедд йеъш щм фйшеъ ейшчеъ дййъд чщешд бсйлеп роек йеъш мъоеъд олм вешн, елп мъоеъд осшип, ъзмеад чшгйеесчемшйъ еозмеъ рщйод. цшйлд щм лзощ ореъ мйен щм фйшеъ ейшчеъ, ае щъй ореъ щм фйшеъ ещмещ ореъ щм йшчеъ, дййъд чщешд бсйлеп дроек бйеъш мъоеъд, лащш цшйлд вбедд йеъш ма ъшод мдфзъд ресфъ бсйлеп. баефп сфцйфй, бдщееад мцшйлд щм щъй ореъ мйен, цшйлд щм зощ ореъ мйен дййъд чщешд бсйлеп роек б-13% мъоеъд олм вешн, б-12% мъоеъд овешойн чшгйеесчемшййн, б-10% мъоеъд осшип, еб-35% мъоеъд озмеъ рщйод.
бдощк, дзечшйн тшле оид-армйжд длеммъ ръерйн о-26 озчшй течбд, бдн 1,892,885 ощъъфйн е-145,015 очшй ъоеъд. брйъез лемм щм дръерйн роцае ъецаеъ геоеъ, тн сйлеп роек б-13% мъоеъд олм вешн тбеш цшйлд щм зощ ореъ фйшеъ ейшчеъ мйен. шеб чбецеъ дфйшеъ едйшчеъ дйе чщешеъ бсйлеп оефзъ мъоеъд, омбг йшчеъ тоймрййн лвеп аферд еъйшс. цшйлд щм ойцй фйшеъ еъфезй агод ма дййъд чщешд баефп оебдч бсйлеп мъоеъд.
дзечшйн ослойн лй ооцайн амд ъеолйн бдомцеъ мфйдп йщ мтегг мцшйлд вбедд щм фйшеъ ейшчеъ, омбг ойцй фйшеъ еъфезй агод.
https://pubmed.ncbi.nlm.nih.gov/33641343/
озчш фшд-чмйрй (йерй 2016) доцбйт тм дфтймеъ дарий-сширйъ щм семфешафп, шлйб доефч ойшчеъ оцмйбйн, мдврд офрй сшип дфд дчщеш бзщйфд мзеошйн чшцйреврййн.
http://www.ncbi.nlm.nih.gov/pubmed/27339168
тм бсйс ръерйн оашбтд озчшй течбд щртшле бйфп (йреаш 2017), бгче дзечшйн аъ дчщш бйп цшйлъ фйшеъ ейшчеъ мбйп дсйлеп мсшип.
бозчш рлмме дръерйн щм л-200,000 ощъъфйн, лащш бъчефъ отчб щм 9-15 щрд аебзре 17,681 очшй сшип. тм бсйс щамерй ъжерд дзечшйн сйееве аъ шоъ дцшйлд щм фйшеъ ейшчеъ мзощ шоеъ.
баефп лммй, роца лй цшйлъ фйшеъ ае йшчеъ ма дййъд чщешд бсйлеп мсшип, вн бзмечд мвбшйн емрщйн евн лащш тйщеп ецшйлъ амледем рлмме брйъез. ооцай дозчш айрн ъеолйн бъфйсд лй цшйлд вбедд щм фйшеъ ейшчеъ ъешоъ мдфзъъ дсйлеп мсшип бчшб даелмесййд дйфрйъ. дзечшйн оцййрйн лй вн б-3 озчшй течбд вгемйн азшйн щртшле башд"б ебайшефд роца лй цшйлъ йшчеъ ма дййъд чщешд, ае чщешд бойгд роелд оаег, мйшйгд бсйлеп мсшип елй ма роца лмм чщш бйп цшйлъ фйшеъ мбйп дсйлеп мсшип.
дтшъ дотшлъ: ъоед бтйрйре щдзечшйн айрн оцййрйн озчшйн фшефсчийбйн шзбй дйчу щлп делйзе лй цшйлъ йшчеъ ефйшеъ чщешйн бсйлеп роек йеъш мсшип.
https://www.ncbi.nlm.nih.gov/pubmed/28142032
лзмч оозчш айшефай вгем (ребобш 2015), оръерйн щм отм 300,000 рщйн темд лй чййн чщш бйп цшйлъ йшчеъ (ак ма фйшеъ) мбйп сйлеп роек йеъш мсшип дщг, бойезг сшип щмймй мчемирйн дешоермййн.
http://www.ncbi.nlm.nih.gov/pubmed/26607934
лзмч оозчш течбд айшефай вгем, бозчш очшд-бчшд дрелзй (йреаш 2016) рлмме л-1,500 очшйн щм рщйн тн сшип дщг ечбецъ бчшд щм л-1,500 рщйн бшйаеъ. роца лй шйлежйн вбедйн йеъш щм биа-чшеип еамфа-чшеип чщешйн бсйлеп роек йеъш мсшип дщг щмймй мчемирйн дешоермййн.
http://www.ncbi.nlm.nih.gov/pubmed/26791185
озчш ачшай обечш оецмб (аечиебш 2015) бгч аъ ддщфтд щм цшйлъ ъошйн, ащш тщйшйн бфемйфреЙмйн ебсйбйн, тм зййгчй дотй етм дсйлеп мсшип дотй.
дзечшйн оцйтйн лй дчщш бйп цшйлъ ожереъ одцеоз мбйп щлйзеъ роелд йеъш щм сшип дотй тщей мдйеъ оесбш, мфзеъ баефп змчй, тм йгй ддщфтд дощембъ щм сйбйн ма осйсйн ефемйфреЙмйн тм зййгчй дотй.
бозчш дщъъфе 22 оъргбйн бшйайн ащш цшле фмсбе (селш фйшеъ) мощк 21 йойн емазш дфсчд щм 14 йойн цшле ъошйн (7 ъошйн, л-50 вшн). блм ъчефъ дозчш дощъъфйн дощйле аъ дъжерд дшвймд щмдн.
бдщееад мфмсбе, цшйлъ ъошйн ма дебймд мщйреййн оебдчйн бцойзъ зййгчй дотй, аемн роцад тмййд оебдчъ бфтймеъ дотййн еъгйшеъ дйцйаеъ (p<0.01) ейшйгд оебдчъ бшйлеж даоерйд бцеад* (p<0.05) мтеоъ ръерй дбсйс. лое лп, ббгйчъ ой-дцеад рцфъд йшйгд оебдчъ бшоъ дштймеъ дврийъ (genotoxicity) егйлей дщвщев щм ъдмйлйн сширййн (p<0.01).
тм бсйс ооцайн амд ослойн дзечшйн лй цшйлъ ъошйн тщейд мъшен мщойшд тм бшйаеъ дотй емдфзйъ аъ дсйлеп мъдмйлйн ащш чщешйн бдъфъзеъ сшип дотй, вн мма дщфтд тм цойзъ зййгчй дотй.
* даоерйд, щрецшъ лъецад ооибемйжн зййгчй щм змберйн, чщешд бдйеецшеъ сшип.
http://www.ncbi.nlm.nih.gov/pubmed/26428278
бозчш течбд (2019) щртшк бгрошч етесч бъжерд, сшип ебшйаеъ - рбгч дчщш бйп цшйлъ фмбереайгйн бъжерд мбйп дсйлеп мъоеъд. бозчш рлмме дръерйн щм 56,048 ощъъфйн, лащш бодмк ъчефъ отчб щм 23 щрд ъетге 14,083 очшй ъоеъд.
роца лй цшйлд оъерд щм фмбереайгйн бъжерд дййъд чщешд бсйлеп оефзъ мъоеъд олм вешн, елп мъоеъд овешойн чшгйеесчемшййн ае сшип. дчщш дзжч бйеъш роца тбеш цшйлд щм л-500 о"в/йен фмбереайгйн, мма ъшеод ощотеъйъ мцшйлд вбедд йеъш. тег роца лй дчщш дйд зжч йеъш бчшб отщрйн бдщееад мма-отщрйн, ебчшб ощъъфйн тн цшйлъ амледем вбедд (йеъш о-20 вшн/йен) бдщееад мроелд-бйрерйъ (тг 20 вшн/йен).
дзечшйн ослойн лй ооцайн амд огвйщйн аъ дфеирцйам мдфзъъ щйтешй дъоеъд баоцтеъ домцд мдвбшъ дцшйлд щм ожереъ тщйшйн бфмбереайгйн, бгвщ тм овееп фйшеъ ейшчеъ бцбтйн щерйн, бойезг тбеш аелмесйеъ бсйлеп.
https://www.ncbi.nlm.nih.gov/pubmed/31409784
озчш течбд фшесфчийбй (оай 2016) ащш ретг мдтшйк аъ дчщш бйп цшйлъ фйшеъ ейшчеъ бвйм цтйш мбйп дсйлеп мсшип дщг. бозчш рлмме л-90,000 рщйн бвймай 27-44 ащш оймае щамеп ъжерд бщръ 1991 ел-44,000 ртшеъ бвймай 13-18 ащш оймае щамеп ъжерд бщръ 1998.
тг мщръ 2013 аебзре 3,235 очшйн щм сшип щг вшешъй, лащш цшйлъ фйшеъ вгемд йеъш бвйм ддъбвшеъ дййъд чщешд бсйлеп роек йеъш мсшип дщг.
баефп сфцйфй, ртшеъ щцшле л-3 ореъ фшй мйен дйе бсйлеп роек бл-25% бдщееад маме щцшле л-0.5 оръ фшй мйен, мма ъмеъ бцшйлъ дфйшеъ бвйм обевш йеъш. чщш жд дйд ощотеъй йеъш тбеш сшип щмймй мчемирйн дешоермййн бдщееад мзйебй мчемирйн дешоермййн.
ма роца чщш бйп ск цшйлъ дфйшеъ бвйм обевш йеъш, ае ск цшйлъ дйшчеъ, мбйп дсйлеп мсшип дщг. тн жаъ, цшйлд щм фйшеъ ейшчеъ тщйшйн бамфа-чшеип дййъд чщешд бсйлеп роек йеъш мсшип щг мфрй вйм дотбш.
тег роца лй цшйлд шбд йеъш щм ъфезйн, брреъ етрбйн бодмк вйм ддъбвшеъ ещм ъфежйн ечййм бвйм обевш йеъш дййъд чщешд бсйлеп роек йеъш мсшип дщг.
ма роца чщш бйп цшйлъ ойх фйшеъ мбйп дсйлеп мсшип дщг.
ооцайн амд оцбйтйн тм дзщйбеъ щм цшйлъ фйшеъ бчшб ртшеъ бвйм ддъбвшеъ боишд мдфзйъ аъ дсйлеп мсшип дщг.
дтшъ дотшлъ: йшчеъ ефйшеъ тщйшйн бамфа-чшеип дн йшчеъ ефйшеъ цдебйн-лъеойн (вжш, биид, гмтъ, гмешйъ) ейшечйн-лдйн (бшечемй, щтетйъ йшечд, аферд йшечд, ъшг, мфъ, зсд).
http://www.ncbi.nlm.nih.gov/pubmed/27170029
тм бсйс ръерйн оашбтд озчшй течбд щртшле бйфп (йреаш 2017), бгче дзечшйн аъ дчщш бйп цшйлъ фйшеъ ейшчеъ мбйп дсйлеп мсшип.
бозчш рлмме дръерйн щм л-200,000 ощъъфйн, лащш бъчефъ отчб щм 9-15 щрд аебзре 17,681 очшй сшип. тм бсйс щамерй ъжерд дзечшйн сйееве аъ шоъ дцшйлд щм фйшеъ ейшчеъ мзощ шоеъ.
баефп лммй, роца лй цшйлъ фйшеъ ае йшчеъ ма дййъд чщешд бсйлеп мсшип, вн бзмечд мвбшйн емрщйн евн лащш тйщеп ецшйлъ амледем рлмме брйъез. ооцай дозчш айрн ъеолйн бъфйсд лй цшйлд вбедд щм фйшеъ ейшчеъ ъешоъ мдфзъъ дсйлеп мсшип бчшб даелмесййд дйфрйъ. дзечшйн оцййрйн лй вн б-3 озчшй течбд вгемйн азшйн щртшле башд"б ебайшефд роца лй цшйлъ йшчеъ ма дййъд чщешд, ае чщешд бойгд роелд оаег, мйшйгд бсйлеп мсшип елй ма роца лмм чщш бйп цшйлъ фйшеъ мбйп дсйлеп мсшип.
дтшъ дотшлъ: ъоед бтйрйре щдзечшйн айрн оцййрйн озчшйн фшефсчийбйн шзбй дйчу щлп делйзе лй цшйлъ йшчеъ ефйшеъ чщешйн бсйлеп роек йеъш мсшип.
https://www.ncbi.nlm.nih.gov/pubmed/28142032
бозчш течбд (ошх 2016), бе рлмме л-46,000 вбшйн азшйдн бецт отчб щм 23 щрд, роцад ъойлд млк щцшйлъ мйчефп тщейд мъшен мдфзъъ дсйлеп мсшип тшоерйъ осев оемчемшй осейн (TMPRSS2:ERG-positive), ооца дозжч аъ ддщтшд лй мсев сшип жд аийемевйд щерд.
https://www.ncbi.nlm.nih.gov/pubmed/26817504
бсчйшд щйиъйъ еоид-армйжд (2017) безрйн дзечшйн аъ дчщш бйп цшйлъ фйшеъ ейшчеъ мбйп дсйлеп мъзмеад чшгйеесчемшйъ, мсшип емъоеъд, ъек дъййзсеъ мдщфМтъ шоъ дцшйлд емсевйн сфцйфййн щм фйшеъ ейшчеъ.
бсчйшд рлмме 142 фшсеойн, бдн 95 озчшй течбд щерйн тн л-2 оймйеп ощъъфйн. орйъез лемм щм дооцайн темд лй тбеш цшйлд щм 200 вшн фйшеъ ейшчеъ мйен дсйлеп мозмъ мб лмймйъ дйд роек б-8%, б-16% мщбх, б-8% мъзмеад чшгйеесчемшйъ, б-3% мсшип еб-10% мъоеъд. овод геод роцад бдъййзс мцшйлъ фйшеъ ае йшчеъ брфшг. тег роца лй цшйлд вбедд йеъш, щм тг 800 вшн мйен (10 ореъ), ъшод мйшйгд ресфъ бшоеъ дсйлеп.
орйъез дръерйн тм фй цшйлъ фйшеъ ейшчеъ сфцйфййн темд лй цшйлд вбедд йеъш щм ъфезйн еавсйн, фйшеъ дгш, тмйн йшечйн, йшчеъ оцмйбйн есми дййъд чщешд бсйлеп роек йеъш мъзмеад чшгйеесчемшйъ емъоеъд, елй цшйлд вбедд йеъш щм йшчеъ йшечйн ецдебйн ещм йшчеъ оцмйбйн дййъд чщешд бсйлеп роек йеъш мсшип. тм бсйс ооцайн амд, еъзъ ддрзд щдчщшйн щроцае отйгйн тм сйбъйеъ, дзечшйн ошайн лй рйъп мййзс 5.6 оймйеп оочшй дъоеъд доечгоъ бтемн бщръ 2013 мцшйлд дроелд осу щм 500 вшн мйен фйшеъ ейшчеъ, ае 7.8 оймйеп бдъййзс мсу аефийоамй щм 800 вшн мйен.
дзечшйн ослойн лй ооцай дозчш осфчйн ъойлд мдомцеъ емълрйеъ ддътшбеъ дойетгеъ мдвбшъ дцшйлд щм фйшеъ ейшчеъ баелмесййд дшзбд, ласишивйд морйтъ ъзмеад лшерйъ емдфзъъ дсйлеп мъоеъд оечгоъ.
https://academic.oup.com/ije/article/3039477/Fruit
бсчйшд (йреаш 2016) оецвеъ дтгейеъ оозчшйн фшд-чмйрййн бревт мдшлб щм фйшеъ йтш щерйн еорврерй дфтемд щмдн тм осмемйн дчщешйн бдъфъзеъ озмеъ, бгвщ тм сшип, ъдмйлйн гмчъййн, рйееп тцбй, селшъ еозмеъ чшгйеесчемшйеъ.
https://www.ncbi.nlm.nih.gov/pubmed/25872898
бозчш отбгд (фбшеаш 2016) оецвъ ддщфтд довйрд щм 8 жрй ъфезй тх бдъййзс морйтъ оеицйеъ, фтймеъ ревгъ зоцеп едврд офрй ийфемй чшйрд.
https://www.ncbi.nlm.nih.gov/pubmed/26753515
бозчш отбгд (оай 2017) огвйойн дзечшйн аъ дфтймеъ дарий-сширйъ щм щрй жрй твбрйеъ щочешн бгшен айимйд лрвг ъай сшип дчйбд.
https://www.ncbi.nlm.nih.gov/pubmed/28488765
счйшд (йреаш 2015) дтесчъ бфтймеъ дарий-сширйъ щм йшчеъ одсев дбеирй Allium, бгвщ тм щен (Allium cepa) ебцм, ебдщфтд щм дшлйбйн двефшъййн доцеййн бйшчеъ амд.
озчшйн афйгойемевййн оцбйтйн тм чщш бйп цшйлъ йшчеъ оощфзъ дщен мбйп сйлеп роек йеъш мсшип, ебойезг сшип ботшлъ дтйлем. оозчшй отбгд темд лй дшлйбйн двефшъййн ощфйтйн тм дфтймеъ дчшцйреврйъ, дфтймеъ дарий-ойчшебйамйъ етм ъдмйлй дзоцеп бъайн.
бресу роца лй йшчеъ лое щен ебцм ешлйбйдн дфтймйн дйрн бтмй дщфтд ъдмйлйн бйемевййн щерйн етм лм щмбй дъдмйк дсширй елъецад олк тщеййн мдщфйт тм дсйлеп мсшип.
http://www.ncbi.nlm.nih.gov/pubmed/25586902
счйшд (йемй 2014) дослоъ аъ орврерй дфтймеъ дарий-сширййн щм орвйфшйп, фемйфрем доцей борве, еоцйвд аъ дооцайн оозчшйн фшд-чмйрййн тглрййн.
http://www.ncbi.nlm.nih.gov/pubmed/24984103
бсчйшд (2014) роца лй мфмбереайгйн доцеййн бчмйфеъ дгшйн йщрд фтймеъ ревгъ сшип, жаъ тм йгй орйтъ арвйевржйс, орйтъ щмйзъ вшешеъ, тйлеб ъретъ ъай сшип блмй дгн, ефшеафефиежйс.
http://www.ncbi.nlm.nih.gov/pubmed/25250322
озчшйн афйгойемевййн оцбйтйн тм чщш бйп цшйлъ йшчеъ ефйшеъ баефп лммй, ак ма бйп ъшлебеъ фремйеъ осейоеъ, мбйп сйлеп роек йеъш мсшип чемешчимй.
мтеоъ жаъ, озчшйн фшд-чмйрййн бдн ртщд щйоещ бгвйоеъ ъайн ае бзйеъ отбгд оцбйтйн тм дфтймеъ дарий-сширйъ щм ъшлебеъ фремйеъ щочешп бъжерд.
бозчш дрелзй (ошх 2015) безрйн дзечшйн аъ лмм дтгейеъ бйзс мдщфтд дарий-сширйъ щм ъшлебеъ фремйеъ щереъ, ъек дъочгеъ блешлеойп, шжбшишем, айжефмберйн, EGCG, абчъ фим щзеш, ойцей аелорйеъ щзешеъ, ойцей в'йрв'ш еойцей шйоеп.
одсчйшд темд лй лешлеойп дйре дшлйб дъжеръй добийз бйеъш лийфем ъеок бсшип чемешчимй.
дзечшйн ослойн лй баефп лммй озчшйн чмйрййн осфчйн ъойлд чмещд мвбй дйтймеъ щм ъшлебеъ фремйеъ лрвг сшип чемешчимй еосбйшйн лй ргшщйн ойрерйн вбедйн оаег тм оръ мвшен мдщфтд бтмъ ощотеъ чмйрйъ.
http://www.ncbi.nlm.nih.gov/pubmed/25693744
озчш (фбшеаш 2016) щртшк тм тлбшйн ретг мбзеп аъ ддщфтд щм ъжерд тщйшд ббшечемй тм тйлем дщеорйн блбг етм ддъфъзеъ щм лбг щеорй еооайшеъ.
босвшъ дозчш дзечшйн ръре мтлбшйн брй 5 щбетеъ гйаиъ бчшд ае гйаид отшбйъ тъйшъ щеоп еселш, тн ае бмй бшечемй. мазш олп, дзечшйн вшое мтлбшйн мфъз ооайшеъ блбг баоцтеъ джшчд щбетйъ щм зеош дрчша diethylnitrosamine (DEN). роца лй цшйлъ бшечемй дврд офрй дъфъзеъ едзошд щм лбг щеорй лъецад оцшйлъ гйаид отшбйъ елп офрй дъфъзеъ ооайшеъ блбг.
http://www.ncbi.nlm.nih.gov/pubmed/26865652
озчш (сфиобш 2015) щртшк тм зйеъ отбгд ошад лй мфемйслшйгйн офшй дфим дщфтд арий-сширйъ лрвг омреод елп мдвбшъ йтймеъ дъшефд длйоеъшфйъ docetaxel.
http://www.ncbi.nlm.nih.gov/pubmed/26200777
озчш отбгд (2015), догвйн лй щйиъ рре-арчфсемцйд мфемйфреЙмйн офшй дшйоеп овбйшд аъ джойреъ дбйемевйъ щм дфемйфреЙмйн еаъ ддщфтд дарий-сширйъ лрвг ъай сшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/25624761
бозчш отбгд (фбшеаш 2015) роца лй мфишежймйд (Petroselinum crispum) дщфтд ревгъ-зоцеп едщфтд овйрд офрй фвйтд б-DNA, ащш тщейд мсййт борйтъ ъдмйлйн сширййн.
http://www.ncbi.nlm.nih.gov/pubmed/25582089
озчш отбгд (аечиебш 2015) доцбйт тм дфтймеъ дарий-сширйъ щм бирйп (Betanin), шлйб доефч осмч, лрвг щешъ ъай сшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/26463240
бозчш отбгд (2015) роца лй мойцей чмйфъ дшйоеп фтймеъ арий-сширйъ бойезг лрвг ъай сшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/26320438
бозчш отбгд (йемй 2016) роца лй мфемйфреЙмйн доцеййн бойцей чмйфъ дшйоеп дщфтд отлбъ тм ъай сшип длбг баоцтеъ дфштд мозжеш дъа етйгег оееъ ъай.
https://www.ncbi.nlm.nih.gov/pubmed/27120393
бозчш отбгд (йерй 2017) огвйойн дзечшйн аъ дфтймеъ дарий-фшемйфшийбйъ (отлбъ щвщев) щм зойщд жрй бцм очргд лрвг ъай сшип чемешчимй.
https://www.ncbi.nlm.nih.gov/pubmed/28528091
бозчш, добесс тм ръерйн оозчш очшд-бчшд (фбшеаш 2017), рбгч дчщш бйп цшйлъ чшеиреайгйн осевйн щерйн еейиойп C мбйп дсйлеп мсшип дшйаеъ.
баоцтеъ шайереъ расфе дръерйн аегеъ дцшйлд дъжеръйъ щм 49 фйшеъ ейшчеъ бщръййн дазшереъ о-1,105 земй сшип шйаеъ ечбецъ бйчешъ щм 1,449 ощъъфйн бшйайн. роца лй бдщееад мощъъфйн тн цшйлъ дчшеиреайгйн дроелд бйеъш, ощъъфйн тн дцшйлд двбедд бйеъш дйе бсйлеп роек йеъш мсшип шйаеъ, тн сйлеп роек б-34% бдъййзс мбиа-чшеип, 30% мамфа-чшеип, 35% мбиа-чшйфиечсрийп, 25% ммйчефп е-26% мейиойп C.
бдъййзс мотщрйн лбгйн, мцшйлд вбедд щм чшеиреайгйн роцад дщфтд овйрд бчшб вбшйн еайме мцшйлд вбедд щм ейиойп C роцад дщфтд овйрд бчшб рщйн. ооцай дозчш оцбйтйн тм дъшеод щм шлйбйн ревгй зоцеп доцеййн бфйшеъ ейшчеъ мдврд офрй дъфъзеъ сшип дшйаеъ, афйме бчшб отщрйн лбгйн.
https://www.ncbi.nlm.nih.gov/pubmed/28293540
бозчш, щртшк бчшб тлбшйн (йемй 2017), ошайн дзечшйн лйцг цшйлъ твбрйеъ дфзйъд аъ дсйлеп мдъфъзеъ рвтйн сширййн бтеш, бтйчш бчшб тлбшйн жлшйн, ллм дршад бщм ддщфтд довйрд щм дчшеиреайгйн офрй ржчй чшйръ дщощ.
https://www.ncbi.nlm.nih.gov/pubmed/28698610
бозчш течбд фшесфчийбй (сфиобш 2017), щртшк башд"б, рбгч дчщш бйп цшйлъ фмбереайгйн бъжерд мбйп дсйлеп мсшип шащ ецееаш, сшип деещи есшип дчйбд. бозчш рлмме л-470,000 ощъъфйн лащш бъчефъ отчб щм л-12 щрд аебзре 2,453 очшйн щм сшип шащ ецееаш, 1,165 очшйн щм сшип деещи е-1,297 очшйн щм сшип дчйбд.
орйъез ръерй дъжерд щм дощъъфйн темд лй шоъ цшйлъ дфмбереайгйн двбедд бйеъш (зойщеп тмйеп) дййъд биеез щм 438-4211 о"в/йен едроелд бйеъш (зойщеп ъзъеп) биеез щм 0-84 о"в/йен. роца лй ощъъфйн тн цшйлъ дфмбереайгйн двбедд бйеъш, бойезг аръецйарйгйрйн ефмбарерйн, дйе бтмй сйлеп роек б-24% мсшип шащ ецееаш бдщееад мощъъфйн тн дцшйлд дроелд бйеъш. ма роца чщш бйп цшйлъ фмбереайгйн мбйп дсйлеп мсшип деещи ае дчйбд. ооцайн амд оцбйтйн тм дфеирцйам щм ъжерд тщйшд бфмбереайгйн мдфзъъ дсйлеп мсшип шащ ецееаш.
https://www.ncbi.nlm.nih.gov/pubmed/28724656
бозчш отбгд (сфиобш 2016) оегвоъ ддщфтд ревгъ дсшип щм ойцей вев'й бшй (Lycium barbarum) лрвг ъай сшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/26525080
бозчш зък (афшйм 2018) детшлд дъшеод щм ъжерд тщйшд бсейд ебйшчеъ оцмйбйн мдфзъъ ъсойрйн лъецад одийфем бчшб рщйн дозмйоеъ осшип дщг.
бозчш рлмме 192 рщйн ооеца сйрй е-173 рщйн мбреъ оашд"б (чмйфешрйд), щдзмйое осшип щг бщмб 0 тг 3, ащш аебзп бйп дщрйн 2006-2012.
дощъъфеъ оймае щамерй ъжерд едщйбе мщамеп имферй бревт мъсойрйн дщерйн дчщешйн бийфем (рйъез, лйоеъшфйд, дчшреъ еийфем ъшефъй), лемм ъсойрй вйм дотбш (вмй зен, джтеъ мймд, йебщ бршъйч едфшщеъ одршъйч), бтйеъ офшчйн, тййфеъ, рщйшъ щйтш ебтйеъ жйлшеп.
баефп лммй иеез дцшйлд щм сейд ещм йшчеъ оцмйбйн рт бйп 0 мбйп 431 е-865 вшн/йен, бдъаод, едйд вбед йеъш бчшб рщйн ооеца сйрй. цшйлд вбедд йеъш щм сейд дййъд чщешд бсйлеп роек йеъш мъсойрй вйм дотбш етййфеъ, лащш бдщееад мрщйн щма цшле сейд, цшйлд щм отм 24 вшн/йен дййъд чщешд бсйлеп роек б-49% еб-57%, бдъаод.тн жаъ, брйъез мфй щййлеъ аърйъ, чщш жд роца оебдч шч тбеш рщйн мбреъ ема тбеш рщйн ооеца сйрй.
бдъййзс мцшйлъ йшчеъ оцмйбйн, роца лй бдщееад мцшйлд роелд (тг 33 вшн/йен) цшйлд вбедд (отм 70 вшн/йен) дййъд чщешд бсйлеп роек б-50% мсбем оъсойрй вйм дотбш бчшб лмм дрщйн. дзечшйн ослойн лй бчшб рщйн дозмйоеъ осшип щг, цшйлд вбедд йеъш щм оецшй сейд ещм йшчеъ оцмйбйн дййъд чщешд бшод роелд йеъш щм ъсойрй вйм дотбш етййфеъ лъецад одийфем дарий-сширй. https://www.ncbi.nlm.nih.gov/pubmed/29230660
зжшд мъзймъ дозчшйн
цшйлъ шлйбйн сфцйфййн - сйбйн ъжеръййн
бсчйшд очйфд ощръ 2025 детшк дчщш бйп цшйлъ сйбйн ъжеръййн мбйп дсйлеп мдъфъзеъ, дйщреъ ае ъоеъд осевйн щерйн щм сшип. дсчйшд дъбссд тм ръерйн о-26 оид-армйжеъ щм озчшйн ъцфйъййн, щлмме 52 оггй ъецад щерйн. дооцайн оцбйтйн тм лк щъжерд тщйшд бсйбйн ъжеръййн чщешд бдфзъъ дсйлеп мсшип ботшлеъ дтйлем, дшбййд едщъп, лемм сшип деещи, дчйбд, дмбмб, дотй, фй дибтъ, дщг, дщзмеъ, дтшоерйъ ещмфезйъ дщъп. баефп сфцйфй, цшйлъ сйбйн дййъд чщешд бсйлеп роек б-26% мсшип дотй, 12% бсйлеп мсшип чемешчимй, е-47-50% бсйлеп мсшип еещи осевйн щерйн.
тн жаъ, цшйлд вбедд щм сйбйн огврйн роцад лчщешд мтмййд бсйлеп мдъфъзеъ сшип длмйеъ едшзн. рйъез мфй ойреп дшад лй тмййд йеойъ щм 2.5, 5 ае 10 вшн бцшйлъ дсйбйн дбйад мщйреййн рйлшйн бшоъ дсйлеп мсшип, лащш иеез цшйлд щм 7-36 вшн мйен роца лйтйм бйеъш борйтъ сшип дотй. дзечшйн ослойн лй ъжерд тщйшд бсйбйн ъжеръййн тщейд мдфзйъ аъ дсйлеп мдъфъзеъ севйн щерйн щм сшип емщфш аъ одмк дозмд. мфйлк, ооцай дсчйшд огвйщйн аъ зщйбеън щм сйбйн ъжеръййн ллмй ошлжй борйтд ебийфем бсшип.
https://foodandnutritionresearch.net/index.php/fnr/article/view/11034/18662
оозчш течбд вгем щлмм л-90,000 рщйн (ошх 2016) темд лй ъжерд тщйшд бсйбйн ъжеръййн бвйм цтйш омеед бсйлеп оефзъ мсшип дщг бдощк дзййн.
http://pediatrics.aappublications.org/content/early/2016/01/28/peds.2015-1226
счйшд щйиъйъ еоид-армйжд (оай 2016) бд рбгч дчщш бйп цшйлъ гврйн долймйн сйбйн ъжеръййн мбйп щйтешй дъоеъд овешойн щерйн. бсчйшд рлмме 14 озчшй течбд фшесфчийбййн бдн рбгч дчщш бйп цшйлъ сйбйн мбйп дсйлеп мъоеъд олм вешн (48,052 очшйн), мъоеъд овешойн чшгйеесчемшййн (16,882 очшйн), мъоеъд осшип (19,489) емъоеъд оозмеъ гмчъйеъ (1,092 очшйн).
роца лй бдщееад мощъъфйн тн цшйлъ дсйбйн дроелд бйеъш, амд тн дцшйлд двбедд бйеъш дйе бсйлеп роек б-19% мъоеъд олм вешн еб-18% овешойн чшгйеесчемшййн.
тег роца лй ллм щцшйлъ дсйбйн дййъд вбедд йеъш, лк дсйлеп мсшип дйд роек йеъш. ма роца чщш бйп цшйлъ сйбйн мбйп ъоеъд оозмеъ гмчъйеъ.
http://www.ncbi.nlm.nih.gov/pubmed/27193606
бозчш отбгд (йреаш 2016) дегвод дфтймеъ дарий-сширйъ щм ойцей рби зйид оеъсс, дролш ъзъ дщн досзшй Avemar. орвреп дфтемд чщеш мфтймеъ ревгъ зоцеп емаеиефавйд лъецад офвйтд боибемйжн щм дъа дсширй.
https://www.ncbi.nlm.nih.gov/pubmed/27245162
бозчш отбгд (гцобш 2016) оецвъ ддщфтд дотлбъ щм зеоцд амвйъ, доефчъ оойцей чмйфъ шйоеп, тм ъай сшип цееаш дшзн.
https://www.ncbi.nlm.nih.gov/pubmed/27941714
бозчш течбд (ребобш 2017) рбгч дчщш бйп цшйлъ гйаид тщйшд бсйбйн мазш абзеп сшип чемешчимй, мбйп дсйлеп мъоеъд. тм бсйс щрй озчшй течбд вгемйн, щртшле башд"б, бозчш дрелзй рлмме 1,575 земй сшип чемешчимй бщмб 1-3. цшйлъ дсйбйн детшлд баоцтеъ щамерй ъжерд щдощъъфйн оймае 6 зегщйн е-4 щрйн мазш абзеп дозмд. бодмк ъчефъ отчб зцйерйъ щм 8 щрйн, 773 одощъъфйн рфише, 174 одн лъецад осшип чемешчимй.
баефп лммй, роца лй цшйлъ сйбйн вбедд дййъд чщешд бсйлеп роек йеъш мъоеъд, лащш тбеш лм тмййд щм 5 вшн бцшйлъ дсйбйн дсйлеп дйд роек б-22% мъоеъд осшип чемшчимй еб-14% мъоеъд олм вешн. мцшйлъ сйбйн щочешн бгврйн дййъд ддщфтд дойийбд двбедд бйеъш, лащш мсйбйн щочешн бйшчеъ роцад ъшеод роелд йеъш. ма роца чщш бйп сйбйн щочешн бфйшеъ мбйп дсйлеп мъоеъд. ооцайн амд огвйщйн аъ зщйбеъ дъжерд мазш абзеп озмъ дсшип мщйфеш щйтеш ддйщшгеъ.
https://www.ncbi.nlm.nih.gov/pubmed/29098294
бозчш отбгд (йерй 2017) детшлд дфтймеъ дфшочемевйъ щм тщб зйид бцешеъ ойцей щереъ, бгвщ тм дфтймеъ дарий-фшемйфшийбйъ лрвг ъай сшип длбг.
https://www.ncbi.nlm.nih.gov/pubmed/28605975
зжшд мъзймъ дозчшйн
цшйлъ шлйбйн сфцйфййн - гврйн омайн
дъшеод щм гврйн омайн мдврд офрй озмеъ лбг
бсчйшд щйиъйъ еоид армйжд ощръ 2024 рзчш дчщш бйп цшйлъ гврйн омайн есйбйн ъжеръййн мбйп озмеъ лбг лшерйеъ.
дсчйшд лммд 28 озчшйн ъцфйъййн, лемм 11 озчшй течбд, 8 озчшй зък е-7 озчшй очшд-бйчешъ, бдн отм м-2 оймйеп ощъъфйн.
бшеб дозчшйн рбгч дчщш бйп цшйлъ гврйн омайн есйбйн мбйп дсйлеп мозмъ лбг щеорй ма амледемйъ емсшип лбг.
брйъез лемм щм дръерйн роца лй дсйлей мсбем оозмъ лбг лшерйъ дйд роек б-10% бчшб дощъъфйн тн дцшйлд двбедд бйеъш щм гврйн омайн бйзс маме тн дцшйлд дроелд бйеъш.
тег роца лй дсйлей дйд роек б-35% бчшб дощъъфйн тн цшйлъ дсйбйн двбедд бйеъш, мтеоъ дроелд бйеъш.
брйъез мфй севйн щерйн щм озмеъ лбг, роца лй дъетмъ дощотеъйъ бйеъш мцшйлъ гврйн омайн дййъд бдъййзс мсйлей мсбем ощзоъ лбг елп бдъййзс мъоеъд тм шчт озмеъ лбг.
дзечшйн ослойн лй ъжерд тщйшд бгврйн омайн ебсйбйн тщейд мдйеъ йтймд мдфзъъ дсйлеп мозмеъ лбг лшерйеъ.
https://pubmed.ncbi.nlm.nih.gov/39264371/
дчщш бйп цшйлъ гврйн омайн мбйп сшип шйаеъ
бозчш течбд ощръ 2025 рбгч дчщш бйп цшйлъ гврйн омайн мбйп дсйлеп мдъфъзеъ сшип шйаеъ.
дозчш лмм ощъъфйн бвйм 55 тг 74 о-10 ошлжйн шфеаййн бшзбй ашд"б. дощъъфйн земче ачшайъ мчбецъ ддътшбеъ щтбшд бгйчеъ счш мвймей оечгн щм мсшип тшоерйъ, шйаеъ, чемешчимй ещзмеъ, ае мчбецъ дбйчешъ щчйбмд ийфем сиргший бмбг.
дтшлд ъжеръйъ бецтд бъзймъ ъчефъ дотчб, ебрйъез дрелзй рлмме шч очшйн щм сшип шйаеъ щаещше ббгйчд фъемевйъ.
бодмк ъчефъ отчб зцйерйъ щм л-12 щрйн, ъетге 1,706 очшй сшип шйаеъ оъек 101,732 ощъъфйн, оъелн 86.3% аебзре лсшип шйаеъ осев NSCLC-13.7% лсшип осев SCLC.
дцшйлд дооецтъ щм гврйн омайн тогд тм 17.7 вшн мйен, едощъъфйн сееве машбт шоеъ цшйлд. бчбецъ дцшйлд двбедд бйеъш, дцшйлд дйеойъ дййъд отм 23 вшн мйен, бтег щбчбецъ дцшйлд дроелд бйеъш дцшйлд тогд тм тг 1 вшн азг мйен.
ооцай дозчш дтме лй ощъъфйн бчбецъ дцшйлд двбедд бйеъш дйе бсйлеп роек б-16% мсшип шйаеъ баефп лммй, еб-17% мсшип осев NSCLC, бдщееад мчбецъ дцшйлд дроелд бйеъш.
ма роца чщш оебдч бйп цшйлъ гврйн омайн мбйп дсйлеп м-SCLC.
дъецаеъ реъше тчбйеъ вн мазш дъаод мвешойн оътшбйн феирцйамййн лвеп вйм, ойп, BMI, тйщеп, цшйлъ амледем едйсиешйд ощфзъйъ.
дзечшйн ослойн лй роцад ъойлд млк щъжерд тщйшд бгврйн омайн чщешд бсйлеп оефзъ мдъфъзеъ сшип шйаеъ, ебтйчш сшип осев NSCLC.
дн оцйтйн осфш орврерйн бйемевййн афщшййн дтщеййн мдсбйш аъ дчщш:
- дфзъъ гмчъ отшлъйъ – баоцтеъ фтймеъп щм зеоцеъ щеоп чцшеъ щшщшъ (SCFAs) щмдп ълереъ ревгеъ гмчъ еревгеъ сшип.
- щйфеш бфтймеъ отшлъ дзйсеп – ъсйсъ сйбйн ъжеръййн тм йгй зййгчй дотй оййцшъ SCFAs, дъешоеъ дп мбшйаеъ дотй едп мщйфеш ъфчег отшлъ дзйсеп байбшйн ошезчйн, лемм дшйаеъ.
- аешз зййн бшйа – арщйн щцешлйн гврйн омайн реийн маешз зййн бшйа йеъш, доъафййп бщмйид вмйчойъ иебд йеъш ешоеъ айрсемйп роелеъ, вешойн дчщешйн бсйлеп оефзъ мдъфъзеъ сшип.
- ълемъ ревгй зоцеп вбедд – гврйн омайн одеейн очеш меейиойрйн, ойршмйн ешлйбйн ревгй зоцеп, дотлбйн ъдмйлй зоцеп дчщешйн бдъфъзеъ сшип.
https://pubmed.ncbi.nlm.nih.gov/39810211/
цшйлъ шлйбйн сфцйфййн - ожеп оп дзй
бсчйшд очйфд ощръ 2025 детшле ддщфтеъ дбшйаеъйеъ щм цшйлъ бйцйн. бсчйшд рлмме 14 счйшеъ щйиъйеъ еоид-армйжеъ, одп 10 счйшеъ добессеъ тм озчшйн ъцфйъййн е-4 счйшеъ добессеъ тм озчшйн обечшйн. дзечшйн тшле рйъез лемм щм дръерйн мдтшлъ дчщш бйп цшйлъ бйцйн мбйп овееп оггйн бшйаеъййн, ебдн: сйлеп мъоеъд лммйъ, ъоеъд еъзмеад чшгйеесчемшйъ, ъоеъд осшип, оггйн оибемййн (сйлеп мселшъ, фшефйм щеорйн, оггйн аръшефеоишййн емзх гн) еъоеъд оозмеъ рщйод. одооцайн тмд лй цшйлд вбедд щм бйцйн дййъд чщешд бсйлеп вбед б-15% май-сфйчъ мб емсйлеп вбед б-13% мъоеъд осшип. лое лп, роца чщш мшоеъ вбедеъ йеъш щм лемсишем лммй, LDL е-ApoB100. бресу, роцае вн чщшйн зйебййн, лемм щйфеш бшоеъ HDL е-ApoA1 еъшеод мвгймд ъчйрд бчшб ймгйн. ма роцае чщшйн оебдчйн сиийсийъ бйзс моггйн дбшйаеъййн дазшйн щрбгче. тн жаъ, дзечшйн огвйщйн лй айлеъ дооцайн длммйъ роелд, бйп дйъш бщм дишеврйеъ ощотеъйъ бйп дозчшйн еайлеъ оъегемевйъ оевбмъ. мфйлк, дн ослойн лй ма роца бйсес мдйортеъ оцшйлъ бйцйн еоцйтйн лй рйъп мщмб бйцйн лзмч оъжерд бшйад еоаежръ, аемн оомйцйн тм тшйлъ озчшйн обессйн еайлеъййн йеъш лгй мдтшйк аъ ддщфтеъ дбшйаеъйеъ щм цшйлъ бйцйн. дзечшйн огеезйн тм дтгш ойоеп зйцерй мозчш етм дтгш рйвегй айришсйн.
https://pubmed.ncbi.nlm.nih.gov/39934049/
бсгшъ оаошйн, (2019) щфешсое дзегщ блъб дтъ Annals of Internal Medicine, оецв сйлен дтгейеъ еддомцеъ бдъййзс мдщфтд дбшйаеъйъ щм цшйлъ бщш аген еотебг. доаошйн фешсое тм йгй чбецъ оеозйн ощбт огйреъ, ащш дтшйле аъ дтгейеъ дозчшйеъ дчййоеъ бъдмйк оъегемевй щйиъй ебдъан млммйн дочебмйн щм чбйтъ зежч ешоъ дбйизеп щм дооцайн. досчрд длммйъ щм дзечшйн дйа лй айп ъойлд озчшйъ млк щмдфзъъ дцшйлд щм бщш аген еотебг йщрд ъетмъ бшйаеъйъ, емитрън обевшйн йлемйн мдощйк емцшек бщш бдъан мдтгфеъ емдшвмйн дайщййн. осчреъ амд обессеъ тм ашбт счйшеъ щйиъйеъ, бдп детшлд ддщфтд дбшйаеъйъ щм бщш аген еотебг тм дбшйаеъ, етм счйшд щйиъйъ ресфъ, дтесчъ бтшлйн ебдтгфеъ дайщйеъ дчщешйн бъжерд ебшйаеъ.
мдмп фйшеи дооцайн дтйчшййн:
- йщрн шч озчшйн обечшйн беггйн, бдн детшлд ддщфтд щм цшйлъ бщш вбедд мтеоъ роелд. бсчйшд щйиъйъ щртшлд, дзечшйн оъбссйн бтйчш тм озчш азг, бе рлмме 48,835 рщйн. оозчш жд темеъ тгейеъ бшоъ бйизеп роелд, дошаеъ лй мцшйлд роелд щм бщш аген ма дййъд дщфтд оебдчъ тм щйтеш дъоеъд длммй етм щйтеш дъзмеад едъоеъд оозмеъ мб елмй гн еосшип (лемм сшип чемешчимй есшип дщг).
- брйъез дръерйн о-105 озчшй течбд, бдн мотмд о-6 оймйеп ощъъфйн, роцае тгейеъ бшоъ бйизеп роелд млк щъжерд, длеммъ шод роелд щм бщш аген ещм бщш отебг, чщешд бйшйгд чирд оаег бсйлеп мъзмеад емъоеъд лъецад овешойн чшгйе-оибемййн ае осшип.
- баефп сфцйфй, йщрп тгейеъ бшоъ бйизеп роелд оаег млк щдфзъъ щмещ ореъ мщбет бцшйлд щм бщш аген ещм бщш отебг чщешд бйшйгд роелд оаег бсйлеп мъоеъд олм вешн, мъзмеад еъоеъд чшгйеесчемшйъ емдъфъзеъ селшъ сев 2 (бдчщш щм селшъ огебш бдфзъд щм 12 очшй селшъ млм 1000 айщ бощк 10 щрйн).
- брйъез дръерйн ощмещйн озчшй течбд, ащш гйеезе тм щйтеш дъоеъд осшип, ещоерйн озчшй течбд, ащш гйеезе тм щйтеш дъзмеад бсшип, роцае тгейеъ бшоъ бйизеп роелд ае роелд оаег млк щдфзъъ щмещ ореъ мщбет бцшйлд щм бщш аген ещм бщш отебг чщешд бйшйгд оетид оаег бсйлеп мъзмеад ае мъоеъд осшип бодмк дзййн.
- бдъбсс тм тгейеъ айлеърйеъ елоеъйеъ, дзечшйн ослойн лй арщйн дцешлйн ъжерд аеорйбешйъ рдрйн оалймъ бщш, отшйлйн лй бщш одеед змч ошлжй бъжерд бшйад еоаойрйн лй айп мдн аъ длйщешйн дргшщйн мдлйп ашезд осфчъ мма бщш, ебаефп лммй айрн отерййрйн бщйрей дшвмй алймъ дбщш щмдн.
дзечшйн дщерйн чйбме ойоеп овефй бшйаеъ маеоййн ебйрмаеоййн, лгевоъ д- WHO, елп ъойлд ма лмлмйъ, щайрд чщешд мозчш, оойчшесефи еаоажеп.
дтшъ отшлъ: озчш жд тешш озмечъ вгемд бчдймд дшфеайъ, лемм зечшйн бдшееашг, щцййре лй ооцай дозчш едосчреъ оревгйн мчеейн орзйн щсйфче маешк ъчефд ашелд оеозйн бъзеой дшфеад дщерйн, щдомйце мцоцн бцшйлъ бщш аген ебщш отебг тчб дчщш щоцае бцшйлд жаъ тн сшип едефтъ озмеъ мб ейшйгд ббшйаеъ дмб. зщеб мцййп лй йщрп дсъййвеъ ебйчешъ оитн арщй дочцет бревт мфшщреъ дсиийсийъ щм дооцайн. лк мощм, дооцайн бревт мселшъ сев 2, ащш децве лбтмй ощотеъ йшегд, айрн ишйеейамйн лщогебш бозмд лд рфецд. лое лп, йщрд бйчешъ тм дозчш дшргеомй добечш дйзйг тмйе дн рщтре, ащш бгч овееп ожереъ тъйшй щеоп ема бщш баефп ойезг, еблмм, дътмоеъ оозчшйн вгемйн щчййойн еофшйлйн аъ дооцайн щмдн.
азг дзщгеъ дтемйн деа рйвег трййрйн, щлп дзечш дшащй, бшагмй вЧерсеп, дйд отешб бтбш бчбецд осзшйъ вгемд, щлммд вн збшеъ ъшефеъ езбшд мййцеш бщш отебг.
https://www.ncbi.nlm.nih.gov/pubmed/31569235
https://www.ncbi.nlm.nih.gov/pubmed/31569236
https://www.ncbi.nlm.nih.gov/pubmed/31569217
https://www.ncbi.nlm.nih.gov/pubmed/31569213
https://www.ncbi.nlm.nih.gov/pubmed/31569214
https://www.ncbi.nlm.nih.gov/pubmed/31569219
бозчш течбд (2021) щртшк башд"б, рбгч дчщш бйп цшйлъ змбеп оочешеъ щерйн ебйп дсйлеп мъоеъд, бчшб рщйн мазш вйм дотбш. ддрзйеъ дъжеръйеъ оъочгеъ блоеъ дзмбеп, аемн дзечшйн иетрйн лй дрзйеъ амд дйрп фщирйеъ, ема осфйчеъ щлп айрп леммеъ дъййзсеъ мочеш дзмбеп. бозчш рлмме дръерйн щм 102,521 рщйн, щвейсе мозчш бйп дщрйн 1993-1998, тн отчб тг мщръ 2017. бодмк ъчефъ дотчб ъетге 25,976 очшй ъоеъд.
мдмп дооцайн дтйчшййн бдщееад бйп дцшйлд двбедд мтеоъ дроелд бйеъш:
-
цшйлъ змбеп одцеоз дййъд чщешд бсйлеп роек б-9% мъоеъд олм вешн, б-12% мъоеъд овешойн чшгйеесчемшййн, еб-21% мъоеъд огорцйд.
-
цшйлъ бщш аген ебйцйн дййъд чщешд бсйлеп вбед б-6% еб-14%, бдъаод, мъоеъд олм вешн.
-
цшйлъ бщш аген ма отебг, бйцйн еоецшй змб, дййъд чщешд бсйлеп вбед б-12%, 24% е-11%, бдъаод, мъоеъд овешойн чшгйеесчемшййн.
-
цшйлъ бйцйн дййъд чщешд бсйлеп вбед б-10% мъоеъд осшип.
-
цшйлъ бщш аген отебг дййъд чщешд бсйлеп вбед б-20% мъоеъд огорцйд, бтег щцшйлъ теу ае бйцйн дййъд чщешд бсйлеп роек б-15% еб-14%, бдъаод.
-
брйъез сиийсий роца, лй дзмфд щм змбеп одзй бзмбеп одцеоз ъшод мдфзъд щм дсйлеп мъоеъд олм вешн, овешойн чшгйеесчемшййн еогорцйд, едзмфд щм бщш аген, бйцйн ае оецшй змб бавежйн, дййъд чщешд бдфзъъ дсйлеп мъоеъд олм вешн.
дзечшйн ослойн лй ооцайн амд огвйщйн аъ дзщйбеъ щм дъййзсеъ мочеш дзмбеп бдрзйеъ дъжеръйеъ.
https://pubmed.ncbi.nlm.nih.gov/33624505/
бозчш очшд-бчшд (сфиобш 2016) рбгч дчщш бйп цшйлъ оецшй змб, мчиеж, сйгп еейиойп D мбйп дсйлеп мсшип дщзмеъ бчшб рщйн афше-аошйчайеъ.бозчш рлмме 490 рщйн тн сшип дщзмеъ ечбецъ бчшд щм 656 рщйн бшйаеъ тн оафййрйн сецйе-гоевшфййн геойн. дръерйн расфе баоцтеъ шайеп имферй щлмм ръерйн гоевшфййн, дйсиешйд айщйъ еощфзъйъ щм сшип, ръерйн ощфзъййн бреща фешйеъ, щйоещ бъшефеъ, оафййрй аешз зййн еойгт дчщеш сфцйфйъ мрщйн афше-аошйчайеъ лвеп фйворицйд, ъфйсеъ аегеъ афмйд еаоереъ ъшбеъйеъ елп баоцтеъ оймей тцой щм щамерй ъжерд. роца лй рщйн щцшле аъ дшод двбедд бйеъш щм змб ома ещм мчиеж дйе бсйлеп лфем мсшип дщзмеъ орщйн щцшле аъ дшод дроелд бйеъш, аемн ма роца чщш бйп змб гм-щеоп, вбйрд ае йевеши. цшйлъ сйгп (одъжерд ае оъесфйн) дййъд чщешд бсйлеп роек йеъш мсшип дщзмеъ (цшйлд щм отм 1200 о"в мйен дййъд чщешд бсйлеп роек бл-49% бдщееад мцшйлд щм тг 478 о"в мйен), аемн ма роца чщш бйп цшйлъ ейиойп D мбйп дсйлеп мсшип дщзмеъ. бресу, зщйфд шбд йеъш мщощ бзегщй дчйх щм отм 23 щтеъ бщбет бзегщй дчйх дййъд чщешд бсйлеп роек бл-29% бдщееад мфзеъ о-6 щтеъ бщбет. дзечшйн ослойн лй тм бсйс ооцайн амд ъжерд тщйшд бсйгп егмд бмчиеж, елп зщйфд осфчъ мщощ, тщейд мдфзйъ аъ дсйлеп мсшип дщзмеъ бчшб рщйн афше-аошйчайеъ.
https://www.ncbi.nlm.nih.gov/pubmed/27632371
лзмч оозчш вгем дтесч бсшип дтшоерйъ, бозчш дрелзй рбгчд ддщтшд мфйд цшйлд вбедд щм щеоп шеей чщешд бсшип тшоерйъ авшсйбй йеъш, елй чщш жд дйре ъмей бщйоещ бсиийрйн. обйп 1,854 земй сшип дтшоерйъ щрлмме бозчш, 321 сееве тн сшип тшоерйъ авшсйбй ейъш дземйн щйоще лчбецъ дщееад. роца лй цшйлъ щеоп шеей вбедд дййъд чщешд бсйлеп вбед бл-50% мсшип тшоерйъ авшсйбй. чщш жд дйд ъмей бщйоещ бсиийрйн, лк щземйн щриме сиийрйн дйе бсйлеп роек йеъш бдщееад мземйн щма риме сиийрйн.цшйлъ лемсишем вбедд йеъш дййъд чщешд бсйлеп вбед мсшип тшоерйъ авшсйбй шч бчшб аошйчайн ооеца айшефй, ак ма бчшб афше-аошйчайн. тег роца лй цшйлд вбедд йеъш щм щеоп шб бмъй шеей дййъд чщешд бсйлеп роек йеъш мсшип тшоерйъ авшсйбй, ак чщш жд ма дйд оебдч сиийсийъ. ма роца чщш бйп сшип тшоерйъ авшсйбй мбйп цшйлъ щеоп зг бмъй шеей ае щеоп ишарс.
https://www.ncbi.nlm.nih.gov/pubmed/27595916
бозчш бе рлмме 659 земй сшип лмйеъ ечбецъ бчшд щм 699 ощъъфйн бшйайн (ребобш 2015) роца лй цшйлъ бщш чщешд бсйлеп оевбш мсшип лмйеъ, ллм дршад лъецад озщйфд мзеошйн дрецшйн бъдмйк дбйщем йзг тн швйщеъ врийъ оевбшъ мзеошйн амд.
http://www.ncbi.nlm.nih.gov/pubmed/26551148
счйшд (2015) щртшлд тм йгй зечшйн йщшамййн оъзен дшфеад дайрившийбйъ оцйвд аъ дтгейеъ мвбй дфтймеъ дшфеайъ щм тщб зйид егрд бфтш бйп ооцайн бозчшйн фшд-чмйрййн маме щроцае бозчшйн чмйрййн. шащйъ оцййрйн дзечшйн лй йщрн йъшереъ бшйаеъййн шбйн дойезсйн мтщб зйид ащш олйм овееп шлйбйн фтймйн: лмешефйм, фмбереайгйн еейиойрй C е-E.
йщрп осфш цешеъ щйоещ мтщб зйид, лемм ойх ишй ае чфеа, ибмйеъ ае абчд лащш ддшлб ощърд бдъан мъдмйк дййцеш емърай двйгем.
озчшй отбгд тм гвйоеъ ъайн ошайн лй мтщб зйид дщфтд арий-сширйъ, ллм дршад бщм дщфтд тм ъдмйлй оееъ ъай. оозчшйн бзйеъ отбгд темд лй мтщб зйид ъшеод морйтд емийфем бсшип елп дщфтд ойийбд тм дфтймеъ дзйсерйъ едфтймеъ ревгъ дзоцеп. озчшйн чмйрййн оцбйтйн тм лк щтщб зйид тщей мдвбйш аъ йтймеъ дийфем длйоеъшфй емдфзйъ ъефтеъ мееай дчщешеъ бийфем, бресу мдщфтд ойийбд боцбйн щм гмчъ офшчйн щвшерйъ, чемйийс, озмеъ доиемевйеъ, селшъ, дщорд етчд зоцерйъ. тн жаъ, огебш бозчшйн чирйн тн фвойн оъегемевййн.
босвшъ дсчйшд ма жеде ъефтеъ мееай зшйвеъ дчщешеъ бщйоещ бтщб зйид аемн бзмч оцешеъ дщйоещ тме бтйеъ щм сбймеъ. дзечшйн ослойн лй йщ мдощйк ембзеп аъ дъетмъ щм тщб зйид бозчшйн чмйрййн вгемйн йеъш тм оръ щрйъп йдйд мчбет домцеъ мщйоещ чмйрй.
http://www.ncbi.nlm.nih.gov/pubmed/26156538
бсчйшд очйфд (сфиобш 2016) оебаеъ дтгейеъ дтглрйеъ оозчшй течбд фшесфчийбййн бревт мдщфтеъ дщмймйеъ щроцае чщешеъ бцшйлъ бщш аген, бгвщ тм ъзмеад лшерйъ лвеп селшъ, озмъ мб лмймйъ, ай сфйчъ мб, щбх, сшип еъоеъд.
дзечшйн ослойн лй бдъбсс тм мфзеъ 6 озчшйн, цшйлд щм 100 вшн бщш ма отебг бйен дййъд омеед бсйлеп вбед йеъш мъзмеад (сйлеп вбед бл-11% мщбх емсшип дщг, 15% мъоеъд овешойн чшгйеесчемшййн, 17% мсшип чемешчимй е-19% мсшип тшоерйъ оъчгн), ан лй ма блм дозчшйн дооцайн дйе оебдчйн сиийсийъ.
цшйлд щм 50 вшн мйен бщш отебг дййъд омеед бсйлеп вбед йеъш баефп оебдч сиийсийъ мошбйъ дозмеъ длшерйеъ щрбгче (4% мсшип дтшоерйъ, 8% мъоеъд осшип, 9% мсшип дщг, 18% мсшип чемешчимй, 19% мсшип мбмб, 13% мщбх, 22% мъоеъд олм вешн, 24% мъоеъд овешойн чшгйеесчемшййн, 32% мселшъ).
тег офшийн дзечшйн одн дорврерйн дбйемевййн ащш тщеййн мтоег ббсйс дчщш бйп цшйлъ бщш мъзмеад лшерйъ елп грйн бдщфтеъ дсбйбъйеъ щм ътщййъ дбщш, лвеп фмйиъ вжй зоод, щйоещ бочешеъ аршвйд оълмйн, щйоещ бойн ефвйтд байлеъ дойн.
дзечшйн ослойн лй рйъп мдсйч щцшйлд вбедд щм бщш аген, ебойезг бщш отебг, чщешд бсйлеп оевбш мосфш озмеъ лшерйеъ емъоеъд оечгоъ едйрд бтмъ дщфтд ощотеъйъ тм дсбйбд. мфйлк, йщрп огйреъ байшефд ащш домйце тм цоцен дцшйлд щм бщш аген лзмч оддрзйеъ дъжеръйеъ дзгщеъ.
https://www.ncbi.nlm.nih.gov/pubmed/27597529
брйъез лемм щм озчшй течбд фшесфчийбййн (йемй 2017) рбгч дчщш бйп севйн щерйн щм щеоп бъжерд мбйп дсйлеп мсшип шйаеъ. дзечшйн осбйшйн лй мъжерд тъйшъ щеоп ъфчйг бдъфъзеъ ъдмйлйн сширййн бшйаеъ, аемн дооцайн оозчшйн афйгойемевййн айрн тчбййн.
бозчш дрелзй рлмме дръерйн отщшд озчшйн, бдн лоймйеп езцй ощъъфйн ел-18,000 очшйн щм сшип шйаеъ - бъчефъ отчб ооецтъ щм 9.4 щрйн. роца лй бдщееад мощъъфйн тн дцшйлд дроелд бйеъш, цшйлд вбедд щм щеоп баефп лммй (38% одчмешйеъ) ещм щеоп шеей (13-14% одчмешйеъ) дййъд чщешд бсйлеп вбед б-7% еб-14%, бдъаод, мсшип шйаеъ. дчщш бйп цшйлъ щеоп шеей мбйп сшип шйаеъ дйд беми бойезг бчшб отщрйн етбеш сшип шйаеъ одсевйн squamous cell е-small cell carcinoma. брйвег млк, цшйлд вбедд щм щеоп шб бмъй шеей дййъд чщешд бсйлеп роек б-8% мсшип шйаеъ.
баоцтеъ оегм сиийсий ошайн дзечшйн лй дзмфд щм 5% оск дчмешйеъ ощеоп шеей бщеоп шб бмъй шеей чщешд бсйлеп роек б16-17% мсшип шйаеъ осев squamous cell е-small cell carcinoma. ма роца чщш бйп щеоп зг бмъй шеей мбйп дсйлеп мсшип шйаеъ. дзечшйн ослойн лй мщйрей дшлб дщеоп бъжерд тщейд мдйеъ ъшеод мдфзъъ дсйлеп мсшип шйаеъ, бойезг бчшб отщрйн.
https://www.ncbi.nlm.nih.gov/pubmed/28742456
бозчш течбд (2021) обесс аелмесййд, рбгч дчщш бйп цшйлъ бйцйн елемсишем мбйп дсйлеп мъоеъд, лемм овешойн чшгйеесчемшййн. бозчш рлмме дръерйн щм 521,120 ощъъфйн бвймай 50-71 оосфш ажешйн башд"б. бодмк ъчефъ отчб зцйерйъ щм 16 щрд ъетге 129,328 очшй ъоеъд, одн 38,747 овешойн чшгйеесчемшййн. цшйлъ дбйцйн дзцйерйъ ртд бйп 0 м-28.7 вшн м-2,000 чмешйеъ мйен, бчшб дощъъфйн тн дцшйлд дроелд едвбедд бйеъш. цшйлъ длемсишем дзцйерйъ ртд бйп 118.3 м-330 о"в м-2,000 чмешйеъ мйен бчшб дощъъфйн тн дцшйлд дроелд едвбедд бйеъш.
роцае чщшйн зйебййн бйп цшйлъ бйцйн ецшйлъ лемсишем мбйп дсйлеп мъоеъд олм вешн, овешойн чшгйеесчемшййн еосшип. баефп сфцйфй, цшйлд щм зцй бйцд ресфъ мйен дййъд чщешд бсйлеп вбед б-7% мъоеъд, елм тмййд щм 300 вшн/йен бцшйлъ длемсишем дййъд чщешд бсйлеп вбед б-19% мъоеъд олм вешн, б-16% мъоеъд овешойн чшгйеесчемшййн еб-24% мъоеъд осшип. баоцтеъ рйъез сиийсий дзечшйн отшйлйн лй лемсишем дсбйш 63.2%, 62.3% е-49.6% одсйлеп мъоеъд олм вешн, овешойн чшгйеесчемшййн еосшип, бдъаод, дчщеш бцшйлъ бйцйн. цшйлд щм змбеп дбйцд бмбг ае ъзмйфй бйцйн дййъд чщешд бсйлеп оефзъ мъоеъд олм вешн, ощбх, осшип, оозмеъ рщйод еоамцдййош. дзмфд щм зцй бйцд блоеъ геод щм змбеп бйцд ае ъзмйфй бйцд, теу, гвйн, оецшй змб ае авежйн ечирйеъ дййъд чщешд бсйлеп роек йеъш мъоеъд олм вешн, овешойн чшгйеесчемшййн, осшип еоозмеъ рщйод.
йзг тн жаъ, дзечшйн оцййрйн лй дтгейеъ дчййоеъ мвбй дчщш бйп цшйлъ бйцйн еъзмеад чшгйеесчемшйъ еъоеъд айрп зг ощотйеъ, лащш йщрп бтйеъ оъегемевйеъ щереъ бдтшлъ чщшйн аме. сйбд азъ афщшйъ мооцайн дма тчбййн бозчшйн чегойн дйрд дчщш щроца богйреъ отшбйеъ бйп цшйлъ бйцйн вбедд мбйп дшвмйн ма бшйайн лвеп тйщеп, зесш фтймеъ вефрйъ еъжерд ма бшйад. жаъ бресу млк щцшйлд вбедд щм лемсишем мшеб омеед вн бцшйлд вбедд щм щеоп шеей ещм змбеп одзй.
дзечшйн ослойн лй бозчш жд роца лй цшйлд вбедд щм лемсишем ещм бйцйн дййъд чщешд бсйлеп оевбш мъоеъд олм вешн, овешойн чшгйеесчемшййн еосшип. дн оцйтйн лй двбмъ цшйлъ длемсишем едзмфъ бйцйн бзмбеп бйцйн бмбг ае бочешеъ азшйн мзмбеп тщейд мъшен мбшйаеъ дчшгйеесчемшйъ емдашлъ ъезмъ дзййн.
дозчш ръок тм йгй ълрйъ озчш маеойъ бсйп едзечшйн огеезйн тм дтгш рйвегй айришсйн.
https://pubmed.ncbi.nlm.nih.gov/33561122/
зжшд мъ
зймъ дозчшйн
цшйлъ шлйбйн сфцйфййн - аеЙовд 3 божеп
бдъбсс тм ръерйн ощрй озчшй течбд вгемйн (йемй 2016), зечшйн бзре аъ дчщш бйп цшйлъ зеоцеъ щеоп осев аеовд 3 щочешп бгвйн мбйп щйтеш дъоеъд бчшб 1,659 ощъъфйн тн сшип чемешчимй.
роца лй цшйлд вбедд йеъш щм аеовд 3 мазш абзеп дозмд дййъд чщешд бсйлеп роек йеъш мъоеъд осшип чемешчимй, лащш амд щцшле мфзеъ 0.3 вшн мйен аеовд 3 дйе бсйлеп роек бл-40% мъоеъд, бдщееад моиефмйн щцшле тг 0.1 вшн мйен аеовд 3. бресу, земйн ащш мазш дабзрд дтме аъ цшйлъ даеовд 3 бмфзеъ 0.15 вшн мйен дйе бтмй сйлеп роек бл-70% мъоеъд бдщееад мземйн щма щйре аъ цшйлъ аеовд 3. ма роца чщш бйп цшйлъ аеовд 3 мазш дабзрд мбйп дсйлеп мъоеъд олм вешн.
дзечшйн ослойн лй дтмаъ дцшйлд щм аеовд 3 бземйн тн сшип чемешчимй тщейд мщфш аъ сйлейй ддйщшгеъ щмдн.
http://www.ncbi.nlm.nih.gov/pubmed/27436272
озчш (ошх 2015) дбезп аъ ддшлб длйой еаъ ддщфтд дарий-сширйъ еревгъ-дзоцеп щм щешщ зжшъ о-3 шоеъ айлеъ, бдъан мдвгшеъ ощшг дзчмаеъ даошйчай.
http://www.ncbi.nlm.nih.gov/pubmed/25684599
бозчш отбгд (гцобш 2016) огвйойн дзечшйн лй цшйлъ авежйн овбйшд аъ дфтймеъ ревгъ зоцеп дибтйъ щм двеу еблк осййтъ морйтъ дъфъзеъ ъайн сширййн ботй.
https://www.ncbi.nlm.nih.gov/pubmed/27996158
бозчш отбгд (йемй 2016) огвйойн дзечшйн аъ дфтймеъ ревгъ дсшип щм ойцей авежй омк ешлйбйе дфтймйн лрвг ъай сшип дотй баоцтеъ дщфтд тм дфтймеъ щм ъай вжт сширййн ботй.
https://www.ncbi.nlm.nih.gov/pubmed/27455311
бозчш ъцфйъй фшесфчийбй (фбшеаш 2018), щртшк бчшб земй сшип дотй двс, детшк дчщш бйп цшйлъ авежйн мбйп щйтешй дйщреъ дсшип едъоеъд блмм еосшип бфши. бозчш рлмме дръерйн щм 826 земй сшип дотй двс - щмб 3 - ащш оймае щамерй ъжерд бжоп ийфемй длйоеъшфйд. мазш ъчефъ отчб зцйерйъ щм 6.5 щрйн, роца лй бчшб оиефмйн щцшле мфзеъ 2 ореъ бщбет щм авежйн олм сев, сйлейй дйщшгеъ мма озмд дйе вбедйн йеъш б-42% есйлейй ддйщшгеъ баефп лммй дйе вбедйн б-57% бдщееад моиефмйн щма цшле лмм авежйн. ддщфтд дойийбд роцад тбеш авежйн, ак ма тбеш беирйн. чщшйн амд рщоше вн мазш дъаод сиийсийъ мвешой дсйлеп дйгетйн мдйщреъ дсшип емъоеъд.
https://www.ncbi.nlm.nih.gov/pubmed/29489429
зжшд мъзймъ дозчшйн
цшйлъ шлйбйн сфцйфййн - фДйиеасишеврйн
счйшд щйиъйъ еоид-армйжд (2019) дтшйлд аъ дчщш бйп цшйлъ айжефмберйн щм сейд ецшйлъ змбеп сейд мбйп ъоеъд лммйъ, ъоеъд осшип баефп лммй, ъоеъд осевй сшип сфцйфййн еъоеъд оозмеъ мб лмй гн. дозчшйн щрлмме бсчйшд ртшле тм обевшйн (вйм>18). цшйлъ оецшй сейд ае сейд зещбд тм йгй сйлен цшйлън щм ожереъ сейд щерйн, лемм иефе, ойсе, иофд, фемй сейд, рбий сейд, фемй сейд оеъссйн, рбий амфмфд, йевеши сейд, вмйгъ сейд, чоз сейд, вбйръ сейд, рчрйчйеъ сейд, шеиб сейд, раие, змб сейд, аечшд, иефе йбщ еиефе оиевп. цшйлъ ожереъ сейд сфцйфййн лммд: раие, иефе еойсе. оъек 23 дозчшйн щрлмме бсчйшд, щрййн ртшле башцеъ дбшйъ, 19 богйреъ асйд, 1 башцеъ дбшйъ, 1 бчргд е-1 баесишмйд; лое лп, 12 озчшйн бгче аъ щрй дойрйн ещаш дозчшйн ртшле шч тм рщйн. мдмп сйлен дооцайн бдчщш щм ъоеъд олм сйбд:
- ма роца чщш оебдч бйп цшйлъ сейд леммъ мъоеъд олм дсйбеъ.
- цшйлд вбедд йеъш щм айжефмберйн щм сейд дййъд чщешд мсйлеп роек йеъш щм 10% мъоеъд олм сйбд (p=0.02).
- озчш азг дгвйн чщш дфек бйп цшйлъ змбеп сейд мбйп ъоеъд олм сйбд.
мдмп сйлен дооцайн бдчщш щм ъоеъд осшип:
- йщре чщш дфек бйп цшйлъ сейд еоецшйд мбйп ъоеъд осшип (p=0.03), ак чщш лжд ма рцфд бдчщш щм ожереъ сфцйфййн щм сейд лое раие,иефе еойсе (p=0.90).
- бозчшйн щртшле басйд, брйъез щм ъъ-чбецеъ, дегвн чщш дфек бйп цшйлъ сейд еоецшйд мбйп ъоеъд осшип ацм рщйн.
- ощъъфйн бчивешйд дтмйерд щм цшйлъ айжефмберйн щм сейд дйе бсйлеп роек б 20% мъоеъд осшип бдщееад мамд бъзъйъ дчивешйд (p=0.008).
- тмййд щм 10 о"в мйен бцшйлъ айжефмберйн щм сейд рчщшд бсйлеп роек б-7% мъоеъд осшип (p=0.003).
мдмп сйлен дооцайн бдчщш щм ъоеъд осев сшип сфцйфй:
- йщре чщш дфек бйп цшйлъ сейд мбйп ъоеъд осшип чйбд (p<0.001), сшип шйаеъ (p<0.001) елп сшип чемешчимй (p=0.003).
- роца чщш дфек бйп цшйлъ айжефмберйн щм сейд мъоеъд осшип дщг (p=0.04).
- тмййд щм 10 о"в мйен бцшйлъ айжефмберйн щм сейд чщешд бсйлеп роек йеъш щм 9% моееъ осшип дщг (p=0.02).
- цшйлд вбедд йеъш щм змбеп сейд дййъд чщешд бсйлеп роек йеъш бъоеъд осшип дщг (p=0.02).
- тмййд щм 5 вшн мйен бцшйлъ змбеп сейд чщешд мсйлеп роек йеъш щм 12% мъоеъд осшип дщг (p<0.001).
- мдмп сйлен дооцайн бдчщш щм ъоеъд оозмеъ мб елмй гн:
- айп чщш оебдч бйп цшйлъ айжефмберйн щм сейд мбйп ъоеъд оозмеъ мб елмй гн (p=0.61).
- айп чщш оебдч бйп цшйлъ змбеп сейд мбйп очшй оееъ лъецад оозмеъ мб елмй гн.
осчръ дзечшйн дйа щйщ мдвгйм аъ цшйлъ дсейд моишъ ашйлеъ йойн, ак йщ мрчеи ждйшеъ бревт мфшщреъ дооцайн бревт мойрерйн.
https://www.ncbi.nlm.nih.gov/pubmed/31278047
озчш течбд (ошх 2016) бе рбгч дчщш бйп дчфгд тм ъжерд тщйшд бфйиеасишеврйн мбйп дсйлеп мсшип чемешчимй, бдъбсс тм ооцайн чегойн дошайн лй цшйлъ фйиеасишеврйн чщешд бсйлеп оефзъ мсшип дтшоерйъ едщг. дзечшйн бгче аъ дръерйн щм л-48,000 рщйн бщбгйд бвймай 30-49. бъчефъ отчб щм л-19 щрд аебзре 206 очшй сшип чемешчимй, аемн ма роца чщш бйп ъжерд тщйшд бфйиеасишеврйн (лвеп мйвррйн еайжефмбереайгйн) мбйп дсйлеп мсшип чемешчимй.
тн жаъ, дзечшйн оцййрйн лй огебш босфш чип йзсйъ щм очшйн ейщ мдощйк ембзеп аъ ддщфтд щм фйиеасишеврйн бозчшйн ресфйн.
http://www.ncbi.nlm.nih.gov/pubmed/27010988
счйшд дойетгъ мбзеп одй ддщфтд дбшйаеъйъ щм фйиеасишеврйн, дрчщшйн мчемирй дасишевп евешойн мдщфтд арий-асишеврйъ.
одсчйшд темд лй мфйиеасишеврйн овееп дщфтеъ ойийбеъ, лемм дфзъъ ъсойрй вйм дотбш (лвеп вмй зен), дфзъъ дсйлеп маесиаефешежйс, дфзъъ дсйлеп мъзмеад чшгйеесчемшйъ, мщореъ, мъсоеръ доибемйъ, мселшъ сев 2 емдфштеъ бъфчег доез елп дфзъъ дсйлеп мсевй сшип щерйн, лемм сшип дщг, сшип дтшоерйъ есшип дотй. тн жаъ, бозчшйн ббтмй зййн, роца чщш мбтйеъ фешйеъ (айп ажлеш бсчйшд аегеъ дщфтд щмймйъ же бозчшйн тм брй агн).
тег оцййрйн дзечшйн лй зщйфд масишевп баефп лммй чщешд бсйлеп вбед мфъз сшип щзмеъ брщйн есшип тшоерйъ еащлйн бвбшйн етм бсйс ооцайн амд дн ослойн лй ддщфтеъ дойийбеъ щм фйиеасишеврйн ма бдлшз темеъ щм ддщфтеъ дщмймйеъ едръерйн дчййойн айрн осфйчйн тм оръ мбцт рйъез тмеъ оем ъетмъ, емлп ма рйъп мчбет осчрд зг-ощотйъ мвбй ддщфтд дойийбд щм фйиеасишеврйн.
дтшъ дотшлъ: зщеб мдбгйм бйп зщйфд масишевп баефп лммй мбйп зщйфд мфйиеасишеврйн елп бйп зщйфд мфйиеасишеврйн божеп лгевоъ сейд ае фщъп мбйп фйиеасишеврйн обеггйн бъесфй ъжерд. мдшзбъ дчшйад бреща фйиеасишеврйн есшип мзце лап: http://www.naturopedia.com/article.asp?rId=880
https://www.ncbi.nlm.nih.gov/pubmed/27723080
бозчш, щртшк бчшб земгеъ (фбшеаш 2017), роца лй цшйлъ в'рйсиайп, шлйб тйчшй бсейд, бодмк лм дзййн (бгеод мъжерд дасййъйъ) овбйшд аъ йтймеъ дийфем дарий-сширй биоечсйфп, бдщееад мцшйлъ в'рйсиайп шч мазш дъфъзеъ двйгем.
https://www.ncbi.nlm.nih.gov/pubmed/28148690
бозчш течбд (ребобш 2017) рбгч дчщш бйп цшйлъ фйиеасишеврйн мбйп дсйлеп мсшип дтшоерйъ бчшб вбшйн. дзечшйн оцййрйн лй йщрп тгейеъ фшд-чмйрйеъ млк щцшйлъ фйиеасишеврйн тмемд мдщфйт тм дсйлеп мсшип бщм добрд дгеод масишевп.
бозчш рлмме дръерйн щм л-27,000 вбшйн, щдщъъфе бозчш обечш дтесч бъшеод щм бгйчеъ счш мсшип. бъчефъ отчб зцйерйъ щм 11.5 щрйн, аебзре 2,598 очшйн щм сшип дтшоерйъ, одн 287 боцб оъчгн.
роца лй ощъъфйн тн дцшйлд двбедд бйеъш щм фйиеасишеврйн мтеоъ дроелд бйеъш, дйе бсйлеп вбед йеъш мдъфъзеъ сшип тшоерйъ оъчгн; сйлеп вбед б-91% тбеш цшйлъ айжефмберйн, б-51% тбеш цшйлъ в'рйсиайп, б-80% тбеш цшйлъ гайгжайп еб-67% тбеш цшйлъ вмйсиайп. чщшйн амд дйе оевбмйн мсшип тшоерйъ оъчгн бмбг.
дтшъ отшлъ: зщеб мцййп лй тогъ авегъ дсшип даошйчайъ дйа щцшйлъ ожереъ сейд осешъййн лое иефе, тщейд мдешйг аъ дсйлеп мзмеъ бсшип дтшоерйъ.
https://www.ncbi.nlm.nih.gov/pubmed/29114854
бсчйшд щйиъйъ еоид-армйжд (йреаш 2018) тглрйъ рбгч дчщш бйп цшйлъ сейд мбйп дсйлеп мсшип дтшоерйъ. бсчйшд рлмме 30 озчшйн ъцфйъййн, бдн л-270,000 ощъъфйн - оъелн л-21,000 очшй сшип тшоерйъ. бозчшйн дщерйн детшлд цшйлъ дсейд бъжерд ае шоъ дайжефмберйн бгн.
брйъез лемм щм дръерйн роца лй цшйлд вбедд йеъш щм сейд баефп лммй ещм врйсиайп, гайгжайп еоецшй сейд ма оеъссйн дййъд чщешд бсйлеп роек йеъш мсшип дтшоерйъ, тн сйлеп роек бл-30%, 10%, 16% е-35%, бдъаод. ма роца чщш бйп цшйлъ оецшй сейд оеъссйн, ск дцшйлд щм айжефмберйн ешоъ дайжефмберйн бгн мбйп дсйлеп мсшип дтшоерйъ. дзечшйн ослойн лй баефп лммй цшйлд вбедд йеъш щм оецшй сейд чщешд бсйлеп роек йеъш мсшип дтшоерйъ, аемн ргшщйн озчшйн ресфйн тм оръ мдтшйк аъ дъшеод щм цшйлъ сейд морйтъ сшип дтшоерйъ.
https://www.ncbi.nlm.nih.gov/pubmed/29300347
бозчш зък (афшйм 2018) детшлд дъшеод щм ъжерд тщйшд бсейд ебйшчеъ оцмйбйн мдфзъъ ъсойрйн лъецад одийфем бчшб рщйн дозмйоеъ осшип дщг.
бозчш рлмме 192 рщйн ооеца сйрй е-173 рщйн мбреъ оашд"б (чмйфешрйд), щдзмйое осшип щг бщмб 0 тг 3, ащш аебзп бйп дщрйн 2006-2012.
дощъъфеъ оймае щамерй ъжерд едщйбе мщамеп имферй бревт мъсойрйн дщерйн дчщешйн бийфем (рйъез, лйоеъшфйд, дчшреъ еийфем ъшефъй), лемм ъсойрй вйм дотбш (вмй зен, джтеъ мймд, йебщ бршъйч едфшщеъ одршъйч), бтйеъ офшчйн, тййфеъ, рщйшъ щйтш ебтйеъ жйлшеп.
баефп лммй иеез дцшйлд щм сейд ещм йшчеъ оцмйбйн рт бйп 0 мбйп 431 е-865 вшн/йен, бдъаод, едйд вбед йеъш бчшб рщйн ооеца сйрй. цшйлд вбедд йеъш щм сейд дййъд чщешд бсйлеп роек йеъш мъсойрй вйм дотбш етййфеъ, лащш бдщееад мрщйн щма цшле сейд, цшйлд щм отм 24 вшн/йен дййъд чщешд бсйлеп роек б-49% еб-57%, бдъаод.тн жаъ, брйъез мфй щййлеъ аърйъ, чщш жд роца оебдч шч тбеш рщйн мбреъ ема тбеш рщйн ооеца сйрй.
бдъййзс мцшйлъ йшчеъ оцмйбйн, роца лй бдщееад мцшйлд роелд (тг 33 вшн/йен) цшйлд вбедд (отм 70 вшн/йен) дййъд чщешд бсйлеп роек б-50% мсбем оъсойрй вйм дотбш бчшб лмм дрщйн. дзечшйн ослойн лй бчшб рщйн дозмйоеъ осшип щг, цшйлд вбедд йеъш щм оецшй сейд ещм йшчеъ оцмйбйн дййъд чщешд бшод роелд йеъш щм ъсойрй вйм дотбш етййфеъ лъецад одийфем дарий-сширй. https://www.ncbi.nlm.nih.gov/pubmed/29230660
зжшд мъзймъ дозчшйн
дщСфтъ гйаиеъ щереъ
ъжерд йн ъДйлерйъ | цДозереъ еиДбтереъ | ъжерд тъйшъ щеоп
дщСфтъ гйаиеъ щереъ - ъжерд йн ъДйлерДйъ
боид-армйжд (2025) детшк дчщш бйп гйаид йн-ъйлерйъ мбйп дсйлеп мсшип щг. дрйъез лмм 31 озчшйн, одн 12 озчшй течбд тн ъчефъ отчб щм 8 тг 33 щрд, е-19 озчшй очшд-бйчешъ. дрйъез бецт бщмещ чивешйеъ: лмм дрщйн, рщйн мфрй вйм дотбш, ерщйн мазш вйм дотбш.
бчшб лмм дрщйн, роца лй дъаод вбедд мгйаид дйн-ъйлерйъ дййъд чщешд бйшйгд щм 13% бсйлеп мсшип дщг. бчшб рщйн мфрй вйм дотбш ма роца чщш оебдч, бтег щбчшб рщйн мазш вйм дотбш геМез тм йшйгд щм 12% бсйлеп. ббзйрд мфй ажешйн ваевшфййн, дчщш дйд оебдч бозчшйн щбецте басйд, щн роца сйлеп роек б-41%. байшефд роцад йшйгд щм 10% бсйлеп, еайме башд"б роцад йшйгд щм 8% щайрд оебдчъ сиийсийъ. тег роца лй дчщш бйп дгйаид дйн-ъйлерйъ мбйп сйлеп оефзъ мсшип щг дйд оебдч шч бозчшй очшд-бйчешъ, ема ба мйгй бйией баефп оебдч бозчшй течбд. дзечшйн ослойн лй дчфгд тм гфес ъжерд йн-ъйлерйъ тщейд мъшен мдфзъъ дсйлеп мсшип щг, бтйчш бчшб рщйн мазш вйм дотбш ебажешйн осейойн, бойезг басйд. тн жаъ, ргшщйн озчшйн ресфйн мцешк айщещ дооцайн ембзйръ ддбгмйн бйп севй отшлй дозчш едажешйн дваевшфййн дщерйн.
https://pubmed.ncbi.nlm.nih.gov/40256142/
бозчш течбд (2025) рбзп дчщш бйп дгйаид дйн-ъйлерйъ мбйп дсйлеп мдъфъзеъ сшип дчщеш бщореъ.
тм фй дселреъ дбйп-маеойъ мзчш дсшип (IARC), чййн чщш оебдч бйп тегу ощчм мбйп сйлеп оевбш мдъфъзеъ озмеъ сшип о-13 севйн, лемм сшип шйшйъ дшзн, деещи, длмйд, дмбмб, длбг едщг, мцг азшйн. дзечшйн оцййрйн лй гйаид йн-ъйлерйъ роцад чщешд бщлйзеъ роелд йеъш щм озмеъ сшип еойъеп тмййд бощчм, емлп тщейд мъшен мдфзъъ дсйлеп мдъфъзеъ севй сшип дчщешйн бщореъ. дозчш дъбсс тм ръерйн оозчш течбд вгем щртшк байшефд (EPIC) бе рлмме обевшйн бвйм 35 тг 70 о-10 огйреъ. босвшъ дозчш детшлд дцшйлд дъжеръйъ щм дощъъфйн баоцтеъ щамерйн доеъаойн млм огйрд, лащш дъаод мгйаид йн-ъйлерйъ детшлд тм семн щм 9 есеевд м-3 чивешйеъ: роелд (0-3 рчегеъ), бйрерйъ (4-6 рчегеъ), евбедд (7-9 рчегеъ). дрйъез дрелзй лмм л-450 аму ощъъфйн брй 51 бооецт. бодмк ъчефъ отчб зцйерйъ щм л-15 щрд щйтеш дощъъфйн щзме бсевй сшип дчщешйн бщореъ дйд л-5%. роца лй дсйлеп дйд роек б-6% бчшб дощъъфйн бчбецъ ддъаод двбедд мгйаид дйн-ъйлерйъ бдщееад мдъаод роелд, лащш довод дййъд геод вн тбеш ощъъфйн бчбецъ ддъаод дбйрерйъ бйзс мроелд.
тн жаъ, дчщш бйп ойгъ ддъаод мгйаид дйн-ъйлерйъ мбйп дсйлеп мсшип ма дйд ъмей боггйн щм щореъ, лемм йзс оеърййн мйшлййн е-BMI.
дзечшйн ослойн лй дчфгд тм гйаид йн-ъйлерйъ дййъд омеед бйшйгд чмд бсйлеп мсевй сшип дчщешйн бщореъ, баефп бмъй ъмей боггйн щм щореъ. дн огвйщйн лй ргшщйн озчшйн ресфйн тм оръ мбзеп аъ орврерй дфтемд бдн гйаид йн-ъйлерйъ ъешоъ морйтъ сшип.
https://pubmed.ncbi.nlm.nih.gov/39998833/
бозчш течбд ебоид-армйжд щм озчшй течбд (ошх 2017) чегойн рбгч дчщш бйп дчфгд тм гйаид йн-ъйлерйъ мбйп дсйлеп мсшип дщг мазш вйм дотбш.
бозчш дтечбд рлмме дръерйн щм л-62,000 рщйн одемрг бвймай 55-69, ащш гйеезе бщръ 1986 тм дшвмй далймд еаешз дзййн щмдп ебецт азшйдп отчб бощк л-20 щрд. млм ощъъфъ зещб цйеп дъаод мгйаид дйн-ъйлерйъ.
тм бсйс дръерйн щм 2,321 одощъъфеъ щаебзре тн сшип дщг ечбецъ дщееад щм 1,665 рщйн бшйаеъ, роца лй рщйн тн цйеп дъаод вбед йеъш мгйаид дйн-ъйлерйъ дйе бсйлеп роек йеъш щм тг 40% мсшип щг щмймй мчемирй асишевп (ER-). дчщш мсшип дщг баефп лммй ае мсшип щг зйебй мчемирй асишевп (ER+) ма дйд оебдч сиийсийъ.
бресу, дзечшйн тшле оид-армйжд щм ъецаеъ дозчш дрелзй йзг тн озчшй течбд чегойн. роца лй дъаод вбедд мгйаид дйн ъйлерйъ, мтеоъ дъаод роелд, дййъд чщешд бсйлеп роек б-6% мсшип дщг баефп лммй, б-2% мсшип щг зйебй мчемирй асишевп, б-27% мсшип щг щмймй мчемирй асишевп еб-23% мсшип щг щмймй мчемирй асишевп ае фшевсишеп. дзечшйн оцййрйн лй бшеб дочшйн мсшип щг дщмймй мчемирйн дешоермййн фшеврежд фзеъ иебд емлп дчфгд тм гйаид йн-ъйлерйъ тщейд мдееъ асишивййъ орйтд зщебд.
https://www.ncbi.nlm.nih.gov/pubmed/28260236
счйшд щйиъйъ еоид-армйжд (йемй 2016) ащш ретгд мдтшйк аъ ддщфтд дбшйаеъйъ щм гйаид йн-ъйлерйъ щайррд оевбмъ бщеоп.
бсчйшд рлмме шч озчшйн обечшйн, длеммйн мфзеъ 100 ощъъфйн, азшйдн бецт отчб щм щрд мфзеъ егеез тм ръерй ъоеъд, ъзмеад чшгйеесчемшйъ, йъш мзх гн еселшъ елп тм ойгъ ддйтреъ мгйаид. бресу рлмме бсчйшд озчшй течбд дбезрйн аъ дчщш бйп гйаид йн-ъйлерйъ есшип.
бщрй озчшйн обечшйн ма роца дбгм бщйтешй дъоеъд олм вешн бйп дгйаиеъ щрбгче. бозчш азг вгем роца лй гйаид йн-ъйлерйъ дййъд чщешд бсйлеп роек йеъш майшетйн чшгйеесчемшййн, сшип дщг еселшъ (сйлеп роек б-29%, 57% е-30%, бдъаод).
брйъез лемм щм озчшй течбд роца лй дйтреъ вбедд мгйаид йн-ъйлерйъ дййъд чщешд бсйлеп роек бл-14% мъоеъд осшип (13 озчшйн) елп мъзмеад бсшип баефп лммй (4%, 3 озчшйн) есшип чемешчимй (9%, 9 озчшйн).
бдъййзс мдщфтд чшгйеесчемшйъ, обйп щмещд озчшйн, бозчш азг роца лй гйаид йн ъйлерйъ дййъд чщешд бсйлеп роек йеъш мдйщреъ щм аеин щшйш дмб емъоеъд. дооцайн мвбй ддщфтд щм гйаид йн ъйлерйъ тм йъш мзх гн, ъфчег чеврйийбй, озмъ лмйеъ, гмчъ офшчйн щвшерйъ еайлеъ дзййн дйе ма тчбййн, ойрйомййн ае ма оебдчйн сиийсийъ.
дзечшйн ослойн лй одтгейеъ доевбмеъ дчййоеъ, гйаид йн ъйлерйъ щайррд оевбмъ бцшйлъ дщеоп тщейд мдфзйъ аъ дсйлеп дчшгйеесчемшй, мсшип дщг емселшъ сев 2 ак ллм дршад айрд офзйъд аъ дсйлеп мъоеъд олм вешн.
http://www.ncbi.nlm.nih.gov/pubmed/27428849
счйшд (сфиобш 2015) дослоъ аъ дтгейеъ мвбй дчщш бйп ъжерд йн-ъйлерйъ мбйп дсйлеп мсшип лфй щтемд оозчшйн чмйрййн, озчшй течбд фшесфчийбййн еозчшй очшд-бчшд. бресу, грйн дзечшйн бдвгшеъ дщереъ щм ъжерд йн-ъйлерйъ боишд мдтшйк аъ йтймеъп.
озчшйн ъцфйъййн тглрййн ъеолйн блк щдчфгд вбедд тм ъжерд йн ъйлерйъ чщешд бсйлеп роек йеъш мъоеъд осшип елп мсйлеп роек йеъш мсевйн осейойн щм сшип, бйрйдн сшип чемешчимй, щг, чйбд, тшоерйъ, лбг ешащ ецееаш.
бдощк оцйвйн дзечшйн аъ дтгейеъ бйзс мчбецеъ дожеп дсфцйфйеъ бъжерд дйн ъйлерйъ, лемм фйшеъ ейшчеъ, гвйн, гврйн омайн, щоп жйъ, амледем еййп аген, бщш еоецшй змб.
дн ослойн лй ллм дршад ддщфтд дойийбд щм дъжерд дйн-ъйлерйъ айрд чщешд бшлйб ъжеръй осейн ама гееча бгфес дъжерд длемм. мошеъ довбмеъ доъегемевйеъ, лйен йщрд ъойлд шзбд мъфчйг щм ъжерд йн-ъйлерйъ бдврд офрй ъзмеад еъоеъд ебдфзъъ дсйлеп мсшип.
http://www.ncbi.nlm.nih.gov/pubmed/27014505
лзмч оозчш обечш вгем шб-ошлжй еобесс аелмесййд (аевеси 2017), щртшк бсфшг, бозчш дрелзй рбгч дчщш бйп гфес дъжерд мбйп дсйлеп мсшип тшоерйъ, мфй ойгъ давшсйбйеъ еддъфщиеъ щм дсшип. босвшъ дозчш ртщд щйоещ бръерйн аръшефеоишййн, афйгойемевййн еъжеръййн, щрасфе о-754 земй сшип дтшоерйъ еочбецъ бйчешъ щм 1,277 ощъъфйн бшйайн - бвймай 38-85. боаош чегн, дзечшйн гйеезе лй рйъп мсеев аъ гфесй дъжерд щм дощъъфйн мщмещ чбецеъ: ъжерд йн-ъйлерйъ, ъжерд щчемд (prudent) еъжерд отшбйъ.
роца лй бдщееад мдъаод роелд, дъаод вбедд мъжерд йн-ъйлерйъ - дтщйшд бфйшеъ ейшчеъ, гвйн, чирйеъ ещоп жйъ - дййъд чщешд бсйлеп роек б-34% мвйгем авшсйбй (цйеп вмйсеп вбед о-6) емсйлеп роек б-51% мщмб чмйрй оъчгн (cT2b-T4). ма роцае чщшйн оебдчйн тбеш гфесйн щм ъжерд щчемд ещм ъжерд отшбйъ. дзечшйн ослойн лй ддрзйеъ дъжеръйеъ морйтъ сшип дтшоерйъ цшйлеъ млмем дъййзсеъ мгфес дъжерд длемм тм фрй шлйбй ожеп осейойн, щлп роцае дбгмйн ощотеъййн бшоъ дсйлеп бйп гфесй дъжерд дщерйн.
https://www.ncbi.nlm.nih.gov/pubmed/28842246
бозчш течбд фшесфчийбй, (2019) щртшк бцшфъ, рбгч дчщш бйп дгйаид дйн-ъйлерйъ мбйп дсйлеп мсшип дтеш. бозчш рлмме дръерйн щм 67,332 рщйн бвймай 45-60 бъзймъ дозчш бщръ 1990. бдъан мщамерй ъжерд щоймае дощъъфеъ бщръ 1993, дзечшйн зйщбе тбеш лм ощъъфъ аъ ойгъ ддъаод мгйаид дйн-ъйлерйъ. бъчефъ дотчб бйп дщрйн 1993-2008 аебзре 2,003 очшйн щм сшип дтеш, одн 404 очшйн щм омреод, 1,367 очшйн щм чшцйреод щм ъайн бжамййн, е-232 очшйн щм чшцйреод щм ъай чщчщ.
роца лй цйеп дъаод вбед йеъш мгйаид дйн-ъйлерйъ дйд чщеш бсйлеп роек йеъш мсшип дтеш, лащш дощъъфеъ тн дцйерйн двбедйн бйеъш дйе бсйлеп роек б-17% бдщееад мощъъфеъ тн дцйерйн дроелйн бйеъш. бресу, роца чщш щмймй емйрйашй бйп цйеп дгйаид мбйп омреод (сйлеп роек б-28%) ечшцйреод щм ъайн бжамййн (сйлеп роек б-23%), ак ма роца чщш оебдч мсйлеп мчшцйреод щм ъай чщчщ.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм лк щгйаид йн-ъйлерйъ чщешд бсйлеп оефзъ мдъфъзеъ сшип дтеш, етщейд мдйеъ мооцайн амд дщмлд ййщеойъ зщебд борйтъ сшип дтеш.
https://pubmed.ncbi.nlm.nih.gov/31380561
зжшд мъзймъ дозчшйн
дщСфтъ гйаиеъ щереъ - цДозереъ еиДбтереъ
бсчйшд очйфд щм счйшеъ щйиъйеъ еоид-армйжеъ, длеммеъ озчшйн ъцфйъййн едътшбеъййн (2020) детшле дтгейеъ бдъййзс мчщш бйп гйаиеъ цозерйеъ осевйн щерйн мбйп ъецаеъ бшйаеъйеъ. брйъез рлмме 20 счйшеъ щйиъйеъ еоид-армйжеъ, бдп рбгче 34 ъецаеъ бшйаеъйеъ, ащш сееве мщбт чивешйеъ: фшефйм дщеорйн, ейиойп B12 едеоецйсиайп, ойршмйн, щореъ, гмчъйеъ еселшъ, сйлеп чшгйеесчемшй, сшип, еъоеъд олм вешн.
мдмп дооцайн дтйчшййн:
-
бдщееад мгйаид аеорйбешйъ, гйаиеъ цозерйеъ дйе чщешеъ бшод роелд йеъш щм лемсишем лммй, LDL е-HDL.
-
бдщееад мгйаид аеорйбешйъ, гйаиеъ цозерйеъ дйе чщешеъ бсйлеп оефзъ мъецаеъ бшйаеъйеъ щмймйеъ, лемм селшъ, озмъ мб лмймйъ, есшип.
-
овод же дйрд ощотеъйъ бойезг бгйаид агеерийсийъ, ащш леммъ оецшй змб ебйцйн, мма гвйн емма амледем етйщеп.
-
бдщееад мгйаид аеорйбешйъ, гйаиеъ цозерйеъ дйе чщешеъ бшйлежйн роелйн йеъш щм ейиойп B12 ебшйлежйн вбедйн йеъш щм деоецйсиайп, елп бшод роелд йеъш щм абх ебшжм ещм цфйфеъ дтцн.
дзечшйн ослойн лй гйаиеъ цозерйеъ чщешеъ бщйфеш фшефйм дщеорйн ебдфзъъ дсйлеп мъецаеъ бшйаеъйеъ щмймйеъ, ак вн бъецаеъ щмймйеъ бгвщ тм шйлеж роек щм ейиойп B12. йщ мбзеп баефп сфцйфй аъ ддщфтд щм гйаиеъ цозерйеъ бдшйеп ебдрчд еаъ ддщфтд щм зсшйн бойршмйн тм дсйлеп мсшип.
https://pubmed.ncbi.nlm.nih.gov/32204974/
бозчш течбд (2024) щртшк башд"б рбгч дчщш бйп гфес ъжерд добесс тм дцеоз ебйп дсйлеп мъоеъд бчшб аелмесййд овееръ обзйрд аърйъ.
дозчш ртшк бйп дщрйн 1993-2019 елмм 144,729 ощъъфйн ооеца мбп, афшйчай, йфрй, мийрй ае ймйгй дееай. бдъан мдтшлд ъжеръйъ щбецтд бъзймъ ъчефъ дотчб, млм ощъъу зещбе щмещд цйерйн: цйеп лммй щм ъжерд одцеоз (PDI), цйеп щм ъжерд бшйад одцеоз (hPDI) ецйеп щм ъжерд ма бшйад одцеоз (uPDI). бодмк ъчефъ отчб ооецтъ щм 21 щрд ъетге 65,087 очшй ъоеъд, лемм 18,663 очшй ъоеъд овешойн чшгйеесчемшййн е-16,171 очшй ъоеъд осшип. мдмп дооцайн дтйчшййн бдщееад бйп дцйерйн двбедйн бйеъш блм огг мтеоъ дроелйн бйеъш:
- цйерйн вбедйн щм ъжерд одцеоз ещм ъжерд бшйад одцеоз дйе чщешйн бсйлеп роек б-11-15% мъоеъд олм вешн вн бчшб вбшйн евн бчшб рщйн.
- цйеп вбед щм ъжерд ма бшйад одцеоз дйд чщеш бсйлеп вбед б-11% мъоеъд олм вешн бчшб рщйн бмбг, еовод геод роцад бдъййзс мъоеъд овешойн чшгйеесчемшййн вн бчшб рщйн евн бчшб вбшйн.
- цйеп вбед щм ъжерд одцеоз дйд чщеш бсйлеп роек б-14% мъоеъд осшип бчшб вбшйн.
- дчщш бйп ъжерд ма бшйад одцеоз ебйп дсйлеп мъоеъд дйд ощотеъй йеъш бчшб вбшйн мбрйн ероек йеъш бчшб рщйн ооеца мийрй.
дзечшйн ослойн лй гфес щм ъжерд одцеоз байлеъ вбедд роца чщеш бсйлеп оефзъ мъоеъд вн бчшб вбшйн евн бчшб рщйн, лащш йщрн дбгмйн бтецоъ дчщш бйп чбецеъ аърйеъ щереъ башд"б.
https://pubmed.ncbi.nlm.nih.gov/38703511/
бозчш течбд (2023) щртшк ббшйирйд рбгч дчщш бйп айлеъ дъжерд одцеоз ебйп дсйлеп мъоеъд емъзмеад лшерйъ. бозчш рлмме 126,394 ощъъфйн одбйе-брч дбшйий щвейсе мозчш бйп дщрйн 2006-2010 тн отчб тг щръ 2021. бдъбсс тм ръерй дцшйлд дъжеръйъ бъзймъ ъчефъ дотчб, млм ощъъу зещб цйеп щм ъжерд бшйад одцеоз (hPDI) ещм ъжерд ма бшйад одцеоз (uPDI). дзечшйн зйщбе аъ дчщш бйп оггйн амд ебйп дсйлеп мъоеъд, мъзмеад чшгйеесчемшйъ, мдъфъзеъ сшип емщбшйн. роца лй ощъъфйн тн дцйерйн двбедйн бйеъш щм ъжерд бшйад одцеоз дйе бсйлеп роек йеъш мъоеъд, мсшип емъзмеад чшгйеесчемшйъ, тн сйлеп роек б-16%, б-7% еб-8%, бдъаод, бдщееад мощъъфйн тн дцйерйн дроелйн бйеъш. бресу, роца сйлеп роек б-14% еб-16% маеин щшйш дмб емщбх айслой, бдъаод. брйвег млк, ощъъфйн тн цйерйн вбедйн щм ъжерд ма бшйад одцеоз дйе бсйлеп оевбш мъоеъд, мъзмеад чшгйеесчемшйъ емсшип. дъецаеъ дйе геоеъ брйъез мфй овгш, тйщеп, BMI, шод сецйе-ачереойъ есйлеп врий. дзечшйн ослойн лй бчшб обевшйн бвйм дбйрййн, дчфгд тм гфес щм ъжерд одцеоз байлеъ вбедд ецоцен дцшйлд щм ожереъ одзй тщейд мъшен мщойшд тм бшйаеъ иебд баефп бмъй ъмей бвешой сйлеп йгетйн мъзмеад лшерйъ ае мсйлеп врий.
https://pubmed.ncbi.nlm.nih.gov/36976560/
озчш течбд вгем бе рлмме л-26,000 вбшйн (ребобш 2015) оцбйт тм лк щъжерд ибтерйъ омеед бсйлеп роек бл-35% мсшип дтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/26561618
бозчш течбд вгем щртшк бдемрг (ошх 2016), рбгч дчщш бйп цозереъ ецшйлд оетид щм бщш мбйп сшип шйаеъ, щг етшоерйъ. огвн дозчш лмм л-11,000 ощъъфйн бвймай 55-69 бъзймъ дозчш (бщръ 1986), ащш сееве м-5 чбецеъ бдъан мойгъ цшйлъ дбщш (цозерййн, аелмй гвйн, аелмй бщш фтн бщбет, аелмй бщш 2-5 фтойн бщбет, аелмй бщш 6-7 фтойн бщбет).
мазш ъчефъ отчб щм л-20 щрд жеде 279 очшйн щм сшип шйаеъ, 312 очшй сшип дщг е-399 очшй сшип дтшоерйъ. мазш дъаод сиийсийъ мовееп ощърйн, ма роца чщш бйп цшйлъ бщш мбйп дсйлеп мщмещъ севй дсшип.
лое лп, роца лй бчшб ощъъфйн щцшле бщш йен азг бщбет дсйлеп мсшип тшоерйъ оъчгн дйд вбед бл-75% бдщееад мощъъфйн щцшле бщш огй йен. дзечшйн ослойн лй цшйлд оетид щм бщш айрд ъешоъ мдфзъъ дсйлеп мдъфъзеъ щм сшип шйаеъ, щг етшоерйъ.
дтшъ дотшлъ: дзечшйн ма мчзе бзщбеп аъ дщфМтъ цшйлъ оецшй дзмб, ащш чщешйн мдъфъзеъ вйгемйн дешоермййн лвеп сшип щг ае сшип тшоерйъ.
йъшд оже, ма йдйд оефшк мдрйз щбчшб цозерйн ащш айрн аелмйн бщш ак айрн ибтерйн чййоъ цшйлд вбедд одооецт щм оецшй змб, ръеп ащш тщей мдщфйт йщйшеъ тм ъецаеъ дозчш емдзмйщ аъ досчрд мвбй дчщш бйп цшйлъ дбщш мдъфъзеъ сширйн щерйн.
http://www.ncbi.nlm.nih.gov/pubmed/26931668
бозчш, щртшк бчшб зжйшйн (2017), рбгче дорврерйн бдн ъжерд тъйшъ чмешйеъ оебймд мдъфъзеъ ъдмйлйн гмчъййн есширййн ботй. дзечшйн ошайн лй ъзъ ърайн щм ъжерд тъйшъ чмешйеъ змд тмййд боъеек дгмчъй IL-6 бшйшйъ дотй бдщееад мчбецъ бйчешъ щцшлд гйаид сиргшийъ.
дзечшйн осбйшйн лй чййойн ийфемйн ъшефъййн лрвг IL-6 мийфем бсшип дотй, аемн ийфемйн амд йчшйн елшелйн бъефтеъ мееай, емлп тщей мдйеъ йъшеп мвйщд ъжеръйъ арий-гмчъйъ морйтъ гмчъ лшерйъ есшип отй. дн ошайн лй десфъ ъфезй агод свемйн, дтщйшйн баръецйарйрйн, мъжерд ъшод мйшйгд ощотеъйъ бшоъ IL-6 ебосмемй дъчщешъ дъайъ дчщешйн амйе, бдщееад мчбецъ бйчешъ, щчйбмд ъжерд тъйшъ чмешйеъ мма ъфезй дагод.
ооца жд огвйн лйцг цшйлъ ожереъ цозййн омайн, долймйн шлйбйн арий-гмчъййн, тщеййн мъшен морйтъ сшип дотй елп осфч ъойлд мозчшйн чегойн, дошайн лй щлйзеъ сшип дотй роелд йеъш бъшбейеъ бдп дъжерд обессъ тм ожереъ одцеоз бдщееад мъшбейеъ бдп йщрд цшйлд вбедд щм ожереъ одзй.
https://www.ncbi.nlm.nih.gov/pubmed/28193578
бозчш очшд бчшд (сфиобш-аечиебш 2017), щдъчййн биайееап ебе ртшлд дщееад бйп дъжерд щм 233 рщйн тн сшип дщг ечбецъ бйчешъ длеммъ 236 рщйн, роца лй ъжерд доаефййръ бцшйлд вбедд щм бщш ещм бщш отебг дййъд чщешд бсйлеп вбед йеъш мсшип дщг еайме ъжерд добессъ тм дцеоз дййъд чщешд бсйлеп роек йеъш.
бозчш очшд-бчшд азш щдъчййн бсйп ебе рлмме 818 рщйн тн сшип дщг ечбецъ бйчешъ щм 935 рщйн, роца лй гфес щм "ъжерд сйрйъ осешъйъ" (щлмм бтйчш бщш, йшчеъ/фйшеъ, аешж, чоз зйид, ъйшс ебйцйн) дйд чщеш бсйлеп роек йеъш мсшип дщг. лое лп, гфес щм "ъжерд оъечд" (щаефййп бовееп ожереъ ае ощчаеъ оъечйн, лвеп ощчаеъ чмйн етевеъ) дйд чщеш бсйлеп роек йеъш. ма роца чщш бйп гфес щм "ъжерд цозерйъ" (щлмм бтйчш ожереъ оп дцеоз лвеп сейд, фйшеъ егврйн омайн ефзеъ бщш еожеп оиевп) егфес щм "ъжерд омезд" (щлмм ожереъ тъйшй омз, лемм шеиб сейд, оересегйен вмеиеоаи еле') - мбйп дсйлеп мсшип дщг. дн осбйшйн щбгфес щм ъжерд оъечд рлмме тег шлйбй ожеп щаемй дщфйте тм дъецаеъ, ебгфес дцозерй шеб дъжерд дсйрйъ дйа обещмъ (мтеоъ йшчеъ ишййн) емлп ййълп ема роцад дщфтд ойийбд лоцефд.
дозчш оеоп тм йгй чшп озчш дсшип дтемойъ ертшк тм йгй зечшйн одошлж мбчшд еорйтъ озмеъ бсйп.
https://www.ncbi.nlm.nih.gov/pubmed/29017525
https://www.ncbi.nlm.nih.gov/pubmed/28898273
зжшд мъзймъ дозчшйн
дщСфтъ гйаиеъ щереъ - ъжерд тъйшъ щеоп
озчш фшд-чмйрй (гцобш 2015), длемм щйоещ боегм щм зйеъ отбгд егвйоеъ ъайн, бе рбгчд ддщфтд щм ъжерд тъйшъ-щеоп гмъ-фзойоеъ тм вйгем оезй авшсйбй осев вмйебмсиеод.
дзечшйн осбйшйн лй ооцайн чегойн оцбйтйн тм дйтймеъ щм дйортеъ овмечеж баоцтеъ гйаид чиеврйъ озойшд, аемн гйаид же чщд мййщен етмемд мвшен мъефтеъ мееай.
млп, бозчш жд рбгчд ддщфтд щм гйаид тъйшъ-щеоп егмъ-фзойоеъ щдйрд озойшд фзеъ ак геод бдщфМтъд доибемйъ едарий-сширйъ, йзг тн щойшд тм дгшйщеъ дъжеръйеъ.
одъецаеъ темд лй гфес гйаид жд дйд бтм дщфтд арий-сширйъ ощотеъйъ еъшн мтйлеб змечъ дъайн дсширййн емтмййд бощк ддйщшгеъ.
http://www.ncbi.nlm.nih.gov/pubmed/26631612
бозчш течбд бе рлмме 177 рщйн (оай 2016) роца лй цшйлд вбедд йеъш щм щеоп шеей ероелд йеъш щм щеоп бмъй шеей бвйм 10-18 чщешд бцфйфеъ вбедд йеъш щм шчоъ дщг бвйм 25-29.
дтшъ отшлъ: шчоъ щг цфефд тмемд мдтмеъ сйлеп мсшип щг.
http://www.ncbi.nlm.nih.gov/pubmed/27197283
брйъез лемм щм озчшй течбд фшесфчийбййн (йемй 2017) рбгч дчщш бйп севйн щерйн щм щеоп бъжерд мбйп дсйлеп мсшип шйаеъ. дзечшйн осбйшйн лй мъжерд тъйшъ щеоп ъфчйг бдъфъзеъ ъдмйлйн сширййн бшйаеъ, аемн дооцайн оозчшйн афйгойемевййн айрн тчбййн.
бозчш дрелзй рлмме дръерйн отщшд озчшйн, бдн лоймйеп езцй ощъъфйн ел-18,000 очшйн щм сшип шйаеъ - бъчефъ отчб ооецтъ щм 9.4 щрйн. роца лй бдщееад мощъъфйн тн дцшйлд дроелд бйеъш, цшйлд вбедд щм щеоп баефп лммй (38% одчмешйеъ) ещм щеоп шеей (13-14% одчмешйеъ) дййъд чщешд бсйлеп вбед б-7% еб-14%, бдъаод, мсшип шйаеъ. дчщш бйп цшйлъ щеоп шеей мбйп сшип шйаеъ дйд беми бойезг бчшб отщрйн етбеш сшип шйаеъ одсевйн squamous cell е-small cell carcinoma. брйвег млк, цшйлд вбедд щм щеоп шб бмъй шеей дййъд чщешд бсйлеп роек б-8% мсшип шйаеъ.
баоцтеъ оегм сиийсий ошайн дзечшйн лй дзмфд щм 5% оск дчмешйеъ ощеоп шеей бщеоп шб бмъй шеей чщешд бсйлеп роек б16-17% мсшип шйаеъ осев squamous cell е-small cell carcinoma. ма роца чщш бйп щеоп зг бмъй шеей мбйп дсйлеп мсшип шйаеъ. дзечшйн ослойн лй мщйрей дшлб дщеоп бъжерд тщейд мдйеъ ъшеод мдфзъъ дсйлеп мсшип шйаеъ, бойезг бчшб отщрйн.
https://www.ncbi.nlm.nih.gov/pubmed/28742456
зжшд мъзймъ дозчшйн
дщСфтъ гйаиеъ щереъ - ъжерд гмчъйъ
бсчйшд еоид-армйжд (ошх 2018) щм озчшйн афйгойемевййн рбгч дчщш бйп ъжерд гмчъйъ мбйп дсйлеп мдъфъзеъ сшип.
бсчйшд рлмме 44 озчшйн байлеъ вбедд, бдн мотмд оомйеп (1,082,092) ощъъфйн, лащш гфес дъжерд щм дощъъфйн бозчшйн дщерйн детшк баоцтеъ догг мъжерд гмчъйъ (dietary inflammatory index-DII). огг жд ощощ мдтшлъ дфеирцйам дгмчъй щм гфес дъжерд длемм, бдъбсс тм дцшйлд щм 45 ожереъ ешлйбйн сфцйфййн (лгевоъ ейиойрйн, ойршмйн, фйиелйойчмйн, сйбйн ъжеръййн, зеоцеъ щеоп зйерйеъ, ревгй зйоцеп етег), мфйе ллм щдцйеп вбед йеъш лк дъжерд йеъш фше-гмчъйъ еллм щдцйеп роек йеъш лк дъжерд йеъш арий-гмчъйъ.
орйъез лмм дръерйн темд лй ощъъфйн тн дцйерйн двбедйн бйеъш дйе бсйлеп вбед б-58% мсшип, бдщееад мощъъфйн тн дцйерйн дроелйн бйеъш. дсйлеп дйд ъмей ойреп, лк щлм тмййд щм рчегд богг DII дйд чщеш бтмййд щм 8.3% бсйлеп мсшип.
овод же роцад тбеш сшип чемешчимй, щг, еещи, тшоерйъ, лмйеъ ещзмеъ, еайме дооцайн тбеш сшип шйаеъ дйе оевбмйн. дзечшйн ослойн лй ъжерд гмчъйъ чщешд бсйлеп оевбш мсшип, аемн ргшщйн озчшйн фшесфчийбййн тм оръ мащщ аъ дооцайн бдъййзс мчбецеъ аелмесййд щереъ есевй сшип щерйн.
https://www.ncbi.nlm.nih.gov/pubmed/29566194
зжшд мъзймъ дозчшйн
фтймеъ вефрйъ
боид-армйжд ощръ 2024 рбзрд дйтймеъ щм айоерй веу-рфщ ефтймеъ вефрйъ мдчмд тм ъсойрй гйлаеп бчшб обевшйн земй сшип. дсчйшд лммд 10 озчшйн ачшаййн обечшйн бдн дщъъфе 620 земй сшип осевйн ебщмбйн щерйн, ащш гйеезе тм ъсойрй гйлаеп. оъек лмм дозчшйн, б-4 рбзрд ддщфтд щм айоерй веу-рфщ, лащш б-3 озчшйн ртшлд дътшбеъ добессъ тм йевд ебозчш азг ц'й-черв ае иай-ц'й. б-6 озчшйн азшйн рбгчд ддщфтд щм фтймеъ вефрйъ осевйн щерйн, лвеп айоерй айшебй ае оъйзеъ. чбецеъ дбйчешъ чйбме ийфем сиргший, дгшлд ае щма чйбме лм дътшбеъ.
брйъез лемм щм дръерйн роца лй дътшбейеъ щлмме фтймеъ вефрйъ ае айоерй веу-рфщ ъшое мщйфеш оебдч бъсойрй гйлаеп бдщееад мчбецеъ дбйчешъ. брйъез ресу тм фй сев ддътшбеъ, роца лй шч фтймеъ вефрйъ дебймд мщйфеш оебдч, бтег щма роцад дщфтд ощотеъйъ майоерй веу-рфщ. тн жаъ, ма роца йъшеп оебдч мфтймеъ вефрйъ бдщееад еийфем сиргший бмбг. дзечшйн ослойн лй фтймеъ вефрйъ тщейд мъшен мдчмд бъсойрй гйлаеп бчшб обевшйн земй сшип, лащш ма роцад ъойлд оебдчъ мъетмъ щм айоерй веу-рфщ, лвеп йевд. йзг тн жаъ, бщм овбмеъ дозчшйн дчййойн йщ цешк бозчш ресу лгй мбсс аъ дооцайн.
https://pubmed.ncbi.nlm.nih.gov/38836958/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2021) детшлд дъшеод щм айоеп вефрй бйъй бтцйоеъ роелд тг бйрерйъ мщйфеш ъсойрй тййфеъ, гйлаеп езшгд бчшб озмйойн осшип. бсчйшд рлмме 11 озчшйн бдн 1,066 ощъъфйн, 77% одн тн дйсиешйд щм сшип щг, 14% сшип щзмеъ, 4% сшип чемешчимй, 4% сшип тшоерйъ е-1% севй сшип азшйн.
обйп дозчшйн, бъщтд рбгчд ддщфтд тм шоъ дтййфеъ ебщрййн рбгчд ддщфтд тм шоъ дгйлаеп едзшгд. брйъез лемм щм дръерйн, айоеп вефрй бйъй роца йтйм мщйфеш ъсойрй тййфеъ вн бсйен ъчефъ ддътшбеъ евн мазш ъчефъ отчб щм щмещд тг ъщтд зегщйн. тег роца лй дътшбейеъ щлмме ййтех бъгйшеъ вбедд дйе омееъ бщйфеш вгем йеъш бъсойрй тййфеъ бдщееад мдътшбейеъ щма лмме ййтех ае щлмме ййтех бъгйшеъ роелд.
дзечшйн ослойн лй айоеп вефрй бйъй тщей мдчм тм тййфеъ бчшб озмйойн осшип, тн дщфтд ооещлъ маешк ъщтд зегщйн мфзеъ ейъшеп мчбмъ ййтех бъгйшеъ вбедд.
https://pubmed.ncbi.nlm.nih.gov/34649267/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2021) детшлд ддщфтд щм фтймеъ вефрйъ, щм гйаид догод цен (fast-mimicking diet – сев щм цен мсйшевйп), ещм дътшбеъ фсйлемевйъ тм щйтеш ддйщшгеъ бчшб земй сшип. бсчйшд рлмме 31 озчшйн, одн ъщтд бзре аъ ддщфтд щм фтймеъ вефрйъ е-22 озчшйн бзре аъ ддщфтд щм дътшбеъ фсйлемевйъ, лащш ма роцае озчшйн бдн рбгчд ддщфтд щм гйаид догод цен.
бозчшйн амд рлмме оиефмйн тн сшип дщг (12 озчшйн), сшип ботшлъ дтйлем (зойщд озчшйн), сшип шйаеъ (зойщд озчшйн), омреод (щрй озчшйн) есевйн азшйн (ъщтд озчшйн). баефп лммй роца лй ддътшбеъ ъшод мщйфеш бощк ддйщшгеъ бозчш азг обйп ъщтд щтсче бфтймеъ вефрйъ ебщоерд обйп 22 щтсче бдътшбеъ фсйлемевйъ. лое лп, дзечшйн бйцте оид-армйжд бд рлмме ъщтд озчшйн бдн детшлд дйтймеъ щм дътшбеъ фсйлемевйъ бчшб земеъ сшип дщг. брйъез жд роцад овод щм щйфеш ощк ддйщшгеъ, бтйчш бийфем ооещк щм щйщд зегщйн еотмд.
одсчйшд темд лй дътшбеъ ооещлъ йеъш дзм ощмбйн оечгойн йеъш щм дозмд роцад обийзд йеъш мщйфеш ощк ддйщшгеъ бчшб земй сшип, аемн ргшщйн озчшйн ресфйн мдтшлъ ддщфтд тм ощк ддйщшгеъ, бтйчш бчшб земй сшип щайре сшип дщг.
https://pubmed.ncbi.nlm.nih.gov/33359756/
бсчйшд щйиъйъ (2019) очйфд оецвеъ дтгейеъ дтглрйеъ бдъййзс мчщшйн бйп фтймеъ вефрйъ мбйп дсйлеп мдъфъзеъ сшип едсйлеп мъоеъд бчшб земй сшип. мдмп дооцайн дтйчшййн:
-
бдъбсс тм 45 гезеъ, бдн рлмме оаеъ озчшйн афйгойемевййн елод оймйерй ощъъфйн, роцае шайеъ зжчеъ млк щшод вбедд щм фтймеъ вефрйъ чщешд бсйлеп роек бл-10-20% мсевйн щерйн щм сшип, лемм щмфезйъ дщъп, щг, отй, шзн, еещи, лмйеъ ечйбд.
-
бдъбсс тм 18 счйшеъ щйиъйеъ еоид-армйжеъ, роцае шайеъ осейоеъ млк щшод вбедд щм фтймеъ вефрйъ чщешд бсйлеп роек бтг 40-50% мъоеъд олм вешн ае мъоеъд осшип бчшб земй сшип щг, сшип чемешчимй, ае сшип тшоерйъ.
-
ооцайн тглрййн озощ оид-армйжеъ ео-25 озчшйн ъеолйн бъецаеъ аме.
дзечшйн ослойн лй шод вбедд щм фтймеъ вефрйъ чщешд бсйлеп оефзъ мдъфъзеъ севйн щерйн щм сшип емщйфеш бщйтеш ддйщшгеъ бчшб змч одземйн. дзечшйн оцйтйн лй йщ мдощйк ембзеп чщшйн амд вн бдъййзс мсевй сшип фзеъ щлйзйн ебчбецеъ аелмесййд щереъ, елп мбзеп лйцг чщшйн амд оещфтйн ошоеъ щереъ щм фтймеъ вефрйъ еодн дорврерйн досбйшйн чщшйн амд.
https://pubmed.ncbi.nlm.nih.gov/31095082/
щмещд озчшйн (оай 2016) оцбйтйн тм дзщйбеъ щм бйцет фтймеъ вефрйъ чбетд мдфзъъ дсйлеп мсшип.
- бозчш течбд шзб дйчу, бе рлмме л-1.4 оймйеп ощъъфйн оашд"б еайшефд, рбгч дчщш бйп бйцет фтймеъ вефрйъ мбйп дсйлеп мосфш севйн рфецйн щм сшип. бъчефъ отчб щм 10-27 щрд жеде л-187,000 очшй сшип лащш шод вбедд, бдщееад мроелд, щм фтймеъ вефрйъ дййъд чщешд бсйлеп роек йеъш м-13 севй сшип: еещи, лбг, шйаеъ, лмйеъ, чйбд, шйшйъ дшзн, мечойд ойамеайгйъ, ойамеод, отй, шащ ецееаш, фй дибтъ, щмфезйъ дщъп ещг. тн жаъ, роца лй шод вбедд йеъш щм фтймеъ вефрйъ дййъд чщешд бсйлеп вбед йеъш момреод емсшип дтшоерйъ. бошбйъ дочшйн, дчщш дйд бмъй ъмей бойгъ ддщорд ае дтйщеп.
- бозчш ресу бе рлмме 9 озчшйн рбгч дчщш бйп фтймеъ вефрйъ мбйп дсйлеп мсшип дщзмеъ. дозчш обесс тм дръерйн щм 8,309 земеъ сшип дщзмеъ бдщееад мчбецъ бчшд щм 12,612 рщйн бшйаеъ. роца лй рщйн щма бйцте фтймеъ вефрйъ дйе бсйлеп вбед б-34% мсшип дщзмеъ бдщееад мрщйн щбйцте фтймеъ вефрйъ чбетд.
- бозчш очшд-бчшд ресу рбгч дчщш бйп бйцет фтймеъ вефрйъ мбйп дсйлеп мсшип цееаш дшзн. бозчш дщъъфе 128 земеъ сшип цееаш дшзн ечбецъ бчшд щм 512 рщйн бшйаеъ. роца лй бдщееад мрщйн бчбецъ дбчшд, рщйн тн сшип цееаш дшзн гйеезе фй 2.5 йеъш тм дйортеъ офтймеъ вефрйъ.
щмещъ дозчшйн оцбйтйн тм лк щрйъп мдлмйм лй бйцет фтймеъ вефрйъ чбетд тщей мдфзйъ аъ дсйлеп мсевйн щерйн щм сшип, мма ъмеъ боафййрйн сецйе-гоевшфййн ае бвешой аешз зййн лвеп дщорд ае тйщеп.
http://www.ncbi.nlm.nih.gov/pubmed/27183032
http://www.ncbi.nlm.nih.gov/pubmed/27197285
http://www.ncbi.nlm.nih.gov/pubmed/27105330
озчш (оай 2016) бе бецт рйъез ръерйн о-9 озчшйн боишд мбзеп аъ дчщш бйп дтгш фтймеъ вефрйъ мбйп дсйлеп мсшип щзмеъ. бозчш рлмме ръерйн щм 8,309 земеъ сшип дщзмеъ ечбецъ дщееад длеммъ 12,612 рщйн бшйаеъ.
роца лй рщйн щма бйцте фтймеъ вефрйъ щбетйъ чбетд дйе бсйлеп вбед бл-34% мзмеъ бсшип дщзмеъ.
дзечшйн ослойн лй ооцай дозчш осфчйн ъойлд ресфъ млк щдтгш фтймеъ вефрйъ одеед вешн сйлеп бмъй ъмей мсшип, лащш йщ мдощйк ембзеп одй шоъ дфтймеъ дйтймд мдфзъъ дсйлеп.
бозчш ресу (йерй 2016) щртшк тм йгй аеън дзечшйн бецт рйъез ръерйн о-12 озчшйн длеммйн 6,806 рщйн тн сшип щзмеъ вшешъй боишд мдтшйк дан дтгш фтймеъ вефрйъ мфрй дабзеп чщеш бсйлеп вбед йеъш мъоеъд бъчефъ отчб щм 5 щрйн.
роца лй рщйн щма бйцте фтймеъ вефрйъ щбетйъ чбетд дйе бсйлеп вбед бл-22-34% мъоеъд.
http://www.ncbi.nlm.nih.gov/pubmed/27197285
http://www.ncbi.nlm.nih.gov/pubmed/27299959
боид-армйжд (ошх 2017) рбгчд дйтймеъ щм ашбтъ дийфемйн дочебмйн бйеъш мдчмд тм ъщйщеъ бчшб земй сшип осевйн щерйн: фтймеъ вефрйъ, ийфем фсйлемевй, щймеб щм фтймеъ вефрйъ еийфем фсйлемевй ае ийфем ъшефъй. боид-дармйжд рлмме 113 озчшйн ачшаййн обечшйн, бдн 11,525 ощъъфйн, ащш фешсое бйп дщрйн 1999-2016.
роца лй фтймеъ вефрйъ, ийфем фсйлемевй ещймеб щм фтймеъ вефрйъ еийфем фсйлемевй дйе омеейн бщйфеш ъзещъ дъщйщеъ бодмк емазш дийфем дарий-сширй дтйчшй (p<0.001), ак ма ийфем ъшефъй. тег роца лй йтймеъ дийфем дййъд ъмейд босфш вешойн, бйрйдн щмб дозмд, цешъ дийфем дарий-сширй ешоъ дъщйщеъ. дзечшйн ослойн лй фтймеъ вефрйъ еийфем фсйлемевй йтймйн йеъш одийфем дъшефъй мдчмд тм ъщйщеъ бчшб земй сшип.
https://www.ncbi.nlm.nih.gov/pubmed/28253393
счйшд щйиъйъ (йерй 2016) щретгд мбзеп аъ дчщш бйп дчфгд тм ддрзйеъ морйтъ сшип, длеммеъ ъжерд рлерд ебйцет фтймеъ вефрйъ, мбйп щйтеш дъзмеад едъоеъд осшип.
бсчйшд рлмме 12 озчшйн бдн роца лй бдщееад мдчфгд роелд тм аешз зййн бшйа, дчфгд вбедд дййъд чщешд бсйлеп оефзъ щм 10-61% бщйтеш дъзмеад едъоеъд осшип баефп лммй.
баефп сфцйфй, роца сйлеп оефзъ щм 19-60% мъзмеад бсшип дщг, 23-60% мъзмеад бсшип дшзн е- 27-52% мъзмеад бсшип чемешчимй. дооцайн бревт мсшип шйаеъ ма дйе зг ощотййн ема роца чщш бйп щойшд тм аешз зййн бшйа мбйп сшип дщзмеъ ае дтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/27340121
счйшд доъашъ аъ дъшеод щм дшфеад дчешйарйъ досешъйъ мшфеад доегшрйъ, ебойезг мийфем бозмъ дсшип, лйееп щоцйтд ийфем шб ъзеой длемм щйреййн баешз дзййн, щйоещ бфешоемеъ цозй ошфа, гйчеш, оечсд, фтймеъ вефрйъ осешъйъ еогйицйд тм оръ мдзжйш аъ дайжеп бйп двеу, дрфщ едшез.
https://www.ncbi.nlm.nih.gov/pubmed/24282099
бозчш зък (2020) детшлд дбшйаеъ двефрйъ едрфщйъ, бдъан мшоъ дфтймеъ двефрйъ еощк дфтймеъ дйещбрйъ, бчшб обевшйн щдзмйое осшип бдщееад мобевшйн мма дйсиешйд щм сшип. оишъ дозчш дййъд мбзеп дан йеъш фтймеъ вефрйъ ефзеъ фтймеъ йещбрйъ, чщешд бщйфеш дбшйаеъ двефрйъ едрфщйъ бщрйн мазш дийфем ревг дсшип. лзмч оозчш течбд вгем, щртшк тм йгй айвег дсшип даошйчай, бозчш жд рлмме 3,718 озмйой сшип щрд тг зощ щрйн мазш дабзрд, 4,248 озмйой сшип щщ тг тщш щрйн мазш дабзрд, е-69,860 ощъъфйн мма дйсиешйд щм сшип.
дощъъфйн дъбчще мгеез тм ощк джоп дооецт бщбет бе тсче бщрд дчегоъ бфтймейеъ вефрйеъ, добецтеъ бтцйоеъ оъерд тг вбедд (MVPA), етм ощк дфтймеъ дйещбрйъ. шоъ дфтймеъ сеевд мзощ чивешйеъ бйп лмм ма м-22.5 еотмд MET щтеъ бщбет (MET = щеед тшк оибемй, щдйре айргчс щм ъцшелъ аршвийъ/чмешйъ), еощк дфтймеъ дйещбрйъ сеев мщмещ чивешйеъ бйп афс мщщ еотмд щтеъ бйен.
мдмп дооцайн дтйчшййн:
-
дцйерйн боггй дбшйаеъ двефрйъ едрфщйъ, дйе вбедйн баефп оебдч бчшб ощъъфйн мма дйсиешйд щм сшип, аемн ддбгмйн бйп дчбецеъ ма дйе ощотеъййн обзйрд чмйрйъ.
-
блм дчбецеъ, шод вбедд йеъш щм фтймеъ вефрйъ дййъд чщешд бцйерйн вбедйн йеъш щм бшйаеъ вефрйъ ерфщйъ.
-
блм дчбецеъ, ощк фтймеъ йещбрйъ роек йеъш дйд чщеш бцйерйн вбедйн йеъш щм бшйаеъ вефрйъ ерфщйъ.
дзечшйн ослойн, лй ооцайн амд осфчйн тгеъ мзщйбеъ щм дчфгд тм фтймеъ вефрйъ едфзъъ фтймеъ йещбрйъ мщйфеш дбшйаеъ двефрйъ ерфщйъ бобевшйн, тн ае мма дйсиешйд щм сшип, лащш ддомцд дйа 150-300 гчеъ бщбет щм фтймеъ бтцйоеъ оъерд ае 75-150 гчеъ бщбет щм фтймеъ бтцйоеъ вбедд.
https://pubmed.ncbi.nlm.nih.gov/33079415/
бге"з озчшй (2017), щфешсн тм йгй щрй вефй озчш вгемйн дтесчйн бзчш озмъ дсшип, оецвеъ дтгейеъ дтглрйеъ бревт мчщш бйп ъжерд, фтймеъ вефрйъ еоггйн аръшефеоишййн мбйп сшип дщг.
длеъбйн оцййрйн лй сшип дщг дйре дсшип дщлйз бйеъш бчшб рщйн, лащш б-2012 аебзре бшзбй дтемн 1.7 оймйеп очшйн згщйн, додеейн лшбт олмм очшй дсшип бчшб рщйн. осчреъ дгез обессеъ тм 119 озчшйн щртшле бшзбй дтемн длеммйн мотмд о-12 оймйеп рщйн ейеъш о-260,000 очшй сшип дщг.
дооцайн дтйчшййн бдъййзс мсшип дщг мфрй вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: дчфгд тм фтймеъ вефрйъ рошцъ, тегу ощчм ае щореъ бвйм цтйш (18-30) ебъчефъ дбвшеъ (тегу ощчм бъчефъ дймгеъ ебвйм ддъбвшеъ чщеш бцойзд айийъ йеъш ебшод роелд йеъш щм вешн вгймд елп вешн мдъоййреъ оечгоъ щм шчоъ дщг щреид фзеъ мъдмйлйн сширййн. бресу тегу ощчм чщеш бшоеъ роелеъ йеъш щм дешоерйн щзмъййн) едрчд; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: цшйлъ амледем евешойн дъфъзеъййн доебймйн мчеод вбедд емощчм мйгд вбед йеъш.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - ER negative), цшйлъ ожереъ долймйн чшеиреайгйн, цшйлъ оецшй змб, цшйлъ ъжерд тщйшд бсйгп ещойшд тм аешз зййн фтйм.
дооцайн дтйчшййн бдъййзс мсшип дщг мазш вйм дотбш:
йщрп тгейеъ обессеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: щойшд тм аешз зййн фтйм (лемм дчфгд тм фтймеъ вефрйъ рошцъ), дрчд етегу ощчм ае щореъ бвймай 18-30; ещдвешойн дбайн чщешйн бсйлеп вбед йеъш мсшип дщг: тегу ощчм ае щореъ бъчефъ дбвшеъ мфрй вйм дотбш, тмййд бощчм бъчефъ дбвшеъ, вешойн дъфъзеъййн доебймйн мчеод вбедд ецшйлъ амледем.
йщрп тгейеъ оевбмеъ млк щдвешойн дбайн чщешйн бсйлеп роек йеъш мсшип дщг: цшйлъ йшчеъ ма тоймрййн (бдъййзс мсшип щг щмймй мчемирй асишевп - (ER negative, цшйлъ ожереъ долймйн чшеиреайгйн ецшйлъ ъжерд тщйшд бсйгп.
дзечшйн оцййрйн лй ооцай дге"з айрн леммйн аъ двешойн дбайн щроцае чщешйн бсйлеп оевбш мдъфъзеъ сшип дщг:
- айшетй зййн дчщешйн бзщйфд вбедд йеъш масишевп ефшевсишеп лемм: дефтъ озжеш деесъ мфрй вйм 12, лрйсд мвйм дотбш мазш вйм 55, ай-дбаъ ймгйн мтемн едшйеп шащеп мазш вйм 30.
- зщйфд мчшйрд бодмк ийфемйн шфеаййн, бойезг бвйм ддъбвшеъ.
- ийфем дешоермй змйфй ещйоещ бвмемеъ морйтъ дшйеп.
ддомцеъ длммйеъ дтемеъ одге"з дйрп щойшд тм ощчм ъчйп, дчфгд тм аешз зййн фтйм, цшйлъ ъжерд бшйад едвбмъ цшйлъ амледем.
http://www.aicr.org/continuous-update-project/breast-cancer.html
рййш тогд (аевеси 2016) щфешсн тм йгй фарм оеозйн оитн дшщеъ дбйрмаеойъ мзчш дсшип (IARC) дтесч бчщш бйп дщорд едсйлеп мсшип. ддтшлд дйа лй бщръ 2013-2014, бшод двмебмйъ, 10.8% одвбшйн, 14.9% одрщйн е-5.0% одймгйн сбме одщоръ йъш (BMI>30).
доеозйн оцййрйн лй дщорд етмййд бощчм маешк дзййн ъмеййн бойгд шбд бвешойн дрйърйн мщмйид ещйрей, бйрйдн шоъ дцшйлд дчмешйъ ебйцет фтймеъ вефрйъ. доеозйн айщще аъ дооцайн дчегойн ощръ 2002, дошайн лй мщойшд тм ощчм ъчйп ъфчйг борйтъ зойщд севй сшип: отй, ещи, лмйеъ, щг (мазш вйм дотбш) ешзн.
брййш дтогд дрелзй, добесс тм мотмд о-1,000 озчшйн афйгойемевййн, оесйфйн доеозйн тег 8 севй сшип мшщйод же: чйбд, лбг, лйс ошд, мбмб, щзмеъ, бмеиъ дъшйс, оез (орйрвйеод) еойамеод рфецд. бресу, йщрп тгейеъ мвбй дчщш м-3 севй сшип ресфйн: тшоерйъ, щг (бвбшйн) емйофеод.
дн ослойн лй дтгш щеоп веу тегу офзйъ аъ дсйлеп мошбйъ севй дсшип. бресу, оозчшйн фшд-чмйрййн темд лй йшйгд олееръ бощчм тщейд мдйеъ бтмъ дщфтд овйрд офрй дъфъзеъ сшип аемн ргшщйн озчшйн чмйрййн ббрй агн тм оръ мащщ ооцайн амд.
http://www.ncbi.nlm.nih.gov/pubmed/27557308
бозчш очшд-бчшд шишесфчийбй (оай 2017) рбгч дчщш бйп аешз зййн фтйм мбйп дсйлеп мсшип щмфезйъ дщъп едлмйеъ.
бозчш рлмме 160 земй сшип лмйеъ, 208 земй сшип щмфезйъ дщъп ечбецъ бйчешъ щм 766 ощъъфйн мма сшип, лемн рбгче ае иефме бошлж ийфем бсшип башд"б (Roswell Park Cancer Institute) бйп дщрйн 1989-1998 едслйое мома щамеп афйгойемевй очйу. босвшъ дщамеп, дощъъфйн дъбчще мгеез аегеъ дойгд бд дн щеЙошйн тм аешз зййн фтйм, лащш ощъъфйн щгйеезе лй маешк дзййн дн обцтйн фтймеъ вефрйъ фзеъ офтн бщбет ае фзеъ о-4 фтойн бзегщ девгше л"ма фтймйн вефрйъ".
роца лй ощъъфйн щайрн фтймйн вефрйъ дйе бсйлеп вбед б-77% мсшип длмйеъ еб-73% мсшип щмфезйъ дщъп. чщшйн геойн роцае вн тбеш ощъъфйн щайрн себмйн ощореъ. дзечшйн ослойн лй ъецаеъ дозчш ъеолеъ бъфйсд мфйд аешз зййн йещбрй одеед вешн сйлеп бмъй ъмей мсшип, аемн ргшщйн озчшйн фшесфчийбййн бдйчу вгем йеъш тм оръ мащщ аъ дооцайн.
https://www.ncbi.nlm.nih.gov/pubmed/28528291
боаош (2019) оцйтйн дзечшйн лмйн едрзйеъ мшефайн лйцг мщмб фтймеъ вефрйъ лзмч оосвшъ дийфем даерчемевй дсиргший.
шащйъ, дзечшйн оцйвйн аъ дтгейеъ мфйдп фтймеъ вефрйъ чщешд бсйлеп оефзъ мдъфъзеъ сшип, бщйфеш ддйщшгеъ ебщйфеш ъецаеъ ресфеъ бчшб земй сшип лвеп айлеъ дзййн, зшгд, гйлаеп, тййфеъ етег. йзг тн жаъ, ошбйъ земй дсшип айрн обцтйн фтймеъ вефрйъ сгйшд. озчшйн ошайн щбочшйн шбйн дземйн лмм айрн очбмйн одцееъ доифм дрзйеъ мбйцет фтймеъ вефрйъ, лащш дзсойн млк леммйн дтгш оегтеъ мтшк щм фтймеъ вефрйъ бчшб земй сшип, зесш егаеъ мвбй дбийзеъ ае ддъаод щм фтймеъ вефрйъ моиефм, дтгш оегтеъ мълрйеъ фтймеъ вефрйъ дойетгеъ мземй сшип, цешк бдлщшд мцешк бйцет ддфрйд еаоерд лй дфрйд мфтймеъ вефрйъ айрд бъзен дийфем щм даерчемев.
босвшъ доаош дзечшйн оцйтйн лмйн дойетгйн мдчм тм даерчемев мдомйх моиефмйн ае мдфреън мълрйъ биезд, йтймд еоъайод, ъек дъййзсеъ мдтгфеъ ецшлй доиефм. тм дшефа мбцт ъдмйк длемм дтшлд щм оцб доиефм, домцд мдтмаъ шоъ дфтймеъ двефрйъ едфрйд мфтймеъ оъайод. йщ мзжеш тм ъдмйк жд бошеезй жоп чбетйн ошащ ае бдъан мцешк емщйреййн боцб дшфеай ае босвшъ дийфем. бсйен доаош дзечшйн грйн баъвшйн еоцйтйн одй дотешбеъ дргшщъ одвешойн дщерйн – цееъ шфеай, чебтй огйрйеъ, зечшйн, ътщййъ дбшйаеъ едлещш едоиефмйн - тм оръ млмем фтймеъ вефрйъ босвшъ дийфем даерчемевйъ дсиргшийъ.
https://pubmed.ncbi.nlm.nih.gov/31617590/
бозчш ъцфйъй (2020) детшк дфеирцйам щм фтймеъ вефрйъ мдфзъъ ддщфтд щм цшйлъ амледем тм дсйлеп мъоеъд осшип. бозчш рлмме дръерйн щм 54,686 ощъъфйн отм вйм 30, отщшд счшй бшйаеъ обессй аелмесййд, щртшле ббшйирйд. тм фй двгшд щошрйъ, севй дсшип дчщешйн бцшйлъ амледем леммйн змм дфд, вшеп, мет, ещи, лбг, чемешчимй, чйбд есшип дщг - лащш бдвгшд шзбд йеъш рлммйн вн сшип дмбмб ешйаеъ.
бдъан мцшйлъ дамледем, дощъъфйн сееве мщщ чивешйеъ цшйлъ амледем, дроггеъ бйзйгеъ амледем мщбет – лм йзйгд щеед мщоерд вшн амледем рчй:
-
ощъъфйн щлмм айрн цешлйн амледем.
-
ощъъфйн щрвоме оцшйлъ амледем.
-
ощъъфйн дцешлйн амледем баефп ачшай.
-
ощъъфйн дцешлйн амледем бдъан мдрзйеъ – тг 14 мрщйн етг 21 мвбшйн.
-
ощъъфйн дцешлйн лоеъ оселръ щм амледем – 14-35 мрщйн е-21-49 мвбшйн.
-
ощъъфйн дцешлйн лоеъ ожйчд щм амледем – отм 35 мрщйн еотм 49 мвбшйн.
фтймеъ вефрйъ сеевд бдъан мшу дъзъеп едтмйеп щм ддомцеъ – 7.5 MET щтеъ/щбет е-15 MET щтеъ/щбет (MET = щеед тшк оибемй, щдйре айргчс щм ъцшелъ аршвийъ/чмешйъ).
брйъез дръерйн роца чщш йщйш зжч бйп цшйлъ амледем едсйлеп мъоеъд осшип тм шчт цшйлъ амледем, лащш бчшб рвомйн дсйлеп дйд вбед б-46%, цшйлд оселръ дййъд чщешд бсйлеп вбед б-39% ецшйлд ожйчд дййъд чщешд бсйлеп вбед б-62%, бдщееад мощъъфйн щайрн цешлйн амледем. шоъ дсйлеп йшгд баефп рйлш бчбецеъ амд, бчшб ощъъфйн щбйцте фтймеъ вефрйъ отм м-7.5 MET щтеъ/щбет (дсйлеп дйд вбед б-25%, б-21% еб-52%, бдъаод).
дзечшйн ослойн лй йщ мтегг мбйцет фтймеъ вефрйъ ласишивйд мдфзъъ дсйлеп мъоеъд осшип тм шчт цшйлъ амледем вбедд.
https://pubmed.ncbi.nlm.nih.gov/32406936/
бозчш ъцфйъй (йемй 2017) рбгчд ддщфтд щм фтймеъ вефрйъ тм дъфчег дчеврйийбй бчшб рщйн щдзмйое осшип дщг, лащш дзечшйн ощтшйн лй щйфеш бъсойрйн лое ъщйщеъ йебйм мщйфеш бъфчег дчеврйийбй.
бозчш рлмме 299 рщйн бреъ 57 бооецт. ощк дфтймеъ дйеойъ бтцйоеъ бйрерйъ-вбедд рогг бощк 7 йойн бшцйфеъ баоцтеъ ог ъаецд (ачсмшеоиш), олщйш чип доецог мвеу доафщш огйгд аебййчийбйъ щм дфтймеъ двефрйъ. лое лп, лм дрщйн оймае щамерйн могйгъ дъщйщеъ едъфчег дчеврйийбй.
роца лй ллм щощк дфтймеъ дйд вбед йеъш лк дрщйн гйеезе тм шоъ ъщйщеъ роелд йеъш. бресу, шоъ ъщйщеъ роелд йеъш дййъд чщешд бщйфеш дъфчегйн дрйдемййн ежйлшеп дтбегд. ооцай дозчш ъеолйн бооцайн чегойн, дошайн лй фтймеъ вефрйъ ъешоъ мийфем бдйгшгшеъ чеврйийбйъ дчщешд бозмъ дсшип еоцбйтйн тм лк щддщфтд дойийбд чщешд бдфзъъ ъзещъ дъщйщеъ.
https://www.ncbi.nlm.nih.gov/pubmed/28677009
брйъез лемм щм озчшй течбд фшесфчийбййн (2019) рбгч дчщш бйп длоеъ едтцйоеъ щм фтймеъ вефрйъ мбйп дсйлеп мсшип. дзечшйн оцййрйн лй ддомцд мфтймеъ вефрйъ дйрд 7.5-15 MET (щеед тшк оибемй - айргчс щм ъцшелъ аршвийъ/чмешйъ) щтеъ бщбет. брйъез, бе рлмме дръерйн оъщтд озчшйн, рбгч дчщш бйп дфтймеъ двефрйъ мбйп дсйлеп м-15 севй сшип, ъек дщееад бйп ощъъфйн щлмм ма бйцте фтймеъ вефрйъ мбйп 7.5, 15, 22.5 ае 30 MET щтеъ бщбет. брйъез рлмме дръерйн щм 755,459 ощъъфйн, азшйдн ртшк отчб щм л-10 щрйн ебодмлп геез тм 50,620 очшйн щм сшип.
мдмп сйлен дооцайн:
- фтймеъ вефрйъ бдъан мдомцеъ дййъд чщешд бсйлеп роек мщбтд севй сшип, лемм сшип дотй (сйлеп роек б-8-14% бчшб вбшйн), щг (сйлеп роек б-6-10%), шзн (сйлеп роек б-10-18%), лмйеъ (сйлеп роек б-11-17%), ойамеод (сйлеп роек б-14-19%), лбг (сйлеп роек б-18-27%), емйофеод щайрд дегв'чйп (сйлеп роек б-11-18% бчшб рщйн).
- тбеш севй сшип осейойн дчщш бйп лоеъ дфтймеъ двефрйъ едйшйгд бсйлеп дйд мйрашй, лащш бсевйн азшйн роца чщш щайре мйрашй.
- дъецаеъ тбеш фтймеъ вефрйъ бтцйоеъ бйрерйъ евбедд ма дйе тчбйеъ.
- дчщш бйп фтймеъ вефрйъ мбйп дсйлеп мсшип дшзн дйд ъмей б-BMI, аемн тбеш щаш севй дсшип дъецаеъ дйе бмъй ъмейеъ б-BMI.
дзечшйн ослойн лй йщ мтегг обевшйн мбйцет фтймеъ вефрйъ бдъан мдомцеъ дчййоеъ боишд мдфзйъ аъ дсйлеп мсевйн щерйн щм сшип.
https://pubmed.ncbi.nlm.nih.gov/31877085/
бозчш течбд фшесфчийбй (2017) рбгч дчщш бйп дмйлд мбйп дсйлеп мъоеъд бчшб чщйщйн. дзечшйн осбйшйн лй чййоеъ тгейеъ обессеъ млк щфтймеъ вефрйъ щм мфзеъ 150 гчеъ мщбет бтцйоеъ бйрерйъ ае 75 гчеъ бтцйоеъ вбедд оеомцъ мщойшд тм дбшйаеъ, аемн дооцайн бревт мъшеод щм дмйлд бмбг дйрн оевбмйн.
бозчш рлмме л-140,000 ощъъфйн брй л-70 бооецт. бъчефъ отчб щм л-13 щрд, л-43,000 ощъъфйн рфише. роца лй бдщееад мдмйлд щм тг щтъййн бщбет (фзеъ одшод доеомцъ), дтгш фтймеъ вефрйъ дййъд чщешд бсйлеп вбед б-26% мъоеъд еайме дмйлд щм 2-6 фтойн бщбет (бдъан мшод доеомцъ) дййъд чщешд бсйлеп роек б-20% мъоеъд едмйлд щм отм 6 щтеъ бщбет дййъд чщешд бсйлеп роек б-22% мъоеъд. дмйлд дййъд чщешд бойгд дшбд бйеъш мсйлеп оефзъ мъоеъд лъецад оозмеъ рщйод, озмеъ чшгйеесчемшйеъ есшип.
дзечшйн ослойн лй бчшб чщйщйн, вн дмйлд фзеъ одшод доеомцъ тщейд мъшен мдфзъъ дсйлеп мъоеъд бдщееад мдтгш фтймеъ вефрйъ, лащш дмйлд бдъан ае отм мшод доеомцъ чщешд бйшйгд вгемд йеъш бшоъ дсйлеп.
http://www.ajpmonline.org/article/S0749-3797(17)30460-9/fulltext
бозчш ъцфйъй (афшйм 2018) детшк дчщш бйп щмещд оггй веу, ащш детшле баоцтеъ CT - осъ щшйш роелд, айлеъ щшйш роелд ешчоъ щеоп тегфъ - мбйп дсйлеп мъоеъд бчшб рщйн тн сшип щг щайре вшешъй.
бозчш рлмме 3,241 рщйн, ащш аебзре бйп дщрйн 2000-2013 тн сшип щг бщмб 2 ае 3. дзечшйн бзре аъ дчщш бйп оггй двеу мбйп ощк жоп ддйщшгеъ едсйлеп мъоеъд олм вешн маешк ъчефъ отчб зцйерйъ щм л-6 щрйн. обйп лмм дрщйн, 34% девгше лбтмъ осъ щшйш роелд (сшчефрйд) е-37% лбтмеъ айлеъ щшйш роелд (цфйфеъ щшйш роелд).
роца лй бчшб рщйн тн сшип щг щайре вшешъй, сшчефрйд дййъд чщешд бсйлеп вбед б-41% мъоеъд бдщееад мрщйн мма сшчефрйд. лое лп, дрщйн бтмеъ ск шчоъ дщеоп двбедд бйеъш (щмйщ тмйеп) дйе бсйлеп вбед б-35% мъоеъд бдщееад мрщйн тн ск шчоъ дщеоп дроелд бйеъш (щмйщ ъзъеп). бчшб рщйн тн сшчефрйд ешчоъ щеоп вбедд, дсйлеп мъоеъд дйд вбед б89%. ма роца чщш бйп огг айлеъ дщшйш мбйп дсйлеп мъоеъд. дзечшйн оцййрйн лй BMI бмбг ма дйд чщеш баефп оебдч мсйлеп мъоеъд ема ъшн мжйдей рщйн дроцаеъ бсйлеп оевбш мъоеъд. дзечшйн ослойн лй йщре абзеп зсш щм сшчефрйд бчшб земеъ сшип дщг, лащш моггй CT щм сшчефрйд ешчоъ щеоп тщей мдйеъ тшк фшевресий еблк мъшен мойчег дийфем елъецад олк мщйфеш щйтешй ддйщшгеъ.
https://www.ncbi.nlm.nih.gov/pubmed/29621380
брййш тогд тглрй,(оай 2018) щфешсн оитн дзбшд даесишмйъ маерчемевйд чмйрйъ (COSA), чебтйн цееъ доеозйн лй фтймеъ вефрйъ дйрд биезд ейтймд мийфем бдщфтеъ двефрйеъ едрфщйеъ дщмймйеъ, дчщешеъ бозмъ дсшип ебийфем бд.
дзечшйн ослойн аъ дтгейеъ дозчшйеъ бревт мъфчйг щм фтймеъ вефрйъ лзмч одийфем бозмъ дсшип еосфчйн дрзйеъ млм арщй дцееъ дшфеай мвбй щймеб дфтймеъ двефрйъ лзмч одийфем дсиргший.
мдмп ддомцеъ дтйчшйеъ:
- йщ мщмб фтймеъ вефрйъ лзмч одийфем дсиргший, лийфем ъеок дойетг мдфзъъ ддщфтеъ дщмймйеъ щм дозмд ещм дийфем.
- тм лм дцееъ дшфеай дшб-ъзеой мтегг мфтймеъ вефрйъ емдомйх моиефмйн мбцт фтймеъ бдъан мдрзйеъ; мфзеъ 150 гчеъ щм фтймеъ айшебйъ бтцйоеъ бйрерйъ е-2-3 айоерй дървгеъ бтцйоеъ вбедд - бщбет.
- фшеиечем дийфем (best practice) цшйк млмем дфрйд мшефа сфеши ае фйжйеъшфйси оеозд бийфем бсшип.
дзечшйн оцййрйн лй йщрп тгейеъ обессеъ млк щфтймеъ вефрйъ ъешоъ мщйфеш дъфчег двефрй, офзйъд тййфеъ лъецад одозмд еодийфем, очмд тм ъзещъ доцечд дфсйлемевйъ еощфшъ аъ айлеъ дзййн.
бресу, йщрп тгейеъ млк щбйцет фтймеъ вефрйъ мфрй, бодмк ае азшй дийфем ъешоъ мдфзъъ дзеошд щм ъефтеъ дмееай емдфзъъ дсйлеп мдъфъзеъ ооайшейеъ згщеъ. лое лп, ооцайн афйгойемевййн оцбйтйн тм лк щфтймеъ вефрйъ чщешд бсйлеп оефзъ мдйщреъ дозмд емъоеъд.
https://www.ncbi.nlm.nih.gov/pubmed/29719196
мдмп щрй оаошйн (йерй 2018)щфешсое мазшерд, догвйщйн аъ дъшеод щм фтймеъ вефрйъ мземйн емозмйойн осшип.
боаош дшащеп оецвъ счйшд щйиъйъ еоид-армйжд, дотшйлд аъ ддщфтд щм фтймеъ вефрйъ тм дтмййд бсйбемъ мб-шйад бчшб обевшйн тн сшип.
бсчйшд рлмме 48 озчшйн ачшаййн обечшйн, бдн 3,632 оиефмйн брй 55 бооецт, ащш земче ачшайъ мдщъъфеъ бълрйъ фтймеъ вефрйъ ае мчбецъ бйчешъ. роца лй фтймеъ вефрйъ дебймд мтмййд оебдчъ бсйбемъ мб-шйад, лащш бчбецъ дбйчешъ ма дйд лм щйрей.
ооца жд дйд бмъй ъмей боафййрй дфтймеъ двефрйъ. бдъййзс мдйбийн щм бийзеъ, б-30 одозчшйн ртшк отчб азш дщфтеъ щмймйеъ. сд"л геез тм 44 дщфтеъ щмймйеъ - шебп чмеъ лвеп сзшзешъ, лабйн бзжд елабй щшйшйн - ак геез вн тм дщфтеъ щмймйеъ зоешеъ, щлмме аеин щшйш дмб ещбш бйшк.
йзг тн жаъ, дзечшйн огеезйн лй щйтеш ддщъъфеъ еддйтреъ дйд вбед ешч 11% одощъъфйн фшще одозчш мфрй сеу ъчефъ дотчб. дзечшйн ослойн лй дщъъфеъ бълрйъ фтймеъ вефрйъ дйрд гшк йтймд мщйфеш дсйбемъ бчшб земй сшип.
боаош ресу оецв озчш течбд, бе рбгч дчщш бйп фтймеъ вефрйъ мбйп дсйлеп мъоеъд бчшб обевшйн тн дйсиешйд щм сшип бъчефъ дймгеъ.
бозчш рлмме 15,450 обевшйн оашд"б ечргд, щзме бсшип мфрй вйм 21 - бйп дщрйн 1970-1999 - еазшйдн ртшк отчб тг мщръ 2013. бвйм 26 бооецт дощъъфйн тре тм щамеп, бе дъбчще мгеез тм осфш щтеъ дфтймеъ двефрйъ бтцйоеъ вбедд щбйцте бщбет, боерзйн щм "щеед тшк оибемй" (metabolic equivalent task –MET - айргчс щм ъцшелъ аршвийъ/чмешйъ, мфй йзйгд азъ щм MET щеед м-3.5 оймймйиш зоцп мчймевшн ощчм веу мгчд, борезд. ллм щд- MET вбед йеъш, дгбш отйг тм оаох вефрй вбед/чщд йеъш).
бъчефъ отчб щм л-10 щрйн, 1,063 одощъъфйн рфише (811 лъецад ооцб бшйаеъй, 120 лъецад одйщреъ ае дъчгоеъ щм аеъе сшип е-132 овешойн азшйн ае ма йгетйн). орйъез дръерйн темд лй щйтешй дъоеъд олм вешн дйе 11.7% тбеш ощъъфйн щгйеезе тм MET щм 0 щтеъ бщбет, 8.6% тбеш 3-6 щтеъ бщбет, 7.4% тбеш 9-12 щтеъ бщбет е-8% тбеш 15-21 щтеъ бщбет. бресу, мазш дъаод сиийсийъ моцб бшйаеъй лшерй емзщйфд мийфемйн щерйн, роца чщш щмймй оебдч бйп фтймеъ вефрйъ мбйп ъоеъд.
орйъез дщйреййн бфтймеъ двефрйъ бъчефд щм 8 щрйн (бдъбсс тм дръерйн щм 5,689 одощъъфйн), роца лй тмййд ооецтъ щм 8 щтеъ MET бщбет дййъд чщешд бйшйгд щм 40% бсйлеп мъоеъд олм вешн бдщееад мощъъфйн щщоше тм фтймеъ вефрйъ роелд маешк лм дъчефд. дзечшйн ослойн лй дчфгд тм фтймеъ вефрйъ бтцйоеъ вбедд, ъек тмййд бщтеъ дфтймеъ тн дтмййд бвйм, дййъд чщешд бсйлеп оефзъ мъоеъд бчшб обевшйн тн дйсиешйд щм озмъ сшип бймгеъ.
https://www.ncbi.nlm.nih.gov/pubmed/29894274
https://www.ncbi.nlm.nih.gov/pubmed/29862412
бозчш,(2020) щртшк бчшб тлбшйн, огвйойн дзечшйн лй мфтймеъ вефрйъ дщфтд тм ъай T ботшлъ дзйсеп ащш овбйшд аъ фтймеън ревгъ дсшип.
https://pubmed.ncbi.nlm.nih.gov/33095157/
зжшд мъзймъ дозчшйн
илрйчеъ дшфййд
бсчйшд щйиъйъ еоид-армйжд ощръ 2024 детшлд дйтймеъ едбийзеъ щм ийфем бгйчеш мщйфеш дфштеъ щйрд бчшб рщйн тн сшип щг. дсчйшд лммд 7 озчшйн бдн дщъъфе 434 оиефмеъ доцейеъ бщмбй ийфем ае дзмод одозмд. босвшъ дозчшйн рбгче севйн щерйн щм гйчеш: гйчеш чмасй (озчш азг), гйчеш зщомй (щмещд озчшйн) егйчеш аежп (зойщд озчшйн). лм ийфем рощк бйп 20 м-30 гчеъ, еощк ддътшбеъ рт бйп 5 м-18 щбетеъ. блм дозчшйн рбзрд дщфМтъ дгйчеш тм айлеъ дщйрд баоцтеъ огг PSQI, ерйъез лемм щм дръерйн дцбйт тм щйфеш оебдч богг жд, мма тгейеъ мдишеврйеъ ощотеъйъ ае мдиййъ фшсен. мтеоъ жаъ, боггйн ресфйн щрбгче бзмч одозчшйн – лое огг ISI мдтшлъ зеошъ айрсеорйд, жоп ддйшгоеъ, ощк дтшеъ бмймд еощк дщйрд длемм – ма роцае ооцайн оебдчйн. мвбй бийзеъ дийфем, геезе дщфтеъ щмймйеъ чмеъ ебеггеъ бмбг, мма тгейеъ мдщфтеъ щмймйеъ ощотеъйеъ. осчръ дзечшйн дйа лй мгйчеш феирцйам мъшен мщйфеш айлеъ дщйрд бчшб рщйн тн сшип щг, ъек щдеа рзщб мийфем биез. тн жаъ, бщм осфш дозчшйн доцеоцн едовбмеъ доъегемевйеъ щм дозчшйн дчййойн, ргшщйн озчшйн ресфйн мдтшлъ ойгъ йтймеъе щм дийфем.
https://pubmed.ncbi.nlm.nih.gov/39299655/
бсчйшд щйиъйъ еоид-армйжд (2021) детшлд ддщфтд щм ийфем боесйчд тм дйбийн фсйлемевййн евефрййн етм айлеъ дзййн бчшб ймгйн земй сшип. дзечшйн осбйшйн лй ийфемйн щерйн ма-фшочемевййн детшле бдъййзс мдчмд тм лаб тм шчт озмъ дсшип, лвеп щйиеъ щм рщйод едшфйд, елп оесйчд ласишивйд мдчмд тм лаб езшгд.
бсчйшд рлмме 11 озчшйн чмйрййн бдн дщъъфе 429 ймгйн тг вйм 18. бозчшйн амд ртщд щйоещ бдътшбеъ ачийбйъ (лвеп щйшд ае рвйрд) ае фсйбйъ (дчщбд моесйчд осевйн щерйн), лм офвщ рощк лзцй щтд бооецт, еъгйшеъ дофвщйн ртд бйп офвщ зг фтой мбйп щрй офвщйн бйен мощк зегщ.
мошеъ дишеврйеъ вгемд бйп дозчшйн, баефп лммй дооцайн ъеолйн бдщфтд дойийбд щм ийфем боесйчд мймгйн земй сшип, бгвщ тм дчмд бъзещъ длаб едзшгд ещйфеш айлеъ дзййн. дзечшйн чешайн мййщен щм ийфем боесйчд ласишивйд згщрйъ, ма фемщрйъ, бтмъ тмеъ роелд етгейеъ обессеъ озчш дъеолеъ бйтймеъд.
https://pubmed.ncbi.nlm.nih.gov/33964406/
бсчйшд щйиъйъ еоид-армйжд, (2021) детшлд дйтймеъ щм ълрйъ оййргфемрс мдфзъъ оъз (MBSR) мщйфеш дщйрд бчшб оиефмйн дозмйойн осшип. бсчйшд рлмме тщшд озчшйн ачшаййн обечшйн бдн сд"л 1,318 ощъъфйн, шебн доезми рщйн. огг доишд дтйчшй дйд айлеъ дщйрд (щрогг боггйн сиргшиййн - Insomnia Severity Index, Pittsburgh Sleep Quality Index), ебресу детшле оггйн ресфйн бдъан мйеорй щйрд щоемае тм йгй дощъъфйн, ае баоцтеъ оггйн фйжйемевййн лвеп вмй оез, чцб мб, ъретеъ тйрййн етег.
роца лй бдщееад мчбецъ бйчешъ щчйбмд аъ дийфем дсиргший, щймеб щм ълрйъ MBSR ъшн мщйфеш айлеъ дщйрд щм дощъъфйн, аемн мма дщфтд ощотеъйъ тм оггй дщйрд. бдщееад мчбецъ бйчешъ щчйбмд дътшбеъ азшъ (лвеп ййтех, CBT ае илрйчеъ мдфзъъ сишс лвеп офвщ збшъй, фтймеъ вефрйъ елгеод), ддщфтд щм MBSR тм айлеъ дщйрд ма дййъд тчбйъ, лащш дщйфеш боггй дщйрд дйд ощотеъй йеъш бчбецъ дбйчешъ.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм дъшеод щм ълрйъ MBSR мщйфеш айлеъ дщйрд бчшб оиефмйн дозмйойн осшип, аемн бщм осфш дозчшйн дчип еъецаеъ щайрп тчбйеъ ргшщйн озчшйн ресфйн байлеъ оъегемевйъ иебд мбйсес йтймеъ ддътшбеъ.
https://pubmed.ncbi.nlm.nih.gov/33460741/
бсчйшд щйиъйъ еоид-армйжд,(2019) длеммъ 17 озчшйн ачшаййн обечшйн бдн 1,111 оиефмйн, роца лй гйчеш ае рчегеъ мзйцд дйе йтймйн мдчмд тм лаб бчшб земй сшип емдфзъъ дщйоещ бощллй лабйн.
https://pubmed.ncbi.nlm.nih.gov/31855257/
бсчйшд щйиъйъ щм озчшйн ачшаййн обечшйн (2020) детшлд ддщфтд щм тйсей бирй тм ъфчег отшлъ дтйлем. бсчйшд рлмме тщшд озчшйн, бдн 464 ощъъфйн дсебмйн оовееп оцбйн бшйаеъййн . бозчшйн дщерйн ртщд щйоещ бовееп илрйчеъ щм тйсей бирй бощк осфш йойн ае маешк лод щбетеъ.
дойоцайн дтйчшййн дтемйн одсчйшд:
-
тйсей бирй ъшн мдчмд тм ъсойрй тцйшеъ бчшб ощъъфйн чщйщйн еощъъфйн тн ишщъ рфецд ае сшип.
-
тйсей бирй щйфш ъретъйеъ дотй бчшб оиефмйн дтебшйн рйъез аешъефгй (skeletal traction).
-
бозчшйн щртшле бчшб ощъъфйн бийфем рошх роца лй тйсей бирй ъшн мщйфеш ъфчег отшлъ дтйлем емдфзъъ рфйзеъ бирйъ.
-
бозчшйн азшйн ма роцад дщфтд оебдчъ мтйсей бирй тм овееп оггйн дчщешйн бъфчег отшлъ дтйлем (лвеп риймъ ощмщмйн, бзймеъ едчаеъ, ъгйшеъ дйцйаеъ ецшйлъ дожеп).
-
бозчшйн щрлмме бсчйшд ма геез тм дщфтеъ щмймйеъ ощотеъйеъ дчщешеъ бтйсей бирй.
дзечшйн ослойн лй роцае ъецаеъ обийзеъ бдъййзс мдщфтд дойийбд щм тйсей бирй, аемн йщ мдощйк ембзеп аъ дйтймеъ бдъййзс мдфштеъ щереъ ботшлъ дтйлем бозчшйн ресфйн.
http://www.sciencedirect.com/science/article/pii/S0965229920318203
бсчйшд очйфд ощръ 2025 рбзрд дйтймеъ щм айоерй веу-рфщ тм айлеъ дзййн едбшйаеъ дрфщйъ бчшб рщйн доъоеггеъ тн сшип щг. дсчйшд лммд 16 оид-армйжеъ е-9 озчшйн ресфйн, ащш сйлое йзг 134 озчшйн чмйрййн обечшйн бдщъъфеъ 9,469 оиефмеъ доцейеъ бщмбй ийфем ае дзмод одозмд. бозчшйн амд рбгчд ддщфтд щм ашбтд севй айоерй веу-рфщ тйчшййн: йевд, иай-ц'й, цй'-черв ебд геап в'йп (сгшд щм ъшвймй ц'й-черв). дооцайн дцбйте тм ъойлд оебдчъ бйевд ллмй йтйм мдчмд тм ъсойрй гйлаеп. роцае тгейеъ зйебйеъ ресфеъ щдйе оевбмеъ ае фзеъ тчбйеъ, лемм ц'й-черв мдчмд тм гйлаеп, айоерй веу-рфщ мщйфеш айлеъ дзййн, мдфзъъ тййфеъ езшгд, елп йевд мщйфеш айлеъ дщйрд. дзечшйн ослойн лй айоерй веу-рфщ, ебфши йевд, тщеййн мъшен мщйфеш айлеъ дзййн едбшйаеъ дрфщйъ щм рщйн тн сшип щг. йзг тн жаъ, дн огвйщйн аъ дцешк ббйцет озчшйн ресфйн байлеъ оъегемевйъ вбедд тм оръ мдтшйк баефп обесс аъ дйтймеъ щм севй ъшвем щерйн.
https://pubmed.ncbi.nlm.nih.gov/40090889/
бсчйшд очйфд ощръ 2024 детшлд дйтймеъ щм гйчеш мийфем бдфштеъ щйрд тм шчт озмъ дсшип. дсчйшд дъбссд тм ръерйн щрасфе о-10 счйшеъ щйиъйеъ еоид-армйжеъ ащш лмме ощъъфйн тн севй сшип овеерйн едъочге бдътшбейеъ щереъ обессеъ гйчеш, мшбеъ гйчеш чмасй, гйчеш зщомй, оечсд, гйчеш аежп ещймебйн бйрйдн. чбецеъ дбйчешъ лмме оиефмйн щчйбме гйчеш огеод, ийфем сиргший ае щма чйбме лм дътшбеъ.
босвшъ дсчйшд детшлд дайлеъ доъегемевйъ щм дозчшйн, дсйлеп мдийд ешоъ деегаеъ щм дооцайн. дтшлд же дтмъд фвойн оъегемевййн одеъййн, бтйчш бщм дйтгш чшйишйерйн бшешйн мдлммд емдзшвд щм озчшйн. йеъш оозцйъ дсчйшеъ девгше лбтмеъ сйлеп вбед мдийд, бйп дйъш тчб айъеш змчй щм озчшйн еай тойгд бфшеиечем озчшй. мошеъ щошбйъ дсчйшеъ дъафййре бшоъ гйеез вбедд йзсйъ, шоъ дшайеъ длеммъ девгшд лроелд. тн жаъ, рйъез дооцайн оцбйт тм лк щмгйчеш тщей мдйеъ феирцйам мщйфеш айлеъ дщйрд бчшб земй сшип дсебмйн одфштеъ щйрд. шеб дсчйшеъ вн дгвйще аъ фшефйм дбийзеъ дзйебй щм дийфем. дзечшйн ослойн лй ау тм фй щроца феирцйам мийфем бгйчеш, ргшщъ ждйшеъ бфйшещ дъецаеъ тчб овбмеъ оъегемевйеъ едтгш ъойлд озчшйъ осфчъ. йщ цешк бозчшйн айлеъййн йеъш, тн оъегемевйд ощефшъ, дфзъъ дийеъ ещйфеш бшоъ дгйеез тм оръ мбсс аъ дйтймеъ щм гйчеш мийфем бдфштеъ щйрд тм шчт озмъ дсшип.
https://pubmed.ncbi.nlm.nih.gov/39128532/
бозчш ачшай обечш (2020) детшлд ддщфтд щм илрйчъ дшвтд (BRR - Benson's Relaxation Response) тм айлеъ дщйрд едъйабеп, бчшб земй сшип дочбмйн лйоеъшфйд. илрйчд же обессъ тм тчшереъ доййргфемрс еъешоъ мдшвтд баоцтеъ дфзъъ дфтймеъ щм отшлъ дтцбйн даеиереойъ. бозчш рлмме 84 оиефмйн, ащш земче ачшайъ мчбецъ ддътшбеъ ае мчбецъ дбйчешъ. дощъъфйн бчбецъ ддътшбеъ моге аъ илрйчъ ддшвтд, едъбчще мййщн аеъд фтоййн бйен бощк 5 йойн шцефйн баоцтеъ дажрд мдешаеъ баежрйеъ. дощъъфйн бчбецъ дбйчешъ чйбме аъ дийфем дсиргший бмбг.
роца лй 24 е-48 щтеъ мазш сйен ъчефъ ддътшбеъ дощъъфйн щбйцте аъ илрйчъ ддшвтд гйеезе тм щйфеш байлеъ дщйрд ебъйабеп, бдщееад мощъъфйн бчбецъ дбйчешъ. ма геез тм дщфтеъ щмймйеъ.
дзечшйн ослойн лй рйъп мтщеъ щйоещ б-BRR ласишивйд ощмйод мщйфеш айлеъ дщйрд едъйабеп бчшб земй сшип дочбмйн лйоеъшфйд, аемн йщ мащщ аъ дооцайн бозчшйн ресфйн тн осфш ощъъфйн вгем йеъш еощк отчб ашек йеъш.
https://www.sciencedirect.com/science/article/abs/pii/S0965229919314876
озчш чмйрй ачшай обечш (оай 2016) бе рбгчд ддщфтд щм ъелрйъ оййргфемрс мщйфеш ъсойрйн фсйлемевййн ефйжййн бчшб рщйн щдзмйое осшип дщг.
бозчш рлмме 322 ощъъфеъ ащш земче баефп ачшай мщъй чбецеъ: ъелрйъ оййргфемрс бъ 6 щбетеъ ае мчбецъ дийфем дсиргший.
дзечшйн дтшйле аъ дъсойрйн дфсйлемевййн (гйлаеп, зшгд, сишс ефзг одйщреъ дозмд) едъсойрйн дфйжййн (ъщйщеъ елаб) бсйен дълрйъ мазш 6 щбетеъ емазш 6 щбетеъ ресфйн.
роца лй бчшб ощъъфеъ бълрйъ доййргфемрс зм щйфеш оебдч сиийсийъ бшоъ дзшгд едфзг одйщреъ дозмд, елп бъзещъ дъщйщеъ, бдщееад мчбецъ дбйчешъ.
ддщфтд щм ъелрйъ доййргфемрс дййъд ощотеъйъ бойезг бчшб ощъъфеъ щдйе тн шоъ дсишс двбедд бйеъш.
https://www.nlm.nih.gov/medlineplus/news/fullstory_159172.html
бозчш дътшбеъй ощръ 2025 детшлд ддщфтд щм ийфем шййчй мдчмд тм ъсойрйн дчщешйн бийфемй лйоеъшфйд. дозчш дъчййн бщъй ошфаеъ зех, ебосвшъе дъбчще дощъъфйн мдтшйк аъ шоеъ дъсойрйн еъзещъ дшеезд длммйъ мфрй еазшй ийфем шййчй бп 15-20 гчеъ щрйъп бодмк чбмъ длйоеъшфйд. догвн лмм 268 оиефмйн, бвйм ооецт щм 63, щчйбме бск длем 392 ийфемй шййчй. роца лй бтчбеъ ддътшбеъ зм щйфеш оебдч, ощотеъй обзйрд чмйрйъ, блм дъсойрйн щрбгче: лаб, тййфеъ, зшгд, бзймд елп бъзещъ дшеезд длммйъ. дощъъфйн гйеезе тм зеейд зйебйъ, щъшод мдшвтд ощотеъйъ емдчмд бъсойрйн. дзечшйн ослойн лй ийфем шййчй босвшъ ийфем лйоеъшфй тщей мъшен мдчмд тм дъсойрйн емщфш аъ айлеъ зееййъ доиефм, ак огвйщйн аъ дцешк бозчшйн ресфйн мбзйръ ддщфтеъ ашелеъ диеез емдтшлъ ййщен дъелрйъ боесгеъ шфеаййн ресфйн.
https://pubmed.ncbi.nlm.nih.gov/39613272/
озчш зък (2019) дтшйк аъ доегтеъ мйевд лийфем ъеок сшип, бчшб 303 ощъъфйн бвймай 18 еотмд доаебзрйн бсшип. бодмк ъчефъ дозчш, щйтешй йевд децте мма тмеъ млмм даелмесййд щм земй сшип бевшйн бошлж абшосеп мсшип баерйбшсйиъ фрсймбрйд. дщйтешйн дйе фтоййн бщбет бщтеъ дйен.
дощъъфйн рщаме мвбй оегтеъ мъшвем йевд ллмй ийфемй еафщшейеъ дъвебд лмме: (1) ма оегт ема ртщд бйгт щйоещ (2) оегт ема ртщд бйгт щйоещ (3) оегт еощъощ.
двйм дооецт щм аелмесййъ дсчш дйд 57.8 (23.1-82.3). дабзреъ дщлйзеъ бйеъш бсшип дйе:
щг (n=95, 31.4%), бйъ зжд (n=43, 14.2%), доиемевй (13.9% ,n=42) еотшлъ дтйлем (n=37, 12.2%).
оъек лмм дземйн, 149 (53.8%) зме бсшип вшешъй. дземйн иефме брйъез (54.5%, n=165), лйоеъшфйд ( (n=272, 89.8%) едчшреъ (n=145, 47.9%).
мдмп сйлен дооцайн:
- лщрщаме тм оегтеъ ещйоещ бъелрйъ дйевд дощмйод, 56% (n=171) одоиефмйн гйеезе тм зесш оегтеъ, 115 земйн (38%) дйе оегтйн мъелрйъ дйевд ак ма рйцме дщйоещ бд, е-5.6% (n=17) дйе оегтйн мд евн рйцме дщйоещ бд.
- земйн вбшйн йеъш дйе оегтйн мйевд (72.4% мтеоъ 48.8%, p=0.045).
- амд щиефме бчшйрд дйе йеъш оегтйн мйевд (p=0.003).
- мошеъ щайрд ощотеъйъ, дййъд овод моегтеъ бчшб земйн цтйшйн йеъш (p=0.076) еземйн ощлймйн йеъш (p=0.064).
- доегтеъ ма дщъръд мфй вжт, оцб ощфзъй, сев сшип ае щмб сшип.
дзечшйн ослойн лй асфчъ щйтешй йевд бзйрн айрд осфчъ, олйееп щосфш рйлш щм земйн ма дйд оегт мщйшеъ. ллм щоътцоеъ тгейеъ мийфемйн ъеолйн лое йевд мийфем бъсойрйн дчщешйн мсшип еийфем бсшип, осйшъ ойгт оецмз тм ийфемйн осев аме ъдйд чшйийъ.
https://www.ncbi.nlm.nih.gov/pubmed/31274335
бозчш фйймеи чмйрй ма обечш,(2020) щртшк бчргд, рбгчд ддщфтд щм тйсей бчшб ймгйн земй сшип, дочбмйн ийфем фмйаийбй. бозш рлмме 8 ймгйн бвймай 10-17. лм дймгйн чйбме тйсей щрощк 60 гчеъ фтн бщбет мощк 4 щбетеъ, ъек дъаод моцбе двефрй едбшйаеъй щм дймг. дймгйн дъбчще мгшв аъ шоъ длаб едгавд мфрй еазшй лм ийфем, ебсйен ддътшбеъ мома щамерйн дтесчйн байлеъ дзййн, шоъ длаб едрлереъ мчбмъ дийфем.
одъецаеъ темд лй мазш щрй ийфемйн змд йшйгд бшоъ длаб емазш ийфем азг змд йшйгд бшоъ дгавд. тн жаъ, ма роцае дбгмйн оебдчйн бъсойрй длаб ебайлеъ дзййн бйп ръерй дбсйс мбйп сйен ддътшбеъ. дощъъфйн дтшйле баефп зйебй аъ дийфем ема геез тм дщфтеъ щмймйеъ. дзечшйн ослойн лй дтйсей ъшн мщйфеш оййгй бъзещъ длаб едгавд, аемн ддщфтд ма рщошд маешк жоп.
https://pubmed.ncbi.nlm.nih.gov/31987232/
бозчш зък бе рлмме 240 земй сшип (аевеси 2014) роца лй двешойн дорбайн йтймеъ вбедд йеъш щм ийфем фмйаийбй леммйн бшйаеъ шезрйъ
ещйоещ басишивйеъ ийфем овеереъ.
http://www.ncbi.nlm.nih.gov/pubmed/25090913
бозчш дътшбеъй (ма обечш) (2019) детшлд дъшеод щм ълрйъ мдфзъъ сишс обессъ оййргфемрс (MBSR) лзмч одийфем дфмйаийбй дшащерй бземй сшип вшешъй. дозчш ртшк бйзйгд даерчемевйъ ббйъ земйн байимйд. ддщъъфеъ бълрйъ децтд м-25 оиефмйн щдефре мийфем фмйаийбй, одн 20 рлмме бозчш. дълрйъ лммд щоерд офвщйн щбетййн щм 2.5 щтеъ, офвщ щм 4.5 щтеъ бйп дщбет дщйщй едщбйтй, езцй щтд бйен щм ъшвем тцоай. дълрйъ детбшд тм йгй огшйк оесок ебрелзеъ щм фсйлемев чмйрй, шефа еазеъ. дзечшйн дтшйле аъ ойгъ ддйълреъ едчбмд щм дълрйъ елп огге аъ шоъ длаб еоцб дшез бчшб 16 одощъъфйн. бресу, ртшле шайереъ теоч зцй-оебрйн тн 8 одощъъфйн. ддйтреъ мълрйъ дййъд 75%. роца лй ддътшбеъ сййтд мощъъфйн мфъз тогд очбмъ йеъш моцбн еблк мщйфеш ддъоеггеъ тн зшгд елаб. бресу, дълрйъ ъшод мщйфеш еейсеъ оцб дшез еъолд бзйбеш щм доиефмйн мтшлйдн емаоерън.
дзечшйн ослойн лй щймеб щм ълрйъ оййргфемрс лзмч одийфем дфмйаийбй дйрд йщйод еочебмъ дйиб тм йгй доиефмйн, етщейд мъшен мдъоеггеъ тн лаб емсфч джгореъ мдчмд швщйъ ешезрйъ.
https://pubmed.ncbi.nlm.nih.gov/31780005/
бозчш бе дщъъфе 121 рщйн щтбше бйефсйд бщг (фбшеаш 2016) роца лй дажрд могйицйд оегшлъ ъшод мдфзъъ шоъ длаб едажрд могйицйд ае моежйчд ъшод мйшйгд бшоъ дзшгд бодмк дийфем ебшоъ дъщйщеъ мазш олп.
http://www.ncbi.nlm.nih.gov/pubmed/26853501
счйшд доъашъ аъ дъшеод щм дшфеад дчешйарйъ досешъйъ мшфеад доегшрйъ, ебойезг мийфем бозмъ дсшип, лйееп щоцйтд ийфем шб ъзеой длемм щйреййн баешз дзййн, щйоещ бфешоемеъ цозй ошфа, гйчеш, оечсд, фтймеъ вефрйъ осешъйъ еогйицйд тм оръ мдзжйш аъ дайжеп бйп двеу, дрфщ едшез.
https://www.ncbi.nlm.nih.gov/pubmed/24282099
бге"з (афшйм 2017), щфешсн оитн давегд маерчемевйд айрившийбйъ, оецвеъ дрзйеъ чмйрйеъ обессеъ шайеъ мщйоещ бийфемйн айрившийбййн бодмк емазш дийфем бсшип дщг, бдъййзс мдъеейеъ чмйрйеъ сфцйфйеъ.
бдъбсс тм дооцайн щфешсое бйп дщрйн 1990-2015, дзечшйн ослойн одн дийфемйн дайрившийбййн щроцае йтймйн бдъййзс млм дъеейд чмйрйъ:
- дфзъъ зшгд/сишс: ийфем боесйчд, огйицйд, рйдем оъзйн ейевд.
- ийфем бгйлаеп/дфштеъ оцб шез: огйицйд, илрйчеъ дшвтд, йевд, тйсей еийфем боесйчд.
- щйфеш айлеъ дзййн: огйицйд ейевд.
- дчмд тм бзймеъ едчаеъ бтчбеъ ийфемй лйоеъшфйд: гйчеш ерчегеъ мзйцд.
дъеейеъ ресфеъ тбешп ма роцае ийфемйн бшоъ йтймеъ вбедд леммеъ ъвебеъ тешйеъ мийфемй чшйрд, ъщйщеъ, мйофагод, рейшефъйд дйчфйъ лъецад оийфемй лйоеъшфйд, лаб, дфштеъ щйрд евмй зен.
одге"з темд лй ма оеомх мдщъощ бацийм-м-чшрйийп морйтъ рейшефъйд дйчфйъ дчщешд бийфемй лйоеъшфйд, бщм дщфтд щмймйъ афщшйъ едзошъ дъсойрйн. лое лп, ма роцае тгейеъ обессеъ мщйоещ бъесфй ъжерд ецозй ошфа мдфзъъ ддщфтеъ дщмймйеъ щм дийфем бсшип дщг.
дзечшйн ослойн лй чййоъ ъойлд озчшйъ мйтймеъ щм ийфемйн айрившийбййн, бойезг ийфемй веу-рфщ, лийфем ъеок бодмк дийфем бсшип дщг. тн жаъ, чййоеъ щйиеъ айрившийбйеъ ресфеъ щайп осфйч тгейеъ тм оръ мчбет одй йтймеъп.
https://www.ncbi.nlm.nih.gov/pubmed/28436999
бдъбсс тм дръерйн оозчш ачшай обечш, (2019) бе рлмме 380 обевшйн земй сшип, роца лй ддщфтд щм дътшбейеъ овт (тйсей ае овт бмбг) оещАфтъ огйлаеп еоъсойрйн фсйлемевййн, емлп ййълп еъдйд ъетмъ мщймеб дътшбейеъ фсйлемевйеъ мщйфеш дйтймеъ щм ийфемй овт.
https://pubmed.ncbi.nlm.nih.gov/31519267/
бозчш ачшай обечш (сфиобш 2017) детшлд дъшеод щм ъшвем йевд ийбийъ мщйфеш дщйрд едъщйщеъ бчшб земеъ сшип дщг (бщмбйн 1-3) дочбмеъ ийфемй лйоеъшфйд.
дощъъфеъ земче баефп ачшай мдщъъфеъ бъшвем йевд ийбийъ (74 рщйн) ае бъшвем оъйзеъ (68 рщйн) мощк 4 офвщйн бодмк ъчефъ дийфем длйоеъшфй е-3 офвщйн ресфйн бодмк 6 дзегщйн мазш олп - бресу мъшвем тцоай ббйъ. лое лп, бозчш рлммд чбецъ бйчешъ, щчйбмд аъ дийфем дсиргший мсшип дщг бмбг (85 рщйн). оггйн майлеъ дщйрд емшоъ дъщйщеъ расфе бъзймъ дозчш, мазш щбет, емазш 3, 6 е-12 зегщйн.
баефп лммй ма роцае дбгмйн бйп дчбецеъ бйзс майлеъ дщйрд ае мшоъ дъщйщеъ маешк жоп. тн жаъ, мазш щбет, дрщйн бчбецъ дйевд гйеезе тм шод роелд йеъш щм дфштеъ бодмк дйен бдщееад мщъй дчбецеъ дазшеъ. оръерй ачийвшфйд (рйиеш жорй дщйрд едтшеъ) темд лй осфш гчеъ дтшеъ бодмк дщйрд дйд вбед йеъш бчбецъ доъйзеъ, бдщееад мчбецъ дйевд ебдщееад мчбецъ дбйчешъ. бресу, бчшб рщйн щгйеезе тм ъшвем йевд мфзеъ фтоййн бщбет бъчефъ дотчб оггй айлеъ дщйрд едачийвшфйд дйе иебйн йеъш мазш 3 е-6 зегщйн, бдщееад мрщйн щма ъшвме йевд бъчефъ дотчб елп бдщееад мрщйн бчбецъ дбйчешъ. рйъп мслн лй мъшвем йевд баефп чбет тщейд мдйеъ ъшеод мщйфеш айлеъ дщйрд бчшб рщйн тн сшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/28940301
бозчш шишесфчийбй (фбшеаш 2017), щртшк бйщшам, детшлд дйтймеъ щм гйчеш ешфмчсемевйд мийфем брейшефъйд дйчфйъ лъецад олйоеъшфйд бчшб рщйн тн сшип дщг. дзечшйн оцййрйн лй рейшефъйд дйчфйъ дйрд ъефтъ мееай щлйзд оаег щм ийфемй лйоеъшфйд, щлйен айп мд ийфем йтйм.
бозчш ртщд щйоещ бшщеоеъ дшфеайеъ щм 30 оиефмеъ, ащш чйбме ийфем ощемб бгйчеш ешфмчсемевйд бочбйм млйоеъшфйд бщм дефтъ ъсойрйн тцбййн. дийфем ртшк тм фй фшеиечем щфеъз бошлж мшфеад ощмйод еайрившийбйъ бошлж дшфеай ъм-абйб, елмм 1-2 офвщйн щбетййн щм гйчеш (20 гчеъ) ешфмчсемевйд (30-40 гчеъ). бооецт, доиефмеъ дзме аъ дийфем 105 йойн мазш дъзмъ длйоеъшфйд едщъъфе б-11 офвщйн бооецт. йтймеъ дийфем детшлд тм фй зеошъ ъсойрй дрейшефъйд бъзймъ ъчефъ дийфем, бодмлд ебсйеод. обйп 28 оиефмеъ тн шщеоеъ шфеайеъ омаеъ, 20 оиефмеъ сбме орейшефъйд срсешйъ, 7 орейшефъйд оеиешйъ е-1 орейшефъйд срсешйъ еоеиешйъ.
обйп 20 доиефмеъ тн рейшефъйд бгшвд 1 тг 2, шч 2 оиефмеъ гйеезе тм ъсойрйн 12 зегщйн мазш дъзмъ дийфем дощемб, елм 8 доиефмеъ тн рейшефъйд бгшвд 3-4 гйеезе тм дтгш ъсойрйн мазш 12 зегщйн. баефп лммй 93% одоиефмеъ гйеезе тм дтгш ъсойрйн мазш щрд оъзймъ дийфем дощемб. дзечшйн ослойн лй мийфем ощемб бгйчеш ебшфмчсемевйд феирцйам ийфемй рйлш мщйфеш ъсойрй рейшефъйд тм шчт лйоеъшфйд, аемн йщ мащщ аъ дооцайн бозчш длемм чбецъ бйчешъ елп мдтшйк одй ддщфтд дорйтъйъ щм ийфем жд.
https://www.ncbi.nlm.nih.gov/pubmed/28150504
зжшд мъзймъ дозчшйн
цозй ошфа
лммй еозчшйн отешбйн | ъд йшеЙч | лМешлен елМеМшлеойп | фМишййъ шййщДй | вД'йрсрв | чгг чшеоДй | щеМщ чйшз | сеЙйд | чтшеМшйъ сДйрйъ | еДйърйд | вгДймп оцей | щшАбйип оцей | фешоемеъ сйрйеъ | щорйн аъшййн
лммй еозчшйн отешбйн
бсчйшд щйиъйъ щм озчшйн чмйрййн (2020) детшлд ддщфтд щм биа-вмечп, доефч офишйеъ, лийфем ощмйн бчшб земй сшип дочбмйн ийфем ревг сшип чербрцйерамй. бсчйшд рлмме 16 озчшйн бдн 1,650 земйн доаебзрйн тн ъщтд севй сшип.
бозчшйн амд дщъоще ббиа-вмечп, доефч осевйн щерйн щм щошйн ефишйеъ, лащш дййъд щереъ вгемд бйп дозчшйн бойреп, аефп дриймд, еощк ддътшбеъ. баефп лммй роца щдщйоещ ббиа-вмечп дйд биез ерсбм дйиб. бшеб дозчшйн роца лй риймъ биа-вмечп бочбйм мийфемй лйоеъшфйд ае шгйеъшфйд дййъд омеед бойъеп дгйлей дзйсерй е/ае бдацъ дщйчен щм ъай дгн дмбрйн. йзг тн жаъ, бзмч одозчшйн ма роцад дщфтд оебдчъ. ддщтшд дйа, щау тм фй щбиа-вмечп деа сйб щайре оътлм, ддщфтд щме дйа гшк чщйшд мъай арийвп (APC) ботй дгч, гбш двешн мъайн амд мщфш аъ фтймеъ дотшлъ дзйсерйъ. дзечшйн ослойн, лй бщм ддишеврйеъ бйп дозчшйн егйеез змчй щм дръерйн, ма рйъп мчбет осчрд бшешд, ергшщйн озчшйн ресфйн мдтшлъ дйтймеъ щм биа-вмечп лийфем ощмйн бчшб земй сшип.
https://pubmed.ncbi.nlm.nih.gov/33309412/
бсчйшд щйиъйъ (2020) отшйлйн дзечшйн аъ дйтймеъ дийфемйъ щм цозй ошфа, доелшйн тм йгй отшлъ дбшйаеъ ббшжйм, мдчмд тм ъефтеъ дмееай щм ийфемйн ревгй сшип (лйоеъшфйд ешгйеъшфйд). бсчйшд рлмме 29 озчшйн ачшаййн обечшйн, ащш ртшле б-15 огйреъ (9 одозчшйн ртшле байшап). бозчшйн амд детшле 12 цозй ошфа ае щймебйн щерйн обйп 71 дцозйн доелшйн ботшлъ дбшйаеъ дбшжймайъ: алймад аму дтмд (Achillea millefolium), щен (Allium sativum), амеешд (Aloe vera), чоеойм (Matricaria (Chamomilla) recutita), цйфешрй зъем (Calendula officinalis), лешлен (Curcuma longa), сейд (Glycine max), в'йрв'ш (Zingiber officinale), ртрт зшйфд (Mentha x piperita), емзк вгем (Plantago major).
мдмп дооцайн дтйчшййн бдъййзс млйоеъшфйд:
- обйп дозчшйн бдн детшлд дйтймеъ щм в'йрв'ш мдчмд тм бзймеъ едчаеъ, 6 озчшйн дцбйте тм дйтймеъ щм в'йрв'ш мбг ае бщймеб тн чоеойм лийфем ощмйн, мтеоъ 6 озчшйн бдн ма роцад йтймеъ оебдчъ.
- в'йрв'ш роца йтйм вн мдчмд тм тцйшеъ.
- бдъййзс моечежйийс бфд, щийфеъ фд, добессеъ тм алймад ае тм чоеойм, роцае йтймеъ мийфем ае морйтд, аемн дщйоещ бмзк вгем ае бщймеб щм чоеойм еорид ма роца йтйм.
- ъесу сейд (MicrSoy-20) ъшн мщйфеш ъсойрй тййфеъ езесш ъйабеп.
- дщйоещ бщен ма роца йтйм морйтъ зен рейишефрй (зен домеед ойтеи ъай гн мбрйн).
мдмп дооцайн дтйчшййн бдъййзс мшгйеъшфйд:
- бщрй озчшйн щйоещ зйцерй бцйфешп зъем ае бамеешд ма роца йтйм морйтъ ъвебд тешйъ ае мийфем бд, бчшб земй сшип шащ ецееаш. аемн, бщрй озчшйн азшйн дщйоещ бцозйн амд роца йтйм морйтъ гшоийийс емийфем бе.
- мийфем боечежйийс бфд, бозчш азг роцад йтймеъ мщйоещ блешлен ебозчш азш дщйоещ бщийфъ фд добессъ тм амеешд ма роца йтйм.
- ощзъ амеешд дййъд йтймд мийфем бгмчъ фй дибтъ (фшечийийс), бчшб земйн тн сшип бажеш давп, елп мдчмд тм сйбелйн дчщешйн блк лвеп лаб, ъзещъ цшйлд ае чещй мдъшечп.
дзечшйн ослойн лй йщрп тгейеъ доцбйтеъ тм дйтймеъ щм цозй ошфа осейойн морйтд емийфем бъефтеъ дмееай дчщешеъ бийфем ревг дсшип, еблк мъшен мщйфеш айлеъ дзййн щм доиефмйн.
https://pubmed.ncbi.nlm.nih.gov/32147034/
бсчйшд леммъ щм счйшеъ щйиъйеъ еоид-армйжеъ щм озчшйн чмйрййн,(2020) детшле дтгейеъ бдъййзс мдщфтд дбшйаеъйъ щм амеешд (Aloe vera). бсчйшд рлмме 20 озчшйн, одн 10 счйшеъ щйиъйеъ бдп ма ртшк рйъез лоеъй, е-10 счйшеъ щйиъйеъ бдп ртшлд оид-армйжд. бдъбсс тм счйшеъ щйиъйеъ щма лмме рйъез лоеъй, роца феирцйам мдщфтд ойийбд щм амеешд боцбйн щм фсешйажйс, ъсойрй GERD, тцйшеъ, фшечийийс тм шчт ийфемй чшйрд, фцтй дрчд, гмчеъ зрйлййн, ачрд есбешйад. ма роцад йтймеъ мдчмд тм йебщ бфд лъецад оийфемй чшйрд, мщйфеш айлеъ дзййн бчшб оиефмйн тн ъсоеръ дотй дшвйщ, ае мщйфеш ъсойрй рейшефъйд селМшъйъ. дсчйшеъ бдп ртшлд оид-армйжд дйе обессеъ тм сд"л 94 озчшйн бдн 14,352 ощъъфйн, одн б-82% одозчшйн ртщд щйоещ зйцерй бамеешд еб-18% ртщд щйоещ бриймд феойъ. блм дозчшйн детшле 71 ъецаеъ щереъ мщйоещ бамеешд. обйп лмм дъецаеъ, 47 ъецаеъ роцае бтмеъ оебдчеъ сиийсийъ, аемн тгейеъ обессеъ роцае шч бдъййзс мйтймеъ щм амеешд морйтъ гмчъ ешйгйн (фмбйийс). тгейеъ азшеъ бдъййзс мдщфтд щм амеешд тм ъецаеъ ресфеъ, бйрйдп бшйаеъ дфд, дфзъъ шоъ двмечеж, ийфем бфцтйн етег дйе байлеъ роелд ае ма дйе оебдчеъ сиийсийъ. дзечшйн ослойн лй мошеъ щбаефп лммй роцае дщфтеъ ойийбеъ мщйоещ бамеешд, ргшщйн озчшйн ресфйн байлеъ оъегемевйъ вбедд тм оръ мдощйк ембзеп аъ дйтймеъ дчмйрйъ щм амеешд.
https://pubmed.ncbi.nlm.nih.gov/32924222/
бсчйшд (2022) оецвйн дооцайн дфшд-чмйрййн едчмйрййн бдъййзс мйтймеъ щм цозй ошфа морйтд емийфем боечежйийс бфд, лдщфтд щмймйъ щм дийфем ревг дсшип. дзечшйн оцйвйн аъ дорврерйн дйщйшйн едтчйфйн дотешбйн бдъфъзеъ оечежйийс бфд лъецад оийфемй лйоеъшфйд ае чшйрд еофшийн аъ дооцайн оозчшйн щртшле бчшб брй агн, бтмй зййн ае гвйоеъ ъайн. босвшъ дсчйшд офешийн дооцайн бдъййзс мшлйбйн дцозййн дбайн: лешлеойп, сймйошйп, ъд осевйн щерйн долймйн ътшебеъ щереъ щм цозй ошфа, цйфешрй зъем (Calendula officinalis), чеошйп, чеешцийп, амеешд (Aloe), дфешоемд дйфрйъ Hangeshashinto , в'йрв'ш (Zingiber officinale), в'йрсрв чешйарй аген (Panax ginseng) ефшефемйс. одсчйшд темд лй йщрп тгейеъ мдщфтд ойийбд щм овееп шлйбйн цозййн, лащш йщрп тгейеъ обессеъ бтйчш мйтймеъ щм лешлеойп, амеешд ефшефемйс. тн жаъ, осфш дозчшйн дчмйрййн чип ейщрд дишеврйеъ вгемд бйп дозчшйн ащш очщд тм чбйтъ осчрд зг ощотйъ.
https://pubmed.ncbi.nlm.nih.gov/34709682/
бсчйшд (2021) грйн дзечшйн бдщфтд щм дшлйб дцозй бшбшйп бщйфеш йтймеъ дийфем ревг дсшип ебдврд офрй дщфтеъйе дщмймйеъ, бгвщ тм орврерй дфтемд дотешбйн едаъвшйн бййщен дчмйрй.
https://pubmed.ncbi.nlm.nih.gov/33559280/
бсчйшд (2021) оецвеъ дтгейеъ дозчшйеъ, бтйчш оозчшйн фшд-чмйрййн, бдъййзс мщйоещ досешъй, мдшлб длйой емфтймеъ дфшочемевйъ щм ртрт (Mentha spicata), лемм фтймеъ арий-ойчшебйамйъ, ревгъ зоцеп, ревгъ сшип, ревгъ гмчъ еовйрд тм длбг.
https://pubmed.ncbi.nlm.nih.gov/34087400/
бсчйшд, (2020) щртшлд тм йгй зечшйн овшорАйд, рбгч дфтш бйп дщйоещ бшфеаъ цозйн айшефайъ осешъйъ мийфем боечежйийс бфд, мбйп дтгейеъ дозчшйеъ дчййоеъ. дзечшйн осбйшйн лй оечежйийс бфд дйре ъефтъ мееай щм дийфем ревг дсшип, лащш оиефмйн шбйн ощъощйн бцозй ошфа мдчмд тм дъсойрйн. тн жаъ, дйгт мвбй цозй дошфа доеомцйн бшфеаъ дцозйн дайшефайъ досешъйъ, дщАфтън ейтймеън - дйре оети бйеъш.
босвшъ дозчш, дзечшйн бзре одн цозй дошфа доелшйн бщйоещ досешъй еаъ дтгейеъ дозчшйеъ дчййоеъ бдъййзс мцозйн амд. бсчйшд щм 14 сфшйн, дтесчйн бшфеаъ дцозйн дайшефайъ досешъйъ, жеде 78 цозй ошфа доеомцйн мийфем боечежйийс бфд. одозчш темд лй чййн фтш ощотеъй бйп дйгт досешъй мбйп озчшйн дбезрйн аъ ддщфтд щм цозйн амд. баефп лммй, дийфем дцозй роца йтйм мдчмд тм оечежйийс бфд, елп мийфем бгмчеъ зрйлййн.
йщрп тгейеъ йзсйъ обессеъ мвбй дйтймеъ щм чоеойм (Matricaria recutita), ошеед шфеайъ (Salvia officinalis), цйфешрй зъем (Calendula officinalis) еъйойп (Thymus spp) мийфем боечежйийс бфд. дзечшйн ослойн лй озчшйн чмйрййн бдн рбгче цозй ошфа доелшйн бшфеаъ дцозйн дайшефайъ досешъйъ дйрн ргйшйн, аемн роцае тгейеъ обийзеъ бдъййзс мйтймеъ щм ашбтд цозй ошфа мийфем боечежйийс бфд.
https://pubmed.ncbi.nlm.nih.gov/31955287/
бсчйшд (2020) оецвйн дооцайн дфшд-чмйрййн дтесчйн бфтймеъ дфшочемевйъ щм фешфешйп (Purpurin), шлйб аръшчеейрерй доцей бфеад дегйъ (Rubia cordifolia), бгвщ тм фтймеъе ревгъ дзоцеп, дтеогъ ббсйс дщАфтъе дойийбд тм доез еревгъ дсшип.
https://pubmed.ncbi.nlm.nih.gov/33254282/
бсчйшд (2019) оцйвйн дзечшйн аъ дтгейеъ дфшд-чмйрйеъ бдъййзс морврерй дфтемд дотешбйн бфтймеъ ревгъ дсшип щм 16 ойрйн щм щен ешлйбйдн дфтймйн, лбсйс мфйъез ийфемйн згщрййн мозмъ дсшип.
https://pubmed.ncbi.nlm.nih.gov/31464060/
бсчйшд (2019) грйн дзечшйн бфтймеъ дшфеайъ щм оешйрвд (Moringa oleifera), бгвщ тм ддщфтд лрвг щвщев ъайн сширййн (арий-фшемйфшийбйъ).
https://www.ncbi.nlm.nih.gov/pubmed/30241049
бсчйшд (2019) грйн дзечшйн борврерйн доемчемшййн дтеогйн ббсйс ддщфтд дойийбд щм шлйбйн саферйрйн цозййн лрвг вйгемйн сширййн ефтймеън мдвбшъ йтймеъ длйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/31294509
бсчйшд (2018) офешийн дооцайн дфшд-чмйрййн ечмйрййн дтглрййн бревт мфтймеъ щм оешйрвд (Moringa oleifera) морйтд емийфем бовееп озмеъ лшерйеъ, лемм озмеъ гмчъйеъ, озмеъ тцбйеъ, селшъ есшип.
https://www.ncbi.nlm.nih.gov/pubmed/29534518
бозчш ъцфйъй (йерй 2017) рзчш дфеирцйам мъвебеъ дггйеъ бйп ъшефеъ ебйп ъшефеъ ецозй ошфа бчшб земй сшип.
босвшъ дозчш асфе дзечшйн ръерйн аегеъ лм дъшефеъ ецозй дошфа щрмчзе тм йгй лм оиефм. баоцтеъ зйфещ ршзб боавшй дръерйн жеде дъвебеъ ддггйеъ дъйаешийеъ дчййоеъ, еддщфтд дчмйрйъ дафщшйъ щмдн детшлд тм йгй шечз чмйрй едетбшд маерчемев доифм.
роца лй обйп 149 оиефмйн щрлмме бозчш, 26 оиефмйн (17.4%) дйе бсйлеп мъвебеъ дггйеъ бйп ъшефеъ, щтщейеъ мдйеъ бтмеъ ощотеъ чмйрйъ, лащш шч 4 оиефмйн (2.7%) сбме бфетм оъвебеъ дггйеъ бйп ъшефеъ. риймд щм щъй ъшефеъ ае йеъш бочбйм роцад чщешд бсйлеп вбед фй 2.5 мъвебеъ дггйеъ бтмеъ ощотеъ чмйрйъ (p=0.03).
лое лп, обйп 149 дощъъфйн бозчш, 84 оиефмйн (56.4%) гйеезе тм щйоещ бцозй ошфа бочбйм мийфем дарий-сширй, лащш бчшб 75 оиефмйн (50.3%) дзечшйн жйде 122 ъвебеъ дггйеъ афщшйеъ бйп ъшефеъ мбйп цозй ошфа. йзг тн жаъ, ма геез тм йгй даерчемев доифм тм ъвебеъ дггйеъ чмйрйеъ одн сбме доиефмйн бфетм. цозй дошфа щроцае чщешйн бъвебеъ дггйеъ леммйн: щен (Allium sativum), амеешд (Aloe barbadensis/capensis), арерд (Annona muricata), ъд йшеч (Camelia sinesis), чйфегрйъ (Echinacea angustifolia), вйрче ге-аеръй (Ginkgo biloba), чоеойм (Matricaria recutita), оешйрвд (Moringa oleifera), в'йрсрв чешйарй (Panax ginseng), сфйшемйрд, аерчшйд (Uncaria tomentosa), емшйап (Valeriana officinalis), евфп (Vitis vinifera). дзечшйн оцййрйн лй дозчш тмем сбем одийеъ, щлп доиефмйн ма рбзше баефп ачшай, дтшлъ дщйоещ бцозй ошфа дъбссд тм гйеез тцой щм доиефмйн езмч одъвебеъ ддггйеъ щжеде дйе ъйаешийеъ бмбг бщм дтгш ръерйн чмйрййн. тн жаъ, дн огвйщйн лй баоцтеъ отчб ъшефъй рйъп мждеъ щйтеш вгем щм оиефмйн дроцайн бсйлеп мъвебеъ дггйеъ еблк мщфш аъ йтймеъ дийфем бземй сшип.
дтшъ дотшлъ: жде озчш щрй щбегч дан чййоеъ бфетм ъвебеъ дггйеъ бйп ъшефеъ мцозй ошфа бчшб земй сшип.
бщрй дозчшйн, мошеъ ъвебеъ дггйеъ ъйаешийеъ шбеъ, ма геез тм лм ощотеъ чмйрйеъ бщймеб щм цозй ошфа еъшефеъ. аъ дозчш дщрй бреща афщш мшаеъ лап.
https://www.ncbi.nlm.nih.gov/pubmed/28628392
озчш чмйрй (фбшеаш 2016) ащш ретг мдтшйк аъ дйтймеъ, дбийзеъ едойреп дочсйоамй дрсбм щм гчм ррсй (Serenoa repens), мдчмд тм ъсойрйн бгшлй дщъп - ъефтъ мееай щм ийфемй чшйрд бвбшйн тн сшип дтшоерйъ.
бщмб дшащеп бе дщъъфе 27 оиефмйн, дзечшйн оцае лй дойреп дочсйоамй щрбгч, 960 о"в, рсбм дйиб тбеш ошбйъ доиефмйн. бщмб дщрй, бе дщъъфе 21 оиефмйн, бгче дзечшйн аъ дйтймеъ щм ойреп жд бдщееад мфмсбе бощк 22 щбетеъ.
ма роца дбгм бйп дчбецеъ бцйеп дъсойрйн (IPSS) аемн бчбецъ дийфем зм щйфеш богг айлеъ дзййн (йшйгд бшоъ дзщщеъ) бдщееад мфмсбе. бресу, бчбецъ дфмсбе 2 оъек 11 оиефмйн риме ийфем ъшефъй мъсойрйн бгшлй дщъп мтеоъ 0 оъек 10 оиефмйн бчбецъ ддътшбеъ.
дзечшйн ослойн лй ойреп щм 960 о"в дйре биез ерсбм дйиб аемн йщ мдощйк ембзеп аъ дйтймеъ мдчмд тм ъсойрйн бгшлй дщъп бодмк ийфемй чшйрд.
http://www.ncbi.nlm.nih.gov/pubmed/26891611
озчш чмйрй зг-сойеъ обечш фмсбе (афшйм 2015) щретг мдтшйк аъ дйтймеъ щм щайфъ щоп в'йрв'ш мдчмд тм бзймеъ едчаеъ емщйфеш айлеъ дзййн бчшб земеъ сшип дщг дтебшеъ ийфемй лйоеъшфйд.
бозчш дщъъфе 60 земеъ ащш бощк 5 йойн чйбме ийфем ашеоъшфй длемм щйоещ бщоп в'йрв'ш ае бщоп фмсбе бщайфд бтжшъ щйоещ бщшщшъ дофйцд аъ дщоп баефп дгшвъй.
роца щйфеш чм бшоъ дбзймд ойг мазш дийфем аемн баефп лммй ма роцад ъойлд мщйоещ бщоп в'йрв'ш мдчмд тм бзймеъ едчаеъ. тн жаъ, роца щйфеш бшоъ дбшйаеъ длммйъ, лемм щйфеш бшоъ дъфчег ебшоъ дъйабеп.
http://www.ncbi.nlm.nih.gov/pubmed/26051575
бозчш фшд чмйрй, (2018) щртшк бчшб тлбшйн етм ъайн арещййн, рбгче дорврерйн ащш тщеййн мтоег ббсйс ддщфтд довйрд щм фешоемъ цозй дошфа дсйрйъ Liu Jun Zi Tang офрй сйбелйн тцбййн, лъецад оийфемй лйоеъшфйд (цйсфмаийп). мшеб рдев мдщъощ бфешоемд мийфем бгйсффсйд ъфчегйъ ебгйлаеп елп мдфзъъ ъефтеъ дмееай дчщешеъ бийфем бцйсфмаийп.
тн жаъ, айп осфйч тгейеъ мвбй йтймеъд морйтъ штймеъ тцбйъ. дфешоемд олймд 8 цозй ошфа: аишчиймегс (Atractylodes macrocephala), фйрмйд (Pinellia ternata), чмйфъ оргшйрд (Citrus reticulata), ъош сйрй (Ziziphus jujube), фишййъ фешйд (Poria cocos), щещ чйшз (Glycyrrhiza glabra), в'йрсрв чешйарй (Panax ginseng) ев'йрв'ш (Zingiber officinale). дзечшйн ошайн лй баоцтеъ дщфтд ревгъ зоцеп еейсеъ фтймеъ дойиелергшйд, зщйфд мфешоемд дййъд йтймд морйтъ штймеъ тцбйъ бтчбеъ ийфем бцйсфмаийп.
https://www.ncbi.nlm.nih.gov/pubmed/29690597
озчш чмйрй лфем-сойеъ обечш фмсбе (йреаш 2015) мбгйчъ ддщфтд щм ийфем ъеок бфешоемъ цозй ошфа йфрйъ, Goshajinkigan, мдфзъъ рейшефъйд дйчфйъ бземй сшип чемешчимй. дфешоемд леммъ 11 цозй ошфа: Rehmannia glutinosa, Achyranthes fauriei, Cornus officinalis, Paeonia suffruticosa, Alisma plantago-aquatica, Dioscorea japonica, Dioscorea opposite, Plantago asiatica, Wolfiporia extensa, Aconitum carmichaelii, Cinnamomum cassia.
бозчш рлмме 182 оиефмйн ащш чйбме ийфем лйоеъшфй ощемб mFOLFOX6 (длемм: фмеаешеаешцйм, маечебешйп еаечсмйфмийп) тн дфешоемд дцозйъ бойреп 7.5 вшн 3 фтойн бйен ае фмсбе. роца лй щйтеш доиефмйн ащш аебзре тн рейшефъйд бшод 2 еотмд дйд 50.6% бчбецъ дийфем е-31.2% бчбецъ дфмсбе. дзечшйн ослойн лй дфешоемд ма роцад йтймд морйтъ рейшефъйд лъецад одийфем длйоеъшфй.
http://www.ncbi.nlm.nih.gov/pubmed/25627820
озчш чмйрй лфем-сойеъ (фбшеаш 2015) бе рбгчд ддщфтд щм щийфъ фд долймд алймад аму дтмд тм оечежйийс бфд лъецад оийфемй лйоеъшфйд.
бозчш дщъъфе 56 земй сшип ащш земче ачшайъ мчбецъ дийфем ае мчбецъ дбйчешъ. лм дощъъфйн дъбчще мвшвш 15 о"м щийфъ фд ййтегйъ 4 фтойн бйен мощк 14 йен, лащш бчбецъ дийфем щийфъ дфд длймд вн ойцей алймад.
роца лй бчбецъ дийфем зм щйфеш ощотеъй бшоъ доечежйийс (йшйгд оцйеп ооецт щм 2.39 бъзймъ дийфем м-1.07 мазш 7 йойн е-0.32 мазш 14 йен). мтеоъ жаъ, бчбецъ дбйчешъ змд дзошд боцб доечежйийс (тмййд оцйеп ооецт щм 2.39 бъзймъ дийфем м-2.75 мазш 7 йойн е-2.89 мазш 14 йен). дзечшйн ослойн лй щйоещ балймад дйре йтйм йеъш одийфем дсиргший мийфем боечежйийс бфд бземй сшип.
http://www.ncbi.nlm.nih.gov/pubmed/25667123
озчш фшд-чмйрй (йемй 2015) доцбйт тм дфтймеъ дарий-сширйъ щм тмй ашийщеч (Cynara scolymus) лрвг сшип осев ожеъмйеод бчшен дшйаеъ (цгш / фмаешд).
http://www.ncbi.nlm.nih.gov/pubmed/26136339
бозчш фшд-чмйрй (аечиебш 2015) роца лй Dehydroandrographolide, азг дшлйбйн дфтймйн баргшевшфйс (Andrographis paniculata), отегг ъоеъъ ъай сшип дфд баоцтеъ двбшъ ъдмйлй аеиефвйд.
https://www.ncbi.nlm.nih.gov/pubmed/26356821
счйшд щйиъйъ еоид-армйжд (оай 2015) щретгд мдтшйк аъ дъшеод щм шфеаъ цозйн осешъйъ лийфем ъеок бсшип бмет дау. бсчйшд рлмме 22 озчшйн ачшаййн обечшйн бдн дщъъфе л-2,300 земйн. б-15 оъек дозчшйн щрсчше роцад тмйд бщйтеш ддйщшгеъ, б-7 озчшйн роцад дщфтд йщйшд тм двйгем еб-3 озчшйн роцад рсйвд щм вшешеъ ошезчеъ. дзечшйн ослойн лй щймеб щм шфеаъ цозйн тн ийфем чербрцйермй тщей мдйеъ йтйм мийфем бсшип бмет дау, аемн ргшщйн озчшйн ресфйн бдйчу шзб йеъш.
http://www.ncbi.nlm.nih.gov/pubmed/25698710
счйшд очйфд (афшйм 2015) ащш ослоъ аъ дтгейеъ оозчшйн фшд-чмйрййн мвбй овееп вгем щм шлйбйн цозййн ащш роцае йтймйн морйтд еийфем бсшип дтшоерйъ. длеъбйн оцйвйн аъ орврерй дфтймеъ баоцтеън шлйбйн амд ъешойн мтйлеб двйгем щм ъайн сширййн емтцйшъ ъдмйк змечъ дъа, мгйлей ъдмйлй арвйевржд емтйгег ъдмйлй ъоеъъ ъайн сширййн. бсчйшд оъййзсйн длеъбйн мшлйбйн дцозййн дбайн: афйврйп (фмбеп доцей бцозйн оощфзъ доешлбйн елп бйшчеъ ефйшеъ); ашиойсйрйп ервжшеъйе (дшлйб дфтйм бцоз дмтрд Artemisia); мшлйбйн дфтймйн Baicalin е-Baicalein (доцеййн бцоз чтшешйъ сйрйъ Scutellaria baicalensis); бшбшйп (амчмеайг доефч оцоз дбшбшйъ Berberis); зеоцд биемйрйъ (ишйишфп фрид-цйчмй доефч очмйфъ тх дмбрд Betula papyrifera), чфсайцйп (оцоз дфмфмъ Capsicum); лешлеойп (доефч олешлен Curcuma longa); гайгжайп (айжефмбеп доцей бфемй сейд); гмфйрйгйп (аръецйарйгйп доцей бовееп цозйн, йшчеъ ефйшеъ); EGCG (чилйп доефч оъд йшеч Camellia sinensis); фйсийп (фмберем доефч оовееп цозйн лвеп Acacia greggii); фешоерерийп (фйиеасишевп доцей бъмъп аген Trifolium pratense); зеоцд вамйъ (фемйфрем доцей бжштй трбйн Vitis vinifera); врйсиайп (айжефмбеп доцей бфемй сейд); Gambogic Acid (шлйб доефч одцоз Garcinia hanburyi); в'йрсресйгйн (дшлйбйн дфтймйн бв'йрсрв Panax); дшлйбйн дфтймйн бцоз дмйчешйх дсйрй Glycyrrhiza uralensis, весйфем (шлйб доцей бжштй леърд Gossypium hirsutum); меиаемйп (фмбеп доефч одцоз ддегй бйбдйичй Terminalia chebula); шлйбйн доефчйн оцоз довремйд (Magnolia); мйчефп (чшеиреайг боефч бтйчш отвбрйеъ); Oridonin доефч одцоз Rabdosia rubescens; семфешафп (доцей бйшчеъ оцмйбйн); Phenethyl-isothiocyanat доцей бовееп йшчеъ оцмйбйн; чеешцийп (фмберем доефч отрбйн Vitis vinifera); зеоцд амвйъ (шлйб фемйфремй доцей бтйчш бфйшеъ йтш ешйоеп); Sanguinarine (доефч одцоз сарвеейрашйд Sanguinaria Canadensis); сймйбйрйп (доефч овгймп оцей Silybum marianum); е- Thymoquinone (фйиелйойчм доефч ожштй чцз Nigella sativa); зеоцд аешесемйъ (шлйб ишйишфреайгй доефч одцоз Cornus officinalis).
http://www.ncbi.nlm.nih.gov/pubmed/25875508
счйшд щм озчшйн ачшаййн обечшйн (афшйм 2015) бдн рбгчд дйтймеъ щм шфеаъ цозйн осешъйъ лийфем ъеок бсшип дщг. бсчйшд рлмме 8 озчшйн, щбецте тм сд"л 798 земеъ сшип дщг. бщмещд одозчшйн дзечшйн огеезйн тм щйфеш байлеъ дзййн бдщееад мчбецъ бйчешъ ебщрййн одозчшйн роца щйфеш бсфйшъ ъай дгн дмбрйн бтчбеъ дийфем бцозй ошфа. базг одозчшйн роца щйфеш бвмй дзен ебайлеъ дщйрд бчбецъ дийфем мтеоъ чбецъ дбйчешъ. дцозйн дтйчшййн бдн ртщд щйоещ бозчшйн дйрн: Astragalus membranaceus, Angelica sinensis, Paeonia japonica, Atractylodes ovata, лащш дщйоещ мшеб дйре бфешоемд ема бцоз бегг.
http://www.ncbi.nlm.nih.gov/pubmed/26275657
бсчйшд (йреаш 2017) ослойн дзечшйн аъ дооцайн дтглрййн оозчшйн фшд-чмйрййн ечмйрййн бревт мщйоещ бшлйбйн ибтййн ебцозй ошфа лийфем ъеок бсшип дмбмб.
босвшъ дсчйшд офешийн бдшзбд озчшйн фшочемевййн, бдн рбгч дщймеб дйтйм едъеок щм шлйбйн ибтййн щерйн тн дийфем длйоеъшфй воцйибйп (Gemcitabine), бйрйдн 3,3-Diindolylmethane доцей бйшчеъ оцмйбйн, Thymoquinone доефч ощоп чцз (Nigella sativa), бощфзъ дгметййн рйъп моцеа аъ Cucurbitacin B, ббшечемй ебйшчеъ оцмйбйн ресфйн, рйъп моцеа - sulforaphane, лое лп, Dimethylaminoparthenolide доефч обп-зшцйъ (Tanacetum parthenium) е-Piperlongumine доефч офмфм ашек (Piper longum).
йъшереъ дщймеб щм шлйбйн амд леммйн щйфеш ъфчег отшлъ дзйсеп, гйлей дъчгоеъ двйгем, дфзъъ ъвебеъ щмймйеъ еъефтеъ мееай щм лоеъшфйд ешгйеъшфйд.
бдощк офешийн дооцайн дфшочемевййн бревт мщймеб щм шлйбйн ибтййн тн ийфемйн лйоеъшфййн ресфйн, емвбй дщймеб щм шлйбйн ибтййн щерйн. мгевоа, дщймеб щм весйфем, доефч ожштй леърд, ев'рйсиайп, доцей бсейд, ъешн мтйлеб ъай мбмб сширййн йеъш оащш лм шлйб брфшг. щймебйн ресфйн щроцае йтймйн дн: семфешафп ечеешцийп, wogonin (доцей бчтшешйъ сйрйъ), apigenin е-chrysin елп оифешойп еасфйшйп.
озчшйн чмйрййн шащерййн оцбйтйн тм дфеирцйам щм вйрче ге-аеръй (Ginkgo biloba), лешлеойп (Curcuma longa), гбчеп мбп (Viscum album) ев'рйсиайп. лое лп йщрн ооцайн обийзйн мщйоещ бфешоемд дсйрйъ дчмасйъ Huang-Qin-Tang ебфешоемд досзшйъ PHY906 добессъ тмйд, ащш олймеъ ашбтд цозй ошфа тйчшййн: чтшешйъ сйрйъ (Scutellaria baicalensis), щещ сйрй (Glycyrrhiza uralensis), агоерйъ (Paeonia lactiflora) еъош сйрй (Ziziphus jujuba).
https://www.ncbi.nlm.nih.gov/pubmed/28232946
бсчйшд (йреаш 2016), ослойн дзечшйн аъ дооцайн дтглрййн едъетмъ дчмйрйъ бревт мщйоещ бшлйбйн ибтййн, дфетмйн лрвг осфш осмемй ъчщешъ ъайъ дчщешйн бдъфъзеъ сшип длбг.
тм бсйс ооцайн фшд-чмйрййн дзечшйн осбйшйн лй шлйбйн щерйн тщеййн мфвет борврерй ддъфъзеъ щм ъай вжт сширййн еблк мдееъ асишивйд обийзд мийфем бсшип длбг. бсчйшд офешийн дооцайн оозчшйн чмйрййн, ебтйчш оозчшйн фшд-чмйрййн, бревт мдщфтд щм шлйбйн ибтййн ецозй ошфа, бйрйдн шжбшишем, сймйбйрйп [шлйб фтйм бвгймп оцей (Silybum marianum)], шлйб ресу деа Phytol (шлйб блмешефйм), щещ чйшз (Glycyrrhiza glabra), шлйб фтйм бчтшешйъ сйрйъ (Scutellaria baicalensis) деа Baicalein, щоп вшйсй фрйрд (Coix). бресу офешийн дооцайн бдъййзс мосфш фешоемеъ цозй ошфа, бйрйдп PHY906 долймд аъ дцозйн дбайн: Scutellaria baicalensis, Glycyrrhiza uralensis, Paeonia lactiflora, Ziziphus jujube.
дзечшйн ослойн лй йщ цешк бозчшйн чмйрййн лфемй сойеъ еобечшй фмсбе тм оръ мдтшйк аъ дйтймеъ щм цозй ошфа еоецшйн ибтййн бщймеб тн дийфем дчербрцйермй.
https://www.ncbi.nlm.nih.gov/pubmed/26879574
бсчйшд (2016) оецвйн дооцайн дфшд-чмйрййн бревт мшлйбйн ибтййн, ащш тщеййн мъшен мийфем бвйгемй оез осев вмйеод, бйрйдн лешлеойп, PEITC (дйгет л-Phenethylisothiocyanate) доцей бйшчеъ оцмйбйн, Aloe Emodin [доефч одцоз амеешд (Aloe vera)] , е- Dioscin доефч обииъ бш ( Dioscorea villosa), шжбшишем, чеешцийп, бшбшйп етег.
https://www.ncbi.nlm.nih.gov/pubmed/26791479
бсчйшд (фбшеаш 2017) безрйн дзечшйн одп дтгейеъ дтглрйеъ мйтймеъ ийфемйн ибтййн ббзймеъ едчаеъ бчшб ймгйн дтебшйн лйоеъшфйд. бсчйшд рлмме 21 озчшйн (ашбтд одн озчшйн ачшаййн обечшйн), щртшле бчшб ймгйн ае обевшйн земй сшип. бозчшйн дщерйн ртщд щйоещ бгйчеш сйрй, ашеоъшфйд, цозй ошфа, дйфрежд едътшбейеъ чеврйийбйеъ-дърдвеъйеъ. бдъййзс машеоъшфйд, йщрн ооцайн обийзйн бревт мйтймеъ щм шйз ъфеж, дп одфшй тцое едп лщоп аъшй. бдъййзс мцозй ошфа, йщрп тгейеъ отешбеъ бревт мйтймеъ щм в'йрв'ш (Zingiber officinale), лащш бозчш ачшай обечш вгем роцад йтймеъ мойреп йеой щм 0.5-1 вшн мдчмд тм бзймеъ лъецад олйоеъшфйд бчшб обевшйн. тег роцад ъойлд мщйоещ блоесеъ ртрт зшйфд (Mentha piperita) еорид (Mentha spicata) мдчмд тм бзймеъ бчшб обевшйн дтебшйн лйоеъшфйд.
дзечшйн оцййрйн лй тм бсйс дтгейеъ дчййоеъ ма рйъп мдсйч тм дйтймеъ едбийзеъ щм ошбйъ дийфемйн тбеш ймгйн. тн жаъ, йщрн ооцайн доцбйтйн тм йтймеъ осейоъ тбеш обевшйн ергшщйн озчшйн ресфйн тм оръ мбзеп одй дйтймеъ едбийзеъ бдъййзс мийфем бймгйн.
https://www.ncbi.nlm.nih.gov/pubmed/28193133
бсчйшд (аечиебш 2016) оецвйн цозй дошфа дощощйн бшфеад ддегйъ досешъйъ мщойшд тм фешйеъ двбш едгзу дойрй, мийфем бозмеъ лшерйеъ еморйтд щм озмеъ ойп есшип ботшлъ дшбййд. дцозйн доежлшйн бсчйшд леммйн: ейърйд ощлшъ (Withania somnifera), чиб оцей (Tribulus terrestris), асфшвес дегй (Asparagus racemosus), рйн (Azadirachta indica), шйзп чгещ (Ocimum sanctum) ев'йрв'ш (Zingiber officinale).
https://www.ncbi.nlm.nih.gov/pubmed/27681646
счйшд (ребобш 2015) доцйвд аъ дтгейеъ дозчшйеъ бревт мдщфтд щм овееп вгем щм шлйбйн ибтййн ецозййн лрвг ъай вжт сширййн. чййоъ вйщд мфйд дочеш мвйгем сширй деа бчбецд чирд щм ъайн тн оафййрйн щм ъай вжт еорврерйн щм дйщшгеъ едъзгщеъ елъецад олк ъайн амд тойгйн бфрй ошбйъ дъшефеъ длйоеъшфйеъ. озчшйн щерйн оцбйтйн тм лк щшлйбйн ибтййн щерйн тщеййн мдщфйт тм осмемйн дотешбйн ббйией дврий щм ъайн амд еблк осфчйн ъойлд мчщш бйп ъжерд одцеоз мбйп дфзъъ щйтеш дооайшейеъ. бсчйшд офешийн дооцайн мвбй шлйбйн шбйн, бйрйдн смйреойцйп, семфешафп, айжефмберйн осейд, EGCG (ъд йшеч), шлйбйн саферйрйн, чеешцийп, лешлеойп, фемйфреЙмйн лое в'йрв'шем етег.
http://www.ncbi.nlm.nih.gov/pubmed/26503998
счйшд (йреаш 2015) дтесчъ бфтймеъ дарий-сширйъ щм йшчеъ одсев дбеирй Allium, бгвщ тм щен (Allium cepa) ебцм, ебдщфтд щм дшлйбйн двефшъййн доцеййн бйшчеъ амд. озчшйн афйгойемевййн оцбйтйн тм чщш бйп цшйлъ йшчеъ оощфзъ дщен мбйп сйлеп роек йеъш мсшип, ебойезг сшип ботшлъ дтйлем. оозчшй отбгд темд лй дшлйбйн двефшъййн ощфйтйн тм дфтймеъ дчшцйреврйъ, дфтймеъ дарий-ойчшебйамйъ етм ъдмйлй дзоцеп бъайн. бресу роца лй йшчеъ лое щен ебцм ешлйбйдн дфтймйн дйрн бтмй дщфтд ъдмйлйн бйемевййн щерйн етм лм щмбй дъдмйк дсширй елъецад олк тщеййн мдщфйт тм дсйлеп мсшип.
http://www.ncbi.nlm.nih.gov/pubmed/25586902
счйшд (ошх 2015) щретгд мдтшйк аъ дтгейеъ мвбй дщйоещ бъесфй ъжерд ецозйн дрйимйн баефп феой бчшб земеъ сшип дщг. дзечшйн бзре аъ дъшеод щм ъесфйн ибтййн мдчмд тм ъсойрй дозмд еъефтеъ дмееай щм дийфем, мщйфеш айлеъ дзййн, мщйфеш дбшйаеъ двефрйъ едшвщйъ емщйфеш щйтеш ддйщшгеъ едъоеъд. бсчйшд рлмме 22 озчшйн досфчйн ъойлд мщйоещ бвеашрд (Paullinia cupana) ебфишййъ шййщй (Ganoderma lucidum) мдчмд тм ъщйщеъ ебвмеиойп мщйфеш оечежйийс бфд.
баефп лммй, дтгейеъ дйрп оевбмеъ еайрп оафщшеъ мвбщ домцеъ чмйрйеъ бшешеъ мвбй дйтймеъ едбийзеъ щм ъесфйн щерйн мземеъ сшип дщг.
http://www.ncbi.nlm.nih.gov/pubmed/25811312
счйшд (фбшеаш 2016) доцйвд аъ дтгейеъ бйзс мйтймеъ щм овееп шлйбйн цозййн морйтд еийфем бомреод. дсчйшд оъочгъ бфмберем дрчша fisetin, EGCG, шжбшишем, лешлеойп, фшеаръецйарйгйрйн, сймйошйп, афйврйп, чфсайцйп, врйсиайп, айргем-3-чшбйрем емеиаемйп.
http://www.ncbi.nlm.nih.gov/pubmed/26864554
счйшд (йемй 2015) доцйвд аъ дтгейеъ дозчшйеъ дтглрйеъ бревт мфйиелйойчмйн ащш фетмйн лрвг ъай вжт сширййн. дзечшйн офшийн одн дорврерйн доемчемшййн бдн ъай двжт дсширййн оъзгщйн елйцг фйиелйойчмйн щерйн февтйн бъдмйлйн амд еолап дщфМтън дарий-сширйъ. дшлйбйн дцозййн дтйчшййн щроцае йтймйн леммйн EGCG, лешлеойп, фйфшйп, семфешафп, биа-чшеип, в'рйсиайп, чеешцийп ешжбшишем. дзечшйн осбйшйн лй лйен даъвш двгем дйре щймеб дшлйб дбегг йзг тн шлйбйн ресфйн боишд мйцеш ийфем арий-сширй зжч ейтйм.
http://www.ncbi.nlm.nih.gov/pubmed/26184171
счйшд (йерй 2015) доцйвд аъ дтгейеъ бйзс мфтймеъ дарий-сширйъ щм фймриес (Phyllanthus emblica), орврерй дфтемд дафщшййн елйеерй озчш тъйгййн дргшщйн мййщен чмйрй щм дооцайн.
http://www.ncbi.nlm.nih.gov/pubmed/26180601
счйшд (ребобш 2015) ащш ослоъ аъ дооцайн мвбй дфтймеъ дарий-сширйъ щм 6 шлйбйн цозййн щочешн бцозйн алймйн ема-алймйн. дшлйбйн дофешийн бсчйшд леммйн: шлйб rottlerin доефч одтх Mallotus philippensis; шлйб berbamine доефч ожрйн щерйн щм дцоз бшбшйс (Berberis); шлйб sparstolonin B доефч одцоз Sparganium stoloniferum; шлйб sulforaphane (семфешафп) доцей бйшчеъ оцмйбйн; шлйб plumbagin доефч одцоз Plumbago zeylanica ешлйб (6)-shogaol доцей бв'йрв'ш (Zingiber officinale). дзечшйн осбйшйн аъ орврерй дфтймеъ дчщешйн бдщфтд дарий-сширйъ щм лм шлйб. дн ослойн лй шлйбйн амд тщеййн мдееъ бсйс мфйъез ъшефеъ згщрйеъ мийфем бсшип. лое лп, шлйбйн амд тщеййн мдвбйш аъ йтймеъ дийфем дчербрцйерамй еморет дйщреъ щм двйгем еблк мщфш аъ ъецаеъ дийфем.
http://www.ncbi.nlm.nih.gov/pubmed/26695359
счйшд (аечиебш 2015) дтесчъ бъшеод щм чрабйс шфеай мдчмд тм лаб.
босвшъ дсчйшд офшийн дзечшйн аъ севй дчрабйреайгйн едчемирйн щмдн еаъ дооцайн дтесчйн бдщфтд дачеийъ едлшерйъ щм ошйзеард. бдощк дн оцйвйн озчшйн ачшаййн обечшйн бдн рбгчд дйтймеъ щм чрабйс мдчмд тм лаб бземй сшип, лаб рейшефий, лаб ачеий елаб лшерй. дн ослойн лй мошеъ дщйоещ дрфех бчрабйс бъшбейеъ щереъ, дозчш дчмйрй мвбй йтймеъе дйре оцеоцн. йщрд ъойлд шзбд йзсйъ мщйоещ бчрабйс мдчмд тм лаб бземй сшип, лащш ойрерйн вбедйн тмемйн мвшен мъефтеъ мееай. йщрн вн ооцайн зйебййн бйзс мдчмд тм лаб рейшефий бсебмйн оаййгс, ишщъ рфецд ае феси-ишаеод.одсчйшд темд лй чрабйс айре оебйм мщйфеш, ае мщйфеш чм, боцбйн щм лаб ачеий есфсийеъ; дооцайн обийзйн йеъш бйзс мщйфеш блаб лшерй. дзечшйн оцййрйн лй йщ мдощйк ембзеп лйцг мдфзйъ ъефтеъ мееай, лвеп рорен, сзшзешъ, йебщ бфд еглгек.
http://www.ncbi.nlm.nih.gov/pubmed/26325482
счйшд (гцобш 2015) доцйвд аъ дщйоещ босфш шлйбйн цозййн доелшйн басйд мийфем еорйтд щм сшип ботшлъ дтйлем, лемм в'йрсрв чешйарй (Panax ginseng), лешлеойп, ъд щзеш, ъд йшеч (Camellia sinensis), в'рйсийап доцей биефе, дшлйбйн дфтймйн бщен (Allium sativum), чфсайцйп, в'йрв'шем есймйошйп.
http://www.ncbi.nlm.nih.gov/pubmed/26651248
счйшд (аечиебш 2015) ащш ретгд мбзеп дан дщйоещ бцозй ошфа бтмй фтймеъ арий-гмчъйъ тщей мдйеъ йтйм морйтд ае тйлеб дъфъзеъ щм ооайшеъ блбг (чшцйреод щм длбг - HCC).
дзечшйн осбйшйн лй йщрп тгейеъ доцбйтеъ тм лк щоцб гмчъй лшерй чщеш бдъфъзеъ щм ооайшейеъ осевйн щерйн ботшлъ дтйлем елп лй шоеъ вбедеъ щм даржйн ALT чщешеъ бсйлеп вбед йеъш м-HCC. отбш млк, боцб щм гмчъ лшерйъ цфей лй йземе щйреййн вриййн баефп одйш йеъш еддъфъзеъ щм вйгемйн тмемд мдйеъ оеацъ лащш шоеъ ALT вбедеъ баефп лшерй. олап, мцозй ошфа бтмй фтймеъ арий-гмчъйъ тщейд мдйеъ дщфтд ойийбд тм дъфъзеъ HCC. бсчйшд офешиеъ дтгейеъ мвбй дщйоещ босфш фешоемеъ цозйеъ доелшеъ бйфп: Sho-saiko-to, Juzen-taiho-to, SNMC елп шлйбйн доефчйн одцоз чтшешйъ сйрйъ (Scutellaria baicalensis) ев'йрсресйгйн доефчйн оцоз дв'йрсрв. дзечшйн ослойн лй цозй дошфа доелшйн мийфем бдфштеъ блбг дйрн бтмй дщфтд арий-гмчъйъ оелзъ аемн йщ мдощйк ембзеп аъ йтймеън морйтд ае тйлеб дъфъзеъ HCC.
http://www.ncbi.nlm.nih.gov/pubmed/26457019
бсчйшд (фбшеаш 2016) оцйвйн дзечшйн аъ дооцайн дтглрййн мвбй дфтймеъ дарий-сширйъ щм цозй ошфа, шлйбйн фтймйн езмчйчй оълеъ (лсу, ждб, абх аечсйг, бшжм аечсйг, рзещъ аечсйг еамеойрйен аечсйг), доефчйн ошлйбйн цозййн баоцтеъ щйоещщ брреилремевйд.
https://www.ncbi.nlm.nih.gov/pubmed/27057273
бсчйшд (аевеси 2016) офешийн дооцайн дтглрййн оозчшйн фшд-чмйрййн бревт мжойреъ дбйемевйъ еморврерй дфтемд дчщешйн бфтймеъ дарий-сширйъ щм ойцей тмй жйъ (Olea europea).
дзечшйн осбйшйн лй бдщееад мщоп жйъ доефч одфшй, тмй джйъ олймйн лоеъ вгемд еовееръ йеъш щм фемйфреЙмйн, щдйрн вн бтмй дбгмйн обрййн одфемйфреЙмйн доцеййн бфшй, еблк тщеййн мдйеъ бтмй дщфтд бшйаеъйъ вгемд йеъш. боегмйн щм ъдмйлйн гмчъййн есширййн роца лй фемйфреЙмйн доцеййн бтмй жйъ дйрн бтмй дщфтд арий-гмчъйъ едщфтд овйрд офрй ржчйн зоцерййн м-DNA. дщфМтън дотлбъ тм ъдмйлйн сширййн чщешд босфш осмемйн, бйрйдн NF-κB еосмем дтчд дзоцерйъ, ак вн бфтймеън дфйиеасишеврйъ. дщфМтъ дфемйфреЙмйн тм чемирй дасишевп тщейд мъшен мдфзъъ дсйлеп мсевй сшип тм шчт дешоермй елп мтйлеб дъчгоеъ двйгем.
https://www.ncbi.nlm.nih.gov/pubmed/27548217
счйшд доъашъ аъ дъшеод щм дшфеад дчешйарйъ досешъйъ мшфеад доегшрйъ, ебойезг мийфем бозмъ дсшип, лйееп щоцйтд ийфем шб ъзеой длемм щйреййн баешз дзййн, щйоещ бфешоемеъ цозй ошфа, гйчеш, оечсд, фтймеъ вефрйъ осешъйъ еогйицйд тм оръ мдзжйш аъ дайжеп бйп двеу, дрфщ едшез.
https://www.ncbi.nlm.nih.gov/pubmed/24282099
бозчш фйймеи обечш (2022) рбгчд ддщфтд щм чеофшсйн щм алймад (Achillea millefolium) тм отшлъ дтцбйн даеиереойъ, бчшб земй сшип вшешъй ащш очбмйн ийфемй чшйрд есебмйн отййфеъ. бозчш рлмме 39 оиефмйн ащш земче ачшайъ мчбецъ ддътшбеъ щиефмд бчеофшсйн ае мчбецъ дбйчешъ щма чйбмд лм дътшбеъ зйцерйъ мощк щбетййн. дщЙАфтъ ддътшбеъ детшлд баоцтеъ дддщъреъ бчцб дмб, логг мъфчег отшлъ дтцбйн даеиереойъ, щроггд бъзймъ дозчш ебсйеое, бйен ебмймд. роца лй бчбецъ ддътшбеъ змд йшйгд бдщъреъ чцб дмб бодмк дйен доцбйтд тм тмййд бфтймеъ дсйофъийъ, мтеоъ тмййд бчбецъ дбйчешъ доцбйтд тм тмййд бфтймеъ дфаша-сйофъийъ. ма роцае дбгмйн оебдчйн бдщъреъ чцб дмб бодмк дмймд. дзечшйн ослойн лй тмййд бфтймеъ дсйофъийъ бодмк дйен тщейд мъоек бщйфеш ъсойрй тййфеъ бчшб земй сшип.
https://pubmed.ncbi.nlm.nih.gov/35430924/
озчш зък ъйаешй (ребобш-гцобш 2015) бе рбгч щйтеш еоафййрй дощъощйн бъесфйн цозййн бчшб земй сшип дтебшйн ийфемй лйоеъшфйд. дръерйн обессйн тм щамеп щдетбш м-397 оиефмйн бошфаеъ зех ббйъ земйн биешчйд. обйп лмм дощъъфйн, м- 28% дйсиешйд ощфзъйъ щм сшип, 22% сбме осшип бгшлй дтйлем е-22% осшип дщг еошбйъ дощъъфйн (92%) дйе бтмй ъфйсеъ гъйеъ еъшбеъйеъ.
роца лй 34% одощъъфйн тще щйоещ бъесфй ъжерд ае цозйн бресу мийфем дшфеай, лащш дшлйбйн дтйчшййн бдн ртщд щйоещ леммйн сшфг- Urtica dioica (л-22% одощъъфйн), фшзй щеош- Foeniculum vulgare (л- 20% одощъъфйн) еоецшйн цозййн ресфйн ащш фешсое блмй дъчщешъ (10%).
тег роца лй 52% одощъощйн бшфеад ощмйод дйе тчшеъ бйъ е-38% дйе тн дйсиешйд ощфзъйъ щм сшип.
дзечшйн ослойн лй дщйоещ бъесфйн цозййн дйре щлйз биешчйд аемн олйееп щзмч вгем одоецшйн дцозййн тмемйн мвшен мдщфтеъ щайрп шцейеъ, тм доифмйн мдлйш дйиб оецшйн амд емййгт аъ доиефмйн мвбй дйъшереъ ае дсйлерйн дафщшййн.
http://www.ncbi.nlm.nih.gov/pubmed/26465625
бозчш очшд-бчшд (2016), щртшк баешевеай, роца лй цшйлд вбедд щм ъд оаид (Yerba mate) дййъд чщешд бсйлеп роек щм тг 60% мсшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/27039789
озчш ощеъу мзечшйн йщшамййн емзечшйн оогйреъ дожшз дъйлеп (ребобш 2015) тесч бсйлерйн дафщшййн дчщешйн бщйоещ бшфеаъ цозйн осешъйъ босвшъ дийфем бземй сшип.
дзечшйн бгче аъ дщйоещ бцозй ошфа бдъан мгйеез доифм даерчемевй едтшйле аъ дсйлерйн лъецад ощйоещ жд. мщн лк, оифмйн аерчемевййн б-16 огйреъ божшз дъйлеп дъбчще мома щамеп бе дъбчще мдтшйк оецшйн цозййн бдн оиефмйдн тещйн щйоещ. баоцтеъ отрд щм 339 оифмйн (80.3%), жеде 44 ъесфйн цозййн е-3 шлйбйн щайрн цозййн, лащш дцозйн дщлйзйн бйеъш дйе сшфг (Urtica dioica), щен (Allium sativum), чцз (Nigella sativa) елешлен (Curcuma longa) елп шлйбйн лое змб рачеъ егбщ.
осчйшъ дсфшеъ огеезйн дзечшйн лй щйоещ б-29 одоецшйн тмем мдйеъ омеед бсйлерйн щерйн.
баефп сфцйфй, бдъййзс м-15 цозй ошфа роцае сйлерйн дчщешйн бъвебд дггйъ бйп дийфем дцозй едъшефъй, бтйчш бщм дщАфтън тм аржйой цйиелшеДДЙн P450. цозй ошфа аме леммйн: Allium sativum, Camellia sinensis, Curcuma longa, Foeniculum vulgare, Ginkgo biloba, Hypericum perforatum, Matricaria recutita (chamomilla), Melissa officinalis, Mentha piperita, Panax ginseng, Polygonum, Silybum marianum, Thymus vulgaris, Trifolium pratense, Vitis vinifera.
18 цозй ошфа тмемйн мвшен мштймеъ баефп йщйш, бтйчш тм йгй двбшъ дсйлеп мгйоен ефвйтд бфтймеъ дисйеъ: Allium sativum, Camellia sinensis, Cuminum cyminum, Curcuma longa, Ferula asafetida, Foeniculum vulgare, Ginkgo biloba, Hippophaerhamnoides, Linum usitatissimum, Nerium oleander, Nigella sativa, Olea europaea, Panax ginseng, Thymus vulgaris, Trifolium pratense, Trigonella foenum-graecum, Vitis vinifera, Zingiber officinale.
е-7 цозй ошфа тмемйн мдщфйт тм йтймеъ длйоеъшфйд: Curcuma longa, Ganoderma lucidum, Linum usitatissimum, Nigella sativa, Panax ginseng, Silybum marianum, Viscum album.
бщм сйлерйн ощотеъййн амд, чешайн дзечшйн моифмйн аерчемевййн мдбрд шзбд еотойчд йеъш щм дщйоещ бцозй ошфа лащш щймеб щм оифмйн айрившийбййн тн длщшд ййтегйъ тщей мъшен дп мземйн едп моифмйн даерчемевййн емсййт бчбмъ дзмиеъ оещлмъ бйзс мйтймеъ едбийзеъ щм дщйоещ бцозй ошфа.
дтшъ дотшлъ: мазш чшйад йсегйъ щм доаош, ршад лй ошбйъ ддомцеъ дребтеъ ооре обессеъ тм дрзеъ ъйаешийеъ, еайрп овебеъ бшайеъ чмйрйеъ. йзг тн жаъ, тчб зщйбеъе щм дреща, лгай бдзми мрдев ждйшеъ бочеоеъ бдн щешд ай еегаеъ.
змч вгем одръерйн еодаждшеъ догеезйн боаош лбш оцей боеревшфйн дшмеериййн байргчс дцозйн щмре. аре оощйлйн мтбг аъ дръерйн ащш фешие боаош, ебойгъ дцешк ртглп аъ доеревшфйн дшмеериййн бдъан.
http://www.ncbi.nlm.nih.gov/pubmed/26599199
озчш (гцобш 2014) щретг мдтшйк аъ дщйоещ дзйцерй боецш (Holoil®) долйм ойцей фшт озешш (Hypericum perforatum) ещоп рйн (Azadirachta indica) мийфем бфвйтд тешйъ лъецад оийфемй лйоеъшфйд ечшйрд бземй сшип шащ ецееаш.
бозчш дщъъфе 28 земйн ащш дъзйме аъ дийфем ойг тн дефтъ фвйтд тешйъ (дагод щм дтеш, бцчъ ае чщчщъ) бощк лм озжешй дийфем ебъчефъ дотчб тг мдзмод.
дощъъфйн бозчш сбме офвйтд тешйъ бшоеъ щереъ едйе дбгмйн бощк ддзмод, ак ма геез тм щйоещ бъшефеъ ресфеъ мдчмд тм дфвйтд отбш мийфем дцозй.
дзечшйн ослойн лй щйоещ бфшт озешш ещоп рйн тщей мдйеъ йтйм ебиез мийфем бфвйтд тешйъ бчшб земй сшип шащ ецееаш.
http://www.ncbi.nlm.nih.gov/pubmed/25544371
бозчш (2015), бе ртщд щйоещ бвйщд илремевйъ згщрйъ дрчшаъ Network pharmacology, бзре дзечшйн аъ ддщфтеъ дщереъ щм дфешоемд дайеешеегйъ "Triphala", бдъбсс тм ойгт оосфш оавшй ръерйн щерйн, боишд мфъз лйеерйн згщрййн мийфем бозмеъ щереъ, бгвщ тм озмъ дсшип.
https://www.ncbi.nlm.nih.gov/pubmed/26477351
оаош (йерй 2015) доъаш брййъ оавш ойгт ооезщб щм шлйбйн цозййн бтмй фтймеъ арий-сширйъ.
дзечшйн осбйшйн лй дооцайн мвбй шлйбйн цозййн еддщфтд дбйемевйъ щмдн дйрн очеш мфйъез ъшефеъ згщрйеъ еийфемйн лрвг севй сшип щерйн. аемн, долщем дтйчшй дйре дтгш ойгт мвбй ддщфтд дфшочемевйъ щм ошбйъ шлйбйн амд.
лйен оавш дойгт лемм 2,439 ийфемйн цозййн арий-сширййн е-3,575 шлйбйн арий-сширййн лащш тбеш лм шлйб йщре фйшеи щм добрд доемчемшй ещм дфтймеъ дфшочемевйъ (сфйвд, фйжеш, оибемйжн едфшщд).
бресу йщре фйшеи дфтймеъ дарий-сширйъ бдъбсс тм 492 щешеъ ъайн щереъ ещм змберй доишд щм шлйбйн амд бдъбсс тм илремевйеъ оъчгоеъ ае тм дгйеезйн бсфшеъ дозчшйъ.
айсеу ешйлеж дойгт тщей мъшен мщйфеш едацъ ъдмйлй дфйъез щм ийфемйн згщрййн едшзбъ дозчш аегеъ шлйбйн цозййн бтмй дщфтд арий-сширйъ.
http://www.ncbi.nlm.nih.gov/pubmed/26074488
оаош (йерй 2015) доцйв вйщеъ тглрйеъ мдфзъъ доемйжд бтчбеъ ийфем ъшефъй, бтйчш лйоеъшфйд, лемм дщйоещ бшлйбйн цозййн.
http://www.ncbi.nlm.nih.gov/pubmed/26047758
бозчш отбгд (2021) дегвод дфтймеъ ревгъ дсшип щм ойцей фим лрвг ъай сшип цееаш дшзн, ъек бгйчъ орврерй дфтемд дотешбйн.
https://pubmed.ncbi.nlm.nih.gov/34230130/
бозчш отбгд (2021) безрйн дзечшйн аъ орврерй дфтемд ревгй дсшип щм EGCG, еошайн лй м EGCG йщ дщфтд тм дзмбеп p53 дотешб бъйчеп ржчйн м-DNA етйгег дъоеъд щм ъайн сширййн.
https://pubmed.ncbi.nlm.nih.gov/33579943/
озчш щртшк тм зйеъ отбгд (гцобш 2014) ошад лй дфтймеъ ревгъ дзоцеп щм тмй оешйрвд дйрд бтмъ дщфтд овйрд тм щмфезйъ дщъп офрй штймеъ лъецад ощйоещ бъшефд длйоеъшфйъ Cyclophosphamide.
http://www.ncbi.nlm.nih.gov/pubmed/25595312
бозчш отбгд (2018) огвйойн дзечшйн аъ дфтймеъ ревгъ дсшип щм ойцей щен (Allium sativum) ишй, лемм двбшъ йтймеъ дийфем ревг дсшип едщфтд тм осфш вгем щм змберйн, дотешбйн бъчщешъ ъайъ ебъдмйлй дфшемйфшцйд едафефиежйс щм дъайн дсширййн.
https://www.ncbi.nlm.nih.gov/pubmed/29621132
озчш отбгд (фбшеаш 2015) доцбйт тм дйтймеъ щм ъесу цозй долйм чеешцийп, лешлеойп, ъд йшеч, ойцей йшчеъ оцмйбйн ешжбшишем мийфем бсшип шащ ецееаш бземй аройд т"щ фрчерй (озмд врийъ чщд доъбиаъ бзесш ъай гн).
http://www.ncbi.nlm.nih.gov/pubmed/25695860
озчш отбгд (афшйм 2015) ащш оцбйт тм орвреп дфтймеъ бе вйрче ъешн мдвбшъ дйтймеъ еморйтъ тойгеъ млйоеъшфйд бъай чйбд сширййн.
http://www.ncbi.nlm.nih.gov/pubmed/25962735
озчш отбгд (йемй 2014) бе жеде дшлйбйн дфтймйн бцоз араошрд щдйрн бтмй фтймеъ арий-сширйъ.
http://www.ncbi.nlm.nih.gov/pubmed/25005066
озчш отбгд (фбшеаш 2015) доцбйт тм орврерй дфтймеъ щм ойх омеп ош мщйфеш дтойгеъ млйоеъшфйд осев gemcitabine бземй сшип мбмб.
http://www.ncbi.nlm.nih.gov/pubmed/25672620
озчш отбгд (йерй 2015) доцбйт тм дйтймеъ щм дшлйб дцозй бшбшйп мдвбшъ дщфМтъ длйоеъшфйд лрвг ъай сшип дщзмеъ.
http://www.ncbi.nlm.nih.gov/pubmed/26087719
озчш отбгд (ошх 2015) бе рбгче дорврерйн дтеогйн ббсйс дфтймеъ дарий-сширйъ щм ойцей оййой щм чйсесйъ (Smilax Glabra).
http://www.ncbi.nlm.nih.gov/pubmed/25732255
озчш отбгд (йемй 2015) доцбйт тм дфтймеъ щм ойцей шежошйп лрвг ъай омреод арещййн.
http://www.ncbi.nlm.nih.gov/pubmed/26176704
озчш отбгд (йемй 2015) доцбйт тм дорврерйн доемчемшййн дтеогйн ббсйс ддщфтд дарий-сширйъ щм ацд зеод лрвг ъай сшип дмбмб.
http://www.ncbi.nlm.nih.gov/pubmed/26204945
озчш отбгд (йемй 2015) бе рбгч ддшлб длйой едфтймеъ дарий-сширйъ щм ойцей тмй жйъ (Olea europaea) лрвг ъай сшип дмбмб.
http://www.ncbi.nlm.nih.gov/pubmed/26193251
озчш отбгд (2015) доцбйт тм дфтймеъ дарий-сширйъ щм ойцей омйсд (Melissa officinalis) лрвг ъай сшип дшйаеъ, сшип дщг, сшип дщзмеъ есшип дтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/26320439
озчш отбгд (2015) дтесч бдщфтд дарий-сширйъ лрвг ъай сшип лмйеъ щм ъесу айешеегй (CRUEL) долйм цозй ошфа еойршмйн. дцозйн доелшйн мре бфешоемд же дн фмфм щзеш (Piper Nigrum), мйчешйх (Glycyrrhiza glabra), оешйрвд (Moringa Oleifera) ешйзп чгещ (Ocimum sanctum).
https://www.ncbi.nlm.nih.gov/pubmed/26745095
бозчш щртшк тм зйеъ отбгд (ребобш 2015) ма роцад дщфтд мриймъ ойцей ъмъп аген (Trifolium pratense) тм йтймеъ дийфем дъшефъй биоечсйфп. ооцайн амд аещще вн бозчш щртшк тм ъай лбг арещййн.
https://www.ncbi.nlm.nih.gov/pubmed/26530625
бозчш отбгд огвйойн дзечшйн аъ дфтймеъ ревгъ дсшип щм ойцей оййой щм тмй оешйрвд (Moringa oleifera) лрвг ъай сшип дещи.
https://www.ncbi.nlm.nih.gov/pubmed/27074620
бозчш отбгд (фбшеаш 2017), щртшк тм йгй зечшйн йщшамййн, рбгчд дштймеъ едъвебд ддггйъ тн ъшефеъ щм осфш цозй ошфа щлйзйн, бдн ртщд щйоещ бчшб земеъ сшип дтебшеъ ийфемй лйоеъшфйд.
шащйъ, дзечшйн асфе ръерйн аегеъ дщйоещ бцозй ошфа бчшб рщйн тн сшип врйчемевй, щдефре мщйшеъй шфеад ощмйод. обйп 98 рщйн, 42 гйеезе тм щйоещ ае леерд мдщъощ бцозй ошфа бодмк ийфемй длйоеъшфйд. тм бсйс ръерйн амд, дзечшйн бзше зойщд цозй ошфа бтмй шмеерийеъ чмйрйъ: тщб зйид (Triticum aestivum), гбчеп мбп (Viscum album), в'йрв'ш (Zingiber officinale), щшбйип оцей (Ephedra campylopoda) егбчеп джйъ (Viscum cruciatum). дщфМтъ цозйн амд рбгчд лрвг щешеъ ъай сшип щзмеъ дшвйщйн ае тойгйн мъшефд длйоеъшфйъ цйсфмаийп елрвг ъай лмйд бшйайн.
роца лй мгбчеп мбп емв'йрв'ш фтймеъ арий-сширйъ оебдчъ лрвг щъй щешеъ дъайн дсширййн. тщб зйид ещшбйип оцей дфзйъе аъ ддщфтд щм дъшефд длйоеъшфйъ чшбефмаийп, лмеош дфзйъе аъ йтймеъ дийфем, бъай сшип щзмеъ швйщйн мцйсфмаийп, бтег щв'йрв'ш, гбчеп мбп егбчеп джйъ ъшое мдвбшъ йтймеъ длйоеъшфйд бщъй щешеъ дъайн дсширййн. тщб зйид, гбчеп мбп ев'йрв'ш двбйше аъ йтймеъ дийфем бчшбефмаийп ебфчмйичсм бъай сшип щзмеъ швйщйн мцйсфмаийп. ма роцад дщфтд мау азг одцозйн тм ъай лмйд бшйайн.
дзечшйн ослойн лй мщйоещ бцозй ошфа тщейд мдйеъ дщфтд, зйебйъ ае щмймйъ, тм дъвебд млйоеъшфйд емлп чешайн маерчемевйн мдйеетх бшефа айрившийбй тм оръ мчбм дзмид оещлмъ еобессъ тгейеъ бжоп аоъ бдъййзс мйтймеъ ебийзеъ дщйоещ бцозй ошфа.
https://www.ncbi.nlm.nih.gov/pubmed/28238155
бсчйшд щм озчшй отбгд (аевеси 2016) ошайн дзечшйн лй ошеед сйрйъ (Salvia miltiorrhiza) тщейд мъшен мтйлеб ъай сшип баоцтеъ фтймеъ ревгъ зоцеп елп мтегг оееъ смчийбй щм ъайн сширййн баоцтеъ йцйшъ шгйчмйн зефщййн (ROS).
https://www.ncbi.nlm.nih.gov/pubmed/27579153
бозчш отбгд (ребобш 2016) рбгчд ддщфтд дарий-сширйъ щм ашбтд цозйн лрвг ъай омреод ооайшд арещййн. дцозйн чтшешйъ бшбид (Scutellaria barbata), мебмйд сйрйъ (Lobelia chinensis), семрен щзеш (Solanum nigrum) е-Hedyotis diffusa, дйрн цозйн щлйзйн бийфем дарий-сширй бшфеад дсйрйъ досешъйъ.
роца лй мойцей оййой щм семрен щзеш дщфтд арий-сширйъ оебдчъ лрвг ъай домреод (p<0.01) елй ддщфтд дарий-сширйъ щм Hedyotis diffusa ма дййъд оебдчъ сиийсийъ еййълп лй ргшщ шйлеж вбед йеъш щм дцоз мйцйшъ дщфтд. ма роцад дщфтд мцозйн чтшешйъ бшбид емебмйд сйрйъ. тег роца лй ойцей семрен щзеш дебйм мйшйгд бфтймеъ ревгъ дзоцеп еблк тщей мъшен мдщфтд дцйиеиечсйъ щроцад елп мдщфтд сйршвйсийъ лащш щемб тн дъшефд длйоеъшфйъ temozolomide.
https://www.ncbi.nlm.nih.gov/pubmed/27843296
бозчш отбгд (гцобш 2015) огвйойн дзечшйн аъ дфтймеъ дарий-сширйъ щм ойцей ъош сйрй (Ziziphus Jujube) лрвг ъай сшип цееаш дшзн.
https://www.ncbi.nlm.nih.gov/pubmed/26718441
бозчш отбгд (гцобш 2015) роца лй мшлйб дцозй бшбшйп дщфтд отлбъ тм дъфщиеъ ъай сшип деещи, бтйчш бщм дщфМтъе тм чемирй лйоечйрйн, дотешбйн бргйгъ ъайн едъфъзеъ вшешеъ.
https://www.ncbi.nlm.nih.gov/pubmed/26667771
бозчш отбгд (аечиебш 2016) роца лй ойцей оййой щм оачд (Lepidium meyenii) ма ъшн мфвйтд бъай сшип дтшоерйъ ема дщфйт тм йтймеъ дийфем дарий-сширй, аемн дебйм мдвбшъ дфтймеъ даргшеврйъ дчщешд бщйфеш дъфчег едзщч дойрй.
https://www.ncbi.nlm.nih.gov/pubmed/27681649
озчш отбгд (гцобш 2014) щретг мбзеп аъ дъшеод щм арв'мйчд сйрйъ мдврд офрй ржч лмййъй лъецад одщйоещ бъшефд длйоеъшфйъ цйсфмийп (cisplatin).
роца лй зщйфъ ъай лмйд мцйсфмийп дебймд мтмййд бщйтеш дъоеъд дъайъ (афефиежйс). тн жаъ, бъайн щрзщфе бочбйм вн мойцей арв'мйчд сйрйъ бойреп 50 оч"в мо"м зм щйфеш бщйтеш дъоеъд дъайъ. тег роца лй зщйфд мар'мйчд сйрйъ дебймд мщйфеш босфш оггйн дчщешйн бдврд тм ъай длмйд бъайн щрзщфе мцйсфмийп.
http://www.ncbi.nlm.nih.gov/pubmed/25495691
озчш щртшк тм зйеъ отбгд оцбйт тм дфтймеъ дарий-сширйъ щм ойцей асишвмес (Astragalus membranaceus) бойреп 500 о"в/ч"в лрвг ъайн щм сшип чемешчимй.
https://www.ncbi.nlm.nih.gov/pubmed/26719057
бозчш фйймеи ачшай обечш фъез (оай 2016), щртшк бщрй ошлжйн аерчемевйн биешчйд, рбгчд ддщфтд щм щийфъ фд цозйъ лийфем ъеок морйтъ оечежйийс бфд бчшб земй сшип дтебшйн лйоеъшфйд (5-фмеаешцйм).
бозчш дщъъфе 60 оиефмйн, ащш земче ачшайъ мчбецъ ддътшбеъ щчйбмд щийфъ фд цозйъ бресу мийфем дсиргший, ае мчбецъ дбйчешъ щчйбмд аъ дийфем дсиргший бмбг.
дийфем дсиргший лмм щийфъ дфд бъойсъ ой омз 4 фтойн бйен мощк 30 щрйеъ ецзцез щйрййн фтоййн бйен - одйен дшащеп мийфем длйоеъшфй емощк щбетййн. чбецъ ддътшбеъ дъбчщд мбцт щийфъ фд ресфъ, зцй щтд мазш сйен дийфем дсиргший, б-15 о"м оътшебъ долймд дйгшесемйн щм ошеед (Salvia officinalis) ийойп (Thymus vulgaris) еорид (Mentha piperita). дзечшйн дтшйле дъфъзеъ оечежйийс тм семн щм 0-4, тм фй ддвгшеъ щм ашвеп дбшйаеъ дтемой. дн оцййрйн лй мшеб оечежйийс оъфъз бъек 4-7 йойн оъзймъ дийфем длйоеъшфй емлп дтшйле аъ дщфМтъ дийфем мазш 5 йойн емазш 14 йойн.
роца лй бйен дзойщй 70% одощъъфйн бчбецъ ддътшбеъ ма сбме ооечежйийс (10% сбме ооечежйийс бшод 1 е-20% бшод 2), мтеоъ 40% бчбецъ дбйчешъ (53.3% сбме ооечежйийс бшод 1 е-6.7% бшод 2), p=0.001. бйен д-14 шеб дощъъфйн ма сбме ооечежйийс, мма дбгм оебдч бйп дчбецеъ (93.3% е-96.7%). ооцайн амд ъеолйн бйтймеъ щм щийфъ фд цозйъ морйтъ оечежйийс бчшб земй сшип доиефмйн блйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/27515877
ъйаеш очшд (йемй 2016) щм айщд бъ 85, ащш двйтд мбйъ земйн бсйп еаебзрд тн сшип шйаеъ бгшвд 4. дайщд ма чйбмд ийфем чербрцйерамй еиефмд бовееп вгем щм цозй ошфа сйрййн бощк 5 щрйн, бгвщ тм цозйн дойетгйн мзйжеч, лемм: чегерефсйс (Codonopsis pilosula), асишвмес (Astragalus membranaceus), аишчиймегс (Atractylodes macrocephala), фишйъ фешйд (Poria cocos), ецозйн дойетгйн мрйчей лемм чтшешйъ бшбид (Scutellaria barbata), ошеед сйрйъ (Salvia miltiorrhiza) ефшермд (Prunella vulgaris).
дзечшйн оцййрйн лй дийфем ъшн мщйфеш байлеъ дзййн щм доиефмъ, бдашлъ ощк ддйщшгеъ ебтйлеб дъфщиеъ двйгем, лащш бжоп лъйбъ доаош дайщд тгййп дййъд бзййн.
https://www.ncbi.nlm.nih.gov/pubmed/26597286
бсчйшд (2016) оъеашйн дорврерйн дчщешйн бсйргшен аебгп ъйабеп ейшйгд бощчм бземй сшип (Anorexia Cancer Cachexia Syndrome), бгвщ тм гмчъ отшлъйъ, едъшеод щм цозй ошфа дъешойн мдфзъъ дфтймеъ дгмчъйъ, двбшъ дфтймеъ дзйсерйъ, тйлеб фйшеч змбеп етйгег ъйабеп етмййд бощчм.
https://www.ncbi.nlm.nih.gov/pubmed/27758689
бозчш отбгд (йреаш 2017) огвйойн дзечшйн аъ дфтймеъ дарий-сширйъ щм ошеед шфеайъ (Salvia officinalis) еошеед сйрйъ (Salvia miltiorrhiza) лрвг ъай лбг сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/27930987
бозчш ачшай обечш (2016) рбгчд дйтймеъ щм в'йрв'ш (Zingiber officinale) мдчмд тм бзймеъ едчаеъ бчшб рщйн тн сшип щг дтебшеъ ийфемй лйоеъшфйд обессй гечсешебйцйп (doxorubicin). бозчш рлмме 150 оиефмеъ, ащш земче баефп ачшай мриймъ ъесу абчъ в'йрв'ш бойреп 500 о"в фтоййн бйен мощк 3 йойн, ае фмсбе.
дзечшйн дтшйле аъ шоъ дбзймд еддчаеъ тм семн щм 1-3 мазш лм сбб лйоеъшфйд мощк 3 сббйн. баефп лммй еблм азг одсббйн ма роца дбгм оебдч сиийсийъ бйп дчбецеъ бйзс мшоъ дбзймд. лое лп, мошеъ щроцад дчмд осейоъ бшоъ ддчаеъ бчшб оиефмеъ щриме в'йрв'ш, ма роцае дбгмйн оебдчйн сиийсийъ. йзг тн жаъ, обйп 85 дрщйн щчйбме дшлб лйоеъшфйд сфцйфй (doxorubicin60 mg/m2 + cyclophosphamid 600 mg/m2), роца лй риймъ в'йрв'ш дййъд омеед бшоъ дчаеъ роелд йеъш бдщееад мфмсбе (цйеп щм 0.64 мтеоъ 1.13, p<0.05). дзечшйн ослойн лй в'йрв'ш дйре ъесу биез моиефмй лйоеъшфйд, аемн йтймеъе мдчмд тм бзймеъ едчаеъ айрд зг-ощотйъ. ргшщйн озчшйн ресфйн тм оръ мвбщ осчрд обессъ, бгвщ тм озчшйн бдн цшйлъ дв'йрв'ш дйрд ооещлъ йеъш маешк лм одмк дийфем.
дтшъ дотшлъ: боаош ма офеши оъй рмчз дъесу бйзс мриймъ длйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/27644633
бозчш ъцфйъй (фбшеаш 2017) огеезйн дзечшйн лй тм бсйс дръерйн щрасфе о-50 земй сшип шащ ецееаш роца щдщйоещ бчшн цозй долйм фшт озешш (Hypericum perforatum) ещоп рйн (Azadirachta indica) дйре биез ейтйм мдфзъъ штймеъ тешйъ лъецад оийфемй чшйрд елйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/28101834
бозчш фшд-чмйрй (2016) оегвоъ ддщфтд дарий-сширйъ щм 3 жрй фишйеъ ошфа: фишййъ шййщй (Ganoderma lucidum), фишййъ щйиачй (Lentinus edodes) ефишййъ ойиачй (Grifola frondosa).
https://www.ncbi.nlm.nih.gov/pubmed/28008808
бозчш отбгд (фбшеаш 2017) роца лй фешоемд згщд дйрд бтмъ дщфтд арий-сширйъ еотеггъ афефиежйс (оееъ ъай) лрвг ъай мечойд. дфешоемд олймд 6 цозй ошфа: Rhus verniciflua, бечйцд (Ulmus rubra), фемйвериен (Polygonatum Sibiricum), вев'й бшй (Lycium chinense), фишййъ шййщй (Ganoderma lucidum) ев'йрсрв чешйарй (Panax ginseng).
https://www.ncbi.nlm.nih.gov/pubmed/27626609
бозчш, щртшк бчшб тлбшйн (2017), рзчшд ддщфтд щм осфш шлйбйн ибтййн боегм щм сшип дтшоерйъ. шащйъ тшле дзечшйн счйшъ сфшеъ шзбд боишд мждеъ одн дшлйбйн щтщеййн мдйеъ дйтймйн бйеъш. дн дощйле ббйцет бгйчеъ отбгд тм овееп вгем щм шлйбйн, лащш дшлйбйн щроцае добийзйн бйеъш дйе зеоцд аешсемйъ, лешлеойп ешжбшишем. баоцтеъ щйоещ боегм тлбшйн тн сшип дтшоерйъ, дзечшйн дтщйше аъ ъжеръ дтлбшйн бщмещъ шлйбйн амд ебгче лйцг цйшефйн щерйн щм аеън шлйбйн тщеййн мдщфйт тм двйгем дсширй.блм дцйшефйн щрбгче роцад дщфтд сйршвйсийъ тм вегм еощчм двйгем дсширй, лк щдщйоещ бшлйбйн дибтййн дебйм мдълеецеъ двйгем. дзечшйн ошайн лй ддщфтд дарий-сширйъ дййъд чщешд бдщфтд дсйршвйсийъ щм шлйбйн амд тм доибемйжн щм вмеиойп елп тм осмемй ъчщешъ ъайъ дотешбйн бдъфъзеъ дъдмйк дсширй (STAT3, mTORC1, AMPK). дн ослойн лй дщйоещ бвйщд озчшйъ же тщей мъшен мжйдей шлйбйн ибтййн дфетмйн баефп сйршвйсий лрвг дъфъзеъ едъчгоеъ ъдмйлйн сширййн.
https://www.nature.com/articles/s41698-017-0024-z
бозчш отбгд (2017) безрйн дзечшйн аъ ддшлб длйой щм ъйойп оджп Thymus alternans (двгм бсмебчйд) ешлйбйе дфтймйн, ъек дгвоъ ддщфтд дарий-фшемйфшийбйъ лрвг ъай сшип арещййн.
https://www.ncbi.nlm.nih.gov/pubmed/28222613
бозчш отбгд (аевеси 2016) роца лй фешоемъ цозй ошфа сйрйъ ъешоъ мтйлеб вгймъ ъай сшип дщг еовбйшд аъ ддщфтд дойийбд щм дийфем длйоеъшфй баоцтеъ ейсеъ даржйн Aurora A kinase, дотешб бъдмйлй змечъ дъа. дфешоемд, San Huang Decoction, рйъръ бцешъ ошъз, добесс тм дцозйн шйбс (Rheum spp) ечефийс (Coptis chinensis).
https://www.ncbi.nlm.nih.gov/pubmed/27461831
бозчш течбд обесс аелмесййд (афшйм 2016), щртшк биайееап, дъшеод щм щйоещ бшфеаъ цозйн сйрйъ лийфем ъеок бчшб земй мечойд ойамеайгйъ лшерйъ.
бдъбсс тм шйщеой бйиез дбшйаеъ дмаеой, дзечшйн жйде 466 земйн, щаебзре бйп дщрйн 2000-2010, ейцше щъй чбецеъ бтмеъ оафййрйн геойн: чбецд азъ щм земйн щтще щйоещ бшфеаъ цозйн сйрйъ ечбецд щрйд щчйбмд аъ дийфем дчербрцйерамй бмбг.
роца лй дсйлеп мъоеъд бчшб дощъъфйн щриме цозй ошфа дйд роек бл-70%, лащш чщш жд дйд ъмей ойреп лк щроца сйлеп роек йеъш тбеш щйоещ ооещк йеъш. цозй дошфа дбемийн щроцае йтймйн леммйн: ошеед сйрйъ (Salvia miltiorrhiza), асишвмес (Astragalus membranaceus), бииъ бш (Dioscorea villosa), шдорйд (Rehmannia glutinosa) ещещ чйшз (Glycyrrhiza glabra).
https://www.ncbi.nlm.nih.gov/pubmed/26773538
бсчйшд (2016) ослойн дзечшйн аъ дтгейеъ дтглрйеъ бревт мщймеб сйршвйсий щм шфеаъ цозйн мийфем бсшип. дзечшйн осбйшйн лй лйееп щсшип дйрд озмд оешлбъ, вн дийфем бд цшйк мдйеъ оешлб, лащш дщйоещ дочебм бъшефд азъ айре осфйч йтйм. мфйлк, щймеб сйршвйсий щм ъшефеъ щереъ, лфй щочебм бшфеаъ дцозйн дсйрйъ, дйре асишивйд обийзд мдвбшъ йтймеъ дийфем, мдфзъъ штймеъ емщйфеш дбийзеъ. босвшъ дсчйшд, оцйвйн дзечшйн щймебйн сйршвйсийн щм шлйбйн, дощощйн мийфем бсшип еъфчйгн бдвбшъ йтймеъ длйоеъшфйд, дфзъъ ъефтеъ дмееай щм дийфем, ейсеъ зйсерй едфзъъ тойгеъ мийфем. гевоаеъ мийфем ощемб, лфй щтемд бсчйшд: лешлеойп + шжбшишем, чеешцийп + EGCG, шжбшишем + врйсиайп елп щйоещ бфешоемеъ долймеъ осфш шлйбйн фтймйн ае осфш цозй ошфа лвеп чешйгмйъ (Corydalis ambigua), чтшешйъ сйрйъ (Scutellaria baicalensis), фишййъ шййщй (Ganoderma lucidum) етег.
https://www.ncbi.nlm.nih.gov/pubmed/26638885
бозчш отбгд (йреаш 2016) огвйойн дзечшйн лй мфемйфреЙмйн, доцеййн боемасд доефчъ осмч селш, фтймеъ арий-сширйъ лрвг ъайн арещййн щм сшип дотй, сшип длбг есшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/27347927
бсчйшд (аевси 2017) оецвеъ дтгейеъ бревт мфтймеъ дшфеайъ щм сийбйд (Stevia rebaudiana), лемм фтймеъ ревгъ зоцеп, арий-ойчшебйамйъ, ревгъ йъш мзх гн, ревгъ селшъ еревгъ сшип, бгвщ тм дъшеод мийфем боцбйн дчщешйн бъсоеръ доибемйъ.
https://www.ncbi.nlm.nih.gov/pubmed/28792778
бозчш отбгд (йерй 2016) роца лй ойцей тмй сшфг (Urtica spp) дйд бтм дщфтд отлбъ тм ъдмйлй фшемйфшцйд (щвщев) щм ъай сшип чемешчимй.
https://www.ncbi.nlm.nih.gov/pubmed/27090648
бозчш отбгд (оай 2017) огвйойн дзечшйн аъ фтймеъ ревгъ дсшип щм ойцей омйсд (Melissa officinalis) лрвг ъай сшип шйаеъ, щг етшоерйъ арещййн.
https://www.ncbi.nlm.nih.gov/pubmed/28259690
бсчйшд (ребобш 2017) оецвйн дооцайн оозчшйн фшд-чмйрййн ечмйрййн бревт мдщфтд дарий-сширйъ щм чрбйреайгйн еморврерй дфтемд щм шлйбйн щерйн, лащш дфтймеъ ревгъ-двйгем рбгчд чмйрйъ шч тм осфш чип щм оиефмйн ема рйъп мчбет осчрд зг-ощотйъ мвбй йтймеъ дийфем.
https://www.ncbi.nlm.nih.gov/pubmed/28799775
бсчйшд (йерй 2016) офешийн дооцайн бревт мдшлб длйой щм фмфмъ (Capsicum annuum) едщфМтън дойийбд щм дшлйбйн дщерйн тм ъдмйлй дтйлем етм дийфем бовееп дфштеъ лемм гйсффсйд, йшйгд бъйабеп, шфмечс, лйб чйбд есшип.
https://www.ncbi.nlm.nih.gov/pubmed/26756096
бсчйшд (ребобш 2017) оецвйн ооцайн оозчшйн фшд-чмйрййн бревт мдщфтд дойийбд щм тмй оешйрвд (Moringa Oleifera) бдъййзс мовееп озмеъ лшерйеъ, лемм озмеъ чшгйеесчемшйеъ, селшъ, сшип елбг щеорй.
https://www.ncbi.nlm.nih.gov/pubmed/29144438
бозчш отбгд (аевеси 2016) рзчше дорврерйн бдн чйроеп (Cinnamomum zeylanicum) ешлйбйе дфтймйн ъешойн мтйлеб ъай вжт тн мечойд, еблк осфч ъойлд озчшйъ мдщфтд дойийбд щм дфешоемд дсйрйъ досешъйъ Sanyangxuedai, долймд чйроеп, тбеш земй мечойд.
https://www.ncbi.nlm.nih.gov/pubmed/27706567
бсчйшд (сфиобш 2016) детшлд ддщфтд дарий-сширйъ щм чцз (Nigella sativa), бгвщ тм дъшеод щм дшлйб дфтйм thymoquinone мтйгег афефиежйс (оееъ ъай), мйшйгд бъретъйеъ емдфзъъ ъдмйлйн вшешъййн бъайн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/28476718
бозчш отбгд (аевеси 2016) роца лй шлйб оййой щдефч огчм ррсй (Serenoa repens) дйре бтм фтймеъ арий-сширйъ лрвг сшип длбг.
https://www.ncbi.nlm.nih.gov/pubmed/27527161
бозчш шишесфчийбй (фбшеаш 2017), щртшк бйщшам, детшлд дйтймеъ щм гйчеш ешфмчсемевйд мийфем брейшефъйд дйчфйъ лъецад олйоеъшфйд бчшб рщйн тн сшип дщг. дзечшйн оцййрйн лй рейшефъйд дйчфйъ дйрд ъефтъ мееай щлйзд оаег щм ийфемй лйоеъшфйд, щлйен айп мд ийфем йтйм. бозчш ртщд щйоещ бшщеоеъ дшфеайеъ щм 30 оиефмеъ, ащш чйбме ийфем ощемб бгйчеш ешфмчсемевйд бочбйм млйоеъшфйд бщм дефтъ ъсойрйн тцбййн. дийфем ртшк тм фй фшеиечем щфеъз бошлж мшфеад ощмйод еайрившийбйъ бошлж дшфеай ъм-абйб, елмм 1-2 офвщйн щбетййн щм гйчеш (20 гчеъ) ешфмчсемевйд (30-40 гчеъ). бооецт, доиефмеъ дзме аъ дийфем 105 йойн мазш дъзмъ длйоеъшфйд едщъъфе б-11 офвщйн бооецт. йтймеъ дийфем детшлд тм фй зеошъ ъсойрй дрейшефъйд бъзймъ ъчефъ дийфем, бодмлд ебсйеод. обйп 28 оиефмеъ тн шщеоеъ шфеайеъ омаеъ, 20 оиефмеъ сбме орейшефъйд срсешйъ, 7 орейшефъйд оеиешйъ е-1 орейшефъйд срсешйъ еоеиешйъ. обйп 20 доиефмеъ тн рейшефъйд бгшвд 1 тг 2, шч 2 оиефмеъ гйеезе тм ъсойрйн 12 зегщйн мазш дъзмъ дийфем дощемб, елм 8 доиефмеъ тн рейшефъйд бгшвд 3-4 гйеезе тм дтгш ъсойрйн мазш 12 зегщйн. баефп лммй 93% одоиефмеъ гйеезе тм дтгш ъсойрйн мазш щрд оъзймъ дийфем дощемб. дзечшйн ослойн лй мийфем ощемб бгйчеш ебшфмчсемевйд феирцйам ийфемй рйлш мщйфеш ъсойрй рейшефъйд тм шчт лйоеъшфйд, аемн йщ мащщ аъ дооцайн бозчш длемм чбецъ бйчешъ елп мдтшйк одй ддщфтд дорйтъйъ щм ийфем жд.
https://www.ncbi.nlm.nih.gov/pubmed/28150504
бозчш ъцфйъй шб-ошлжй (йреаш 2017), щртшк биешчйд ебе рлмме 281 земй сшип, роца лй щлйзеъ дщйоещ бъесфйн цозййн мфрй рйъез дйд 39% етмд м-54% бодмк ийфемй длйоеъшфйд. дъесфйн дщлйзйн бйеъш дйе ъесфй щен (Alium sativum) мфрй рйъез еъесфй сшфг (Urtica dioica) бодмк длйоеъшфйд. мошеъ дщлйзеъ двбедд, ошбйъ доиефмйн цййре лй ма рщаме мвбй щйоещ бъесфйн тм йгй дцееъ доифм.
https://www.ncbi.nlm.nih.gov/pubmed/28573249
бозчш течбд (сфиобш 2017), добесс тм шщеоеъ дбйиез дшфеай дмаеой биайееап, рбгч оде дчщш бйп дщйоещ бшфеаъ цозйн сйрйъ мбйп дсйлеп мдъфъзеъ сшип дщг. бозчш рлмме дръерйн щм 184,386 рщйн бвймай 20-79 - оъек огвн маеой оййцв щм лоймйеп айщ. бодмк ъчефъ отчб щм л-13 щрйн аебзре 1,853 очшйн щм сшип щг фемщрй. баефп лммй дщйоещ бшфеаъ цозйн сйрйъ дйд вбед (л-80%).
роца лй бчшб рщйн щма дщъоще лмм бшфеаъ цозйн сйрйъ щйтеш очшй сшип дщг дйд 1.73 млм 10,000 щреъ агн, лащш дщйтеш дйд 0.85 млм 10,000 щреъ агн тбеш рщйн щдщъоще бшфеаъ цозйн сйрйъ е-0.63 тбеш рщйн щдщъоще бфешоемд Si Wu Tang [долймд шдорйд (Rehmannia glutinosa), агоерйъ (Paeonia spp), арв'мйчд сйрйъ (Angelica sinensis) емйвесийчен (Ligusticum striatum)]. ръерйн амд обиайн сйлеп роек мсшип дщг б-43% еб-64%, бдъаод. дзечшйн ослойн лй аеорн орврерй дфтемд айрн йгетйн, дщйоещ бшфеаъ цозйн сйрйъ тщейд мдееъ асишивйд йтймд морйтд тбеш рщйн бсйлеп вбед.
https://www.ncbi.nlm.nih.gov/pubmed/28858112
бсчйшд (ребобш 2016) оецвйн дооцайн оозчшйн фшд-чмйрййн бревт мдщфтд дарий-сширйъ щм ойцей шежошйп (Rosmarinus officinalis) ешлйбйе дфтймйн (carnosic acid, rosmarinic acid) елп мвбй орврерй дфтемд дчщешйн блк.
https://www.ncbi.nlm.nih.gov/pubmed/27869665
бозчш отбгд (аечиебш 2016) огвйойн дзечшйн аъ ддщфтд дарий-сширйъ щм чедещ щзеш (Cimicifuga racemosa) лрвг вйгемйн ъмейй асишевп, бойезг вйгемйн бшйшйъ дшзн.
https://www.ncbi.nlm.nih.gov/pubmed/27223250
бсчйшд щйиъйъ (аевеси 2016) детшле дтгейеъ оозчшйн ачшаййн обечшйн бревт мйтймеъ ембийзеъ щм шфеаъ цозйн сйрйъ мийфем бсшип дтшоерйъ. бсчйшд рлмме 17 озчшйн, бдн 1,224 ощъъфйн, лащш бошбйъ дозчшйн рбгч дщйоещ бшфеаъ цозйн сйрйъ лийфем ъеок ащш рйъп бцешъ ошъз.
баефп лммй дооцайн оцбйтйн тм лк щдийфем дощемб дйд йтйм йеъш одийфем даргечшйрй бмбг бтйлеб дъчгоеъ дозмд бл-10 зегщйн, бдашлъ ощк ддйщшгеъ б-7-15 зегщйн ебщйфеш дъфчег еайлеъ дзййн щм доиефмйн. йзг тн жаъ, дзечшйн оцййрйн лй ооцайн амд дйрн оевбмйн бщм дайлеъ доъегемевйъ дроелд щм дозчшйн. ма геез тм дщфтеъ щмймйеъ ощотеъйеъ дчщешеъ бийфем.
бозчшйн дщерйн ртщд щйоещ бфешоемеъ щереъ долймеъ овееп вгем щм цозй ошфа, лащш дцозйн дщлйзйн бйеъш бдн ртщд щйоещ леммйн чгг чшеой (Astragalus membranaceus), аишчиймегс (Atractylodes macrocephala), чегерефсйс (Codonopsis pilosula) ефишййъ фешйд (Poria cocos). дзечшйн ослойн лй ргшщйн озчшйн ресфйн байлеъ вбедд тм оръ мащщ аъ дооцайн еаъ дъшеод щм дщйоещ бшфеаъ цозйн сйрйъ моиефмйн тн сшип дтшоерйъ.
https://www.ncbi.nlm.nih.gov/pubmed/27490098
бсчйшд (2017) оецвйн дооцайн, бтйчш оозчшйн фшд-чмйрййн, бревт мфеирцйам щм овееп шлйбйн цозййн мъшен мщйфеш дфтймеъ дзйсерйъ бсшип дщг. йщрп тгейеъ млк щмшлйбйн цозййн щерйн дщфтд ревгъ сшип баоцтеъ орврерйн бйемевййн щерйн, лемм ейсеъ дфтймеъ дзйсерйъ щдебймд мдфзъъ вгймъ дъайн дсширййн. дтгейеъ оцбйтеъ тм дфеирцйам щм цозй дошфа дбайн мийфем бсшип дщг: щещ чйшз (Glycyrrhiza glabra), аерчшйд (Uncaria tomentosa), ъд йшеч (Camellia sinensis), в'йрсрв чешйарй (Panax ginseng), афшсч (Prunus armenaica), щен (Allium sativum), мфд вгемд (Arctium lappa) елешлен (Curcuma longa).
бозчшй отбгд роца лй мцозйн амд шлйбйн бтмй фтймеъ оеесъъ зйсерйъ дчщешд бдщфтд ревгъ дсшип щмдн. шлйбйн амд леммйн: ajoene, arctigenin, β-carotene, curcumin, epigallocatechin-3-gallate, ginsan, glabridin, quinic acid. босвшъ дсчйшд грйн дзечшйн бфйшеи бдщфтд щм шлйбйн амд ебййщен дафщшй мийфем бсшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/27539316
боид-армйжд (оай 2017) щм озчшйн ачшаййн обечшйн детшлд дъшеод щм шфеаъ цозйн сйрйъ моиефмйн тн сшип дмбмб, дочбмйн лйоеъшфйд. брйъез дръерйн рлмме 22 озчшйн, ащш бгче 9 фешоемеъ дрйъреъ бжшйчд тм 1,329 оиефмйн сд"л. одъецаеъ темд лй бдщееад млйоеъшфйд бмбг, дщйоещ бщмещ одфешоемеъ дйд омеед бсйлеййн вбедйн йеъш мщйфеш дъфчег дйен-йеой едвефрй, тм фй догг Karnofsky performance score) KPS):
тег роца лй бдщееад млйоеъшфйд бмбг, ийфем дощмб жшйчъ Aidi дйд йтйм йеъш мдфзъъ мейчефрйд. Aidi – олймд асишвмес (Astragalus membranaceus), в'йрсрв сйбйшй (Eleutherococcus senticosus) езйфещйъ оджп Mylabris phalerata.
ма роцад дщфтд мийфем дощемб тм огг дйтймеъ дчмйрйъ етм шоъ дбзймеъ еддчаеъ. йзг тн жаъ, шеб дфешоемеъ роцае йтймеъ йеъш, бдщееад млйоеъшфйд бмбг, мдфзъъ дщфтеъ щмймйеъ (мейчефрйд ебзймеъ едчаеъ). дзечшйн ослойн лй щймеб щм шфеаъ цозйн сйрйъ тн дийфем длйоеъшфй тщей мъшен моиефмйн тн сшип дмбмб мщйфеш дъфчег емдфзъъ ддщфтеъ дщмймйеъ.
https://www.ncbi.nlm.nih.gov/pubmed/28538415
боаош (ребобш 2016) оецвъ счйшд щм дтгейеъ оозчшйн ачшаййн обечшйн бревт мйтймеъ щм ъесфйн цозййн мийфем бъзмеад лшерйъ.
- йъш мзх гн: йщрн ооцайн дъеолйн бйтймеъ щм щен (Allium sativum) ещм дйбйсчес (Hibiscus sabdariffa) мдешгъ мзх дгн, лащш дщйоещ бв'йрсрв чешйарй (Panax ginseng) ма роца йтйм мщйфеш речщеъ дтешчйн бчшб оиефмйн тн йъш мзх гн доиефмйн ъшефъйъ.
- йъш щеорйн бгн: ъесфйн цозййн щроцае йтймйн мщйфеш фшефйм дщеорйн леммйн щен (Allium sativum) ещошй аешж аген.
- гмчъ офшчйн рйеерйъ: ъесфйн цозййн щроцае йтймйн мийфем бъсойрйн щм гмчъ офшчйн рйеерйъ леммйн дшфве (Harpagophytum procumbens), тшбд мбрд (Salix alba), лешлен (Curcuma longa) емберд (Boswellia spp).
- сшип: мошеъ щаерчемевйн шбйн оървгйн мриймъ ъесфйн бодмк дийфем дарий-сширй, давегд маерчемевйд айрившийбйъ (SIO) оомйцд тм осфш шлйбйн цозййн щтщеййн мдйеъ бтмй дщфтд ойийбд, лемм лешлеойп, фишййъ ойиачй (Grifola frondosa), ъд йшеч (Camellia sinensis) еасишвмес (Astragalus membranaceus).
- селшъ сев 2: йщрн шлйбйн цозййн шбйн щрзчше бдчщш мийфем бселшъ, аемн дозчшйн дчмйрййн дтглрййн дйрн оевбмйн. тм бсйс дозчшйн дчййойн, дзечшйн ослойн лй ма роцад ъойлд мйтймеъ щм чйроеп (Cinnamomum zeylanicum) майжеп шоеъ дселш, аемн йщрн ооцайн дъеолйн бдщфтд дойийбд щм зймбд (Trigonella foenum-graecum). дзечшйн ослойн лй ргшщйн озчшйн ресфйн байлеъ оъегемевйъ вбедд йеъш ащш оъййзсйн мдйбийн щм сбймеъ ебийзеъ, лащш боцбйн щм ъзмеад лшерйъ йщ мдъайн айщйъ аъ дщйоещ бъесфйн цозййн, ъек дъййзсеъ майришачцйеъ тн дийфем дъшефъй.
https://journals.lww.com/tnpj/Fulltext/2016/11000/Herbal_supplements_used_to_treat_common_chronic.6.aspx
бсчйшд (ребобш 2017) оецвеъ дтгейеъ оозчшйн фшд-чмйрййн мвбй ддщфтд ревгъ дсшип щм оибемйийн ощрййн дойецшйн овшсйрйд (Garcinia) ефшт озешш (Hypericum perforatum) еорврерй дфтемд щмдн.
https://www.ncbi.nlm.nih.gov/pubmed/28363851
орйъез дръерйн (2019) щм ълрйъ дчрабйс щм огйръ ойрсеид башд"б, роца лй щйоещ бчрабйс шфеай бчшб земй сшип рсбм дйиб едйд йтйм мдфзъъ ъсойрй зшгд, аебгп ъйабеп, гйлаеп, дфштеъ щйрд, тййфеъ, бзймд, лаб едчаеъ.
https://www.ncbi.nlm.nih.gov/pubmed/30860938
зжшд мъзймъ дозчшйн
ъд йшеЙч
озчш дощк (ошх 2014) мозчш чмйрй обечш фмсбе ащш ретг мбзеп аъ ддщфтд щм ойцей ъд йшеч брщйн тн сшип щг щмймй мчемирйн дешоермййн бгшвд 1-3 баоцтеъ рйъез гвйоеъ дгн едщъп щрасфе бозчш.
дрщйн бозчш земче баефп ачшай мчбецъ дфмсбе ае мчбецъ дийфем щримд ойцей идеш щм ъд йшеч (Polyphenon E) бойрерйн щерйн, 400 о"в, 600 о"в ае 800 о"в, фтоййн бйен бощк 6 зегщйн.
роца лй мазш зегщййн риймъ ойцей ъд йшеч дебймд мйшйгд оебдчъ бшоъ дешоеп двгймд HGF бдщееад мфмсбе (12.7%- мтеоъ 6.3%), лащш бдощк дийфем рщошд овоъ дйшйгд ак ддбгм ма дйд оебдч сиийсийъ. бресу, жедъд овод щм йшйгд блемсишем бчбецъ дъд дйшеч.
ма роцае дщфтд тм оггй дгмчъ ае тм дфтймеъ ревгъ дзоцеп.
http://www.ncbi.nlm.nih.gov/pubmed/24646362
счйшд щйиъйъ еоид-армйжд (йемй 2015) щретгд мбзеп аъ дчщш бйп цшйлъ ъд йшеч еъд щзеш мбйп дсйлеп мсшип дшзн. ск длм рлмме бсчйшд 13 озчшй течбд еозчшй очшд-бчшд.
бдъбсс тм 6 озчшйн бдн рбгчд дцшйлд щм ъд йшеч, роца лй шоъ дцшйлд двбедд бйеъш щм ъд йшеч дййъд чщешд бйшйгд щм л-22% бсйлеп мсшип дшзн бдщееад мшоъ дцшйлд дроелд бйеъш. тег роца лй тмйд бцшйлъ дъд дйшеч блес азъ мйен дййъд чщешд бйшйгд щм 11% бсйлеп мсшип дшзн.
брйъез лемм щм 9 озчшйн бдн рбгчд дцшйлд щм ъд щзеш, ма роца чщш бйп цшйлъ ъд щзеш едсйлеп мсшип дшзн. дзечшйн ослойн лй ооцайн амд оцбйтйн тм лк щцшйлъ ъд йшеч, ак ма ъд щзеш, тщейд мдйеъ бтмъ дщфтд овйрд офрй дъфъзеъ сшип дшзн.
http://www.ncbi.nlm.nih.gov/pubmed/26138307
счйшд (йемй 2015) дослоъ аъ ддщфтд дбйемевйъ щм ъд йшеч едййщен дчмйрй дафщшй бдчщш щм бтйеъ теш.
бдъбсс тм ооцайн оозчшйн афйгойемевййн ерйсеййн бдн дегвод дфтймеъ дарий-сширйъ еарий-гмчъйъ, йщре щйоещ шзб бойцей ъд йшеч боецшйн гшоиемевййн ечесоиййн.
босвшъ дсчйшд оцйвйн дзечшйн аъ дтгейеъ бревт мдщфтд дбйемевйъ щм ъд йшеч едшлйб дфтйм EGCG, бгвщ тм фтймеъ ревгъ зоцеп еарий-гмчъйъ. бдощк оецвеъ дтгейеъ бревт мййщен дчмйрй едзйцерй щм ойцей ъд йшеч мийфем ббтйеъ теш, лемм дврд оржчй чшйрд есшип дтеш, жйдеой теш, ачрд, аиефйч гшоийийс, шчод цмчъйъ, рщйшъ щйтш ешйфей фцтйн.
дзечшйн ослойн лй мошеъ дооцайн добийзйн, йщрн шч оти озчшйн чмйрййн обечшйн ергшщйн озчшйн ресфйн тм оръ мдтшйк аъ дйтймеъ щм ъд йшеч мийфем ббтйеъ теш емвбщ домцеъ мщйоещ чмйрй.
http://www.ncbi.nlm.nih.gov/pubmed/26177066
счйшд (гцобш 2015) доцйвд аъ дщйоещ босфш шлйбйн цозййн доелшйн басйд мийфем еорйтд щм сшип ботшлъ дтйлем, лемм в'йрсрв чешйарй (Panax ginseng), лешлеойп, ъд щзеш, ъд йшеч (Camellia sinensis), в'рйсийап доцей биефе, дшлйбйн дфтймйн бщен (Allium sativum), чфсайцйп, в'йрв'шем есймйошйп.
http://www.ncbi.nlm.nih.gov/pubmed/26651248
счйшд (2016) дтесчъ бфтймеъ дарий-сширйъ щм шлйбйн ъжеръййн щерйн, бгвщ тм ъшеоън мийфем бсшип дщг.
дсчйшд леммъ фйшеи мвбй зеоцъ щеоп аеовд 3 доефчъ огвйн, шжшбишем доцей бтрбйн е-EGCG доцей бъд йшеч елп оефч одцоз Ziziphus jujube.
босвшъ дсчйшд оцйвйн дзечшйн аъ орврерй дфтемд доемчемшййн бдн шлйбйн амд отлбйн ъдмйлйн сширййн, бйрйдн ейсеъ дфтймеъ щм аржйойн ревгй зоцеп ейцйшъ дщфтд арий-фшемйфшийбйъ (тйлеб щвщев ъайн сширййн) еафефиеийъ (тйгег оееъ ъайн сширййн).
дзечшйн чешайн мчйен озчшйн ресфйн мдтшлъ дщйоещ дчмйрй бшлйбйн амд лзмч одийфем бсшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/26156544
бсчйшд щйиъйъ еоид-армйжд (ошх 2017) рбгч дчщш бйп цшйлъ ъд йшеч мбйп дсйлеп мсшип дтшоерйъ. бсчйшд рлмме щбтд озчшйн ъцфйъййн (ашбтд озчшй течбд ещмещд озчшй очшд-бчшд) ещмещд озчшйн ачшаййн обечшйн, бдн рйъп 400 о"в/йен EGCG ае 600 о"в/йен чилйрйн оъд йшеч мощк 12-30 зегщйн.
брйъез лемм щм дозчшйн дъцфйъййн ма роца дбгм оебдч бсйлеп мсшип дтшоерйъ бйп дощъъфйн тн дцшйлд двбедд бйеъш щм ъд йшеч, мтеоъ дроелд бйеъш. тн жаъ, роцад овод, щайррд оебдчъ сиийсийъ, мфйд лм тмййд щм лес азъ мйен бцшйлъ ъд йшеч дййъд чщешд бйшйгд бсйлеп мсшип дтшоерйъ баефп ъмей ойреп, лащш цшйлд щм 7 лесеъ еотмд дййъд чщешд бсйлеп роек йеъш баефп оебдч. бозчшйн добечшйн роца лй цшйлъ ъд йшеч дййъд омеед бсйлеп роек бл-60% мдъфъзеъ сшип дтшоерйъ бчшб аелмесййд бсйлеп бдщееад мфмсбе.
ооцайн амд оцбйтйн тм дфеирцйам щм ъд йшеч мдврд офрй дъфъзеъ сшип дтшоерйъ, аемн ргшщйн озчшйн ресфйн тм оръ мбсс аъ досчреъ емвбщ домцеъ мщйоещ чмйрй.
https://www.ncbi.nlm.nih.gov/pubmed/28353571
бсчйшд, длеммъ озчшйн фшд-чмйрййн ечмйрййн (2016), оецвйн орврерй дфтемд дарий-сширййн щм ъд йшеч (Camellia sinensis), дчщешйн бфтймеъ ревгъ зоцеп, ак вн бдвбшъ фтймеъ зоцерйъ дфевтъ бъайн дсширййн.
https://www.ncbi.nlm.nih.gov/pubmed/27221834
счйшд (ребобш 2015) доцйвд аъ дтгейеъ дозчшйеъ бревт мдщфтд щм овееп вгем щм шлйбйн ибтййн ецозййн лрвг ъай вжт сширййн. чййоъ вйщд мфйд дочеш мвйгем сширй деа бчбецд чирд щм ъайн тн оафййрйн щм ъай вжт еорврерйн щм дйщшгеъ едъзгщеъ елъецад олк ъайн амд тойгйн бфрй ошбйъ дъшефеъ длйоеъшфйеъ.
озчшйн щерйн оцбйтйн тм лк щшлйбйн ибтййн щерйн тщеййн мдщфйт тм осмемйн дотешбйн ббйией дврий щм ъайн амд еблк осфчйн ъойлд мчщш бйп ъжерд одцеоз мбйп дфзъъ щйтеш дооайшейеъ.
бсчйшд офешийн дооцайн мвбй шлйбйн шбйн, бйрйдн смйреойцйп, семфешафп, айжефмберйн осейд, EGCG (ъд йшеч), шлйбйн саферйрйн, чеешцийп, лешлеойп, фемйфреЙмйн лое в'йрв'шем етег.
http://www.ncbi.nlm.nih.gov/pubmed/26503998
щъй счйшеъ тглрйеъ (аечиебш 2013) ащш фешсое блъб дтъ даошйчай мъжерд чмйрйъ тесчйн бйтймеъ щм ъд йшеч морйтъ сшип. азъ дсчйшеъ оцйвд тгейеъ отешбеъ дтемеъ оозчшйн афйгойемевййн еослоъ лй дъфчйг щм ъд йшеч борйтъ сшип айре зг ощотй ергшщйн озчшйн чмйрййн ресфйн тм оръ мчбет домцеъ мцшйлъ ъд йшеч мцешк орйтъ сшип. дсчйшд дщрййд безръ аъ дооцайн оозчшй отбгд еозчшйн дътшбеъййн ббрй агн егрд брещайн бдн ргшщйн озчшйн ресфйн. мсйлен, ощъй дсчйшеъ темд лй чййоъ ъойлд бъфчйг щм ъд йшеч мдврд офрй севйн щерйн щм озмеъ ооайшеъ, аемн ргшщ озчш ресу бъзен тм оръ мвбщ домцеъ мцешк ийфем еорйтд. йзг тн жаъ, мъд йшеч тщеййн мдйеъ йъшереъ бшйаеъййн щерйн, отбш мдврд офрй ооайшеъ, ебщм дйеъе биез мщйоещ, итйн ежем аре оомйцйн тм цшйлъ ъд йшеч лзмч одъфшйи дйеой.
http://www.ncbi.nlm.nih.gov/pubmed/24172305
http://www.ncbi.nlm.nih.gov/pubmed/24172300
бозчш фйймеи лфем-сойеъ обечш фмсбе (фбшеаш 2017) рбгчд ддщфтд щм ийфем бшлйбйн ибтййн тм чцб тмййъ догг PSA бчшб вбшйн тн дйщреъ бйелйойъ щм сшип дтшоерйъ, доаефййрйн бтмййд бйрерйъ б-PSA.
бозчш дщъъфе 22 вбшйн тн жоп длфмъ PSA щм 4-15 зегщйн емма тгеъ мвшешеъ. дощъъфйн земче ачшайъ мчбецъ дийфем ае мчбецъ дфмсбе мощк 12 щбетеъ. дийфем лмм риймъ 4 ибмйеъ мйен оъесу ибтй долйм 100 о"в лешлеойп, 30 о"в шжбшишем е-100 о"в ъд йшеч мибмйд, елп 4 лоесеъ мйен щм рбий бшечемй ошелжйн (щеед тшк м-8 вшн мйен рбийн ишййн). оишъ дозчш дтйчшйъ дййъд мдтшйк аъ дйълреъ доъегемевйд дозчшйъ елп мбзеп аъ ддщфтд тм шоъ дъсойрйн, айлеъ дзййн еоцб дшез. роца лй дтойгд бфшеиечем дозчш дййъд иебд оаег едийфем рсбм дйиб, мма дбгм бйп дчбецеъ бйзс мдщфтеъ дщмймйеъ.
дзечшйн оцййрйн лй ма дййъд цйфййд бозчш дфйймеи мдбгмйн оебдчйн бйп дчбецеъ бйзс м-PSA емоггйн дчмйрййн. тн жаъ, брйвег моцефд, бчбецъ дийфем роцад дзошд бжоп длфмъ д-PSA, ак дзечшйн оцййрйн лй ддбгм айре оебдч сиийсийъ еиеез дитеъ дйре вгем лк щдн оцйтйн мдощйк ембзеп аъ дщфМтъ ъесфйн амд бозчш обечш бдйчу вгем йеъш.
https://www.ncbi.nlm.nih.gov/pubmed/28181675
озчш отбгд (фбшеаш 2015) доцбйт тм дйтймеъ щм ъесу цозй долйм чеешцийп, лешлеойп, ъд йшеч, ойцей йшчеъ оцмйбйн ешжбшишем мийфем бсшип шащ ецееаш бземй аройд т"щ фрчерй (озмд врийъ чщд доъбиаъ бзесш ъай гн).
http://www.ncbi.nlm.nih.gov/pubmed/25695860
бсчйшд (йемй 2016) оецвйн дооцайн оозчшйн афйгойемевййн еоозчшйн фшд-чмйрййн, доцбйтйн тм дъшеод дафщшйъ щм цшйлъ ъд мдфзъъ дсйлеп мсшип дщг, ъек дгвщъ ддщфтд дотлбъ щм EGCG тм дъфъзеъ ъайн сширййн.
https://www.ncbi.nlm.nih.gov/pubmed/27483305
бсчйшд (ребобш 2016) грйн дзечшйн бооцайн оозчшйн фшд-чмйрййн, дтесчйн бдщфтд дарий-сширйъ щм чилйрйн оъд йшеч (EGCG), бгвщ тм орврерй дфтемд дбйе-фйжйчамййн, ебъшеод дафщшйъ мийфем бсшип еморйтъе. мгевоа, йщрн озчшйн дошайн лй EGCG вешн мтмййд бречщеъ дообшрд щм ъайн сширййн, ак ма щм ъайн бшйайн, бгеод мдщфтд щм ъшефеъ лйоеъшфйеъ. бресу, дайришачцйд тн дшлйбйн дщеорййн бообшрд февтъ бцойгеъ щм дъайн дсширййн, азг доафййрйн дбйе-фйжйчамййн дтйчшййн дчщешйн бдъфъзеъ вшешеъ.
https://www.ncbi.nlm.nih.gov/pubmed/27869750
бозчш отбгд (2021) безрйн дзечшйн аъ орврерй дфтемд ревгй дсшип щм EGCG, еошайн лй м EGCG йщ дщфтд тм дзмбеп p53 дотешб бъйчеп ржчйн м-DNA етйгег дъоеъд щм ъайн сширййн.
https://pubmed.ncbi.nlm.nih.gov/33579943/
зжшд мъзймъ дозчшйн
лМешлен елМеМшлеойп
орйтд | ийфем | дфзъъ ъефтеъ мееай
орйтд
озчш чмйрй шащерй (2001) бзп аъ бийзеъ ейтймеъ дриймд щм лешлеойп бойреп вбед лаоцтй морйтъ сшип бчшб 25 рбгчйн бсйлеп вбед. 25 рбгчйн (иеез вймайн 36-77) доевгшйн бсйлеп вбед мфъз сшип. мрбгчйн дйе бйп дщаш рвтйн ишен сширййн бщмфезйъ дщъп, озмъ беап щм дтеш (щмб оечгн ещизй щмсшип ъай дчщчщ), рвтйн ишен ооайшйн бцееаш дшзн, чшръ бедчъ (мейчефмчйд бзмм дфд), еоифмжйд айрисийрмйъ бчйбд (дщъреъ ъай дафйъм бчйбд моцб дгеод мъай дотй). дрбгчйн иефме баоцтеъ ъоцйъ ъчрйъ щм лешлен (оъечрръ мдлйм 99.3% лешлеойп блм ибмйд) бощк щмещд зегщйн лащш дойреп ддъзмъй дйд 500 о"в мйен едетмд бдгшвд м-12 вшн мйен. бъен ддътшбеъ рбгчъ азъ оъек 4 рбгчеъ тн рвтйн ишен сширййн бцееаш дшзн, ербгч азг оъек щбтд тн чшръ бедчъ бзмм дфд фйъзе сшип мошеъ дийфем блешлеойп. мтеоъ жаъ, рцфд щйфеш дйсиемевй боцб дрвтйн дишен сширййн бчшб 1 оъек 2 рбгчйн тн рвтйн бщмфезйъ дщъп, 2 оъек 7 рбгчйн тн чшръ бедчъ (мейчефмчйд) бзмм дфд, 1 оъек 6 рбгчйн тн оифмжйд айрисийримйъ бчйбд, 1 оъек 4 рбгчеъ тн рвтйн ишен сширййн бцееаш дшзн е-2 оъек 6 рбгчйн тн озмъ беап щм дтеш. ъефтеъ штймеъ геезе дзм оойреп щм 8 вшн мйен, лщоъзъ мойреп жд лешлеойп рсбм дйиб едйд биез мщйоещ. ск длм рцфд щйфеш дйсиемевй бчшб 7 оъек 25 рбгчйн (28%). дщйфеш рцфд блм дойрерйн щрбгче.
https://www.ncbi.nlm.nih.gov/pubmed/11712783
озчш чмйрй (2016) ачшай лфем сойеъ еобечш фмсбе бзп аъ йтймеъ лешлеойп (BCM95–Biocurcumax) бриймд феойъ бийфем бмейчефмчйд. 223 рбгчйн дсебмйн очшръ бедчъ (мейчефмчйд – рвтйн ишен сширййн) бзмм дфд земче ачшайъ мчбмъ лешлеойп бойреп 3.6 вшн мйен ае фмсбе бощк щйщд зегщйн. ъесу длешлеойп длйм ъоцйъ ъчрйъ оъечрръ мдлйм 88% лешлеореайгйн е-7% щорйн аъшййн доефчйн оцоз длешлен. бъен ддътшбеъ щйтеш дрбгчйн щзее щйфеш чмйрй ома дйд 67.5% бчбецъ длешлеойп бдщееад м-55.3% бчбецъ дфмсбе (p=0.03). лтбеш щйщд зегщйн оъен ддътшбеъ щйтеш доиефмйн щма зее дйщреъ щм дрвтйн дйд 88.9% бчбецъ длешлеойп бдщееад м-87.5% бчбецъ дфмсбе. ма рцфе дбгмйн оебдчйн бйп лешлеойп ебйп фмсбе ббгйчд ддйсиемевйъ (p=0.71), ак бщймеб дъвебд дчмйрйъ еддйсиемевйъ мийфем дегвн йъшеп оебдч млешлеойп тм фрй фмсбе (p=0.02). дощк дийфем бчшб рбгчйн тн щйфеш змчй лтбеш щйщд зегщй ийфем ма дгвйн щйфеш ресу. дийфем баоцтеъ лешлеойп дйд биез.
https://www.ncbi.nlm.nih.gov/pubmed27267893
озчш чмйрй ачшай лфем сойеъ еобечш фмсбе (2010) бзп аъ йтймеъ дщймеб щм лешлеойп еайжефмберйн морйтъ сшип дтшоерйъ бчшб рбгчйн бсйлеп вбед. 85 рбгчйн тн шоеъ арийвп сфцйфй мтшоерйъ PSA вбедеъ мма сшип ае дщъреъ ишен сширйъ земче ачшайъ мчбмъ фмсбе ае ъесу дощмб лешлеойп бойреп 100 о"в мйен еайжефмбеп сейд бойреп 40 о"в мйен бощк щйщд зегщйн. бъен ддътшбеъ, бъъ чбецд щм рбгчйн тн тшлй PSA≥10 рцфъд йшйгд оебдчъ бтшлй д-PSA бдщееад мфмсбе (p=0.01). дзечшйн ощтшйн лй щмйид бшоеъ дгмчъ бтшоерйъ, лфй щбае мйгй бйией бшоеъ дарийвп дсфцйфй PSA дйа щоертъ аъ дъфъзеъ дсшип.
https://www.ncbi.nlm.nih.gov/pubmed/20503397
озчш чмйрй зг сойеъ обечш фмсбе бобрд оецмб (2009) бзп аъ йтймеъ лешлеойп борйтъ ойамеод рфецд бчшб рбгчйн бщмб ишен сширй (MGUS-Monoclonal gammopathy of undetermined significance). б-MGUS ъай дфмсод одеейн фзеъ о-10% оъай оз дтцн еайп ъсойрй озмд. 26 рбгчйн тн MGUS земче ачшайъ мщъй чбецеъ бйзс щм 2:1 мриймъ лешлеойп бойреп 4 вшн мйен (лешлеойп 3600 о"в, DMT бойреп 320 о"в, BDMT бойреп 80 о"в) ае фмсбе мощк щмещд зегщйн емазш олп децмбе дрбгчйн мчбмъ дийфем дрвгй мощк щмещд зегщйн ресфйн. бъен ддътшбеъ роца щлешлеойп дфзйъ аъ шоеъ древгп дзг щбий (дойецш тм йгй ъай дфмсод, одеед соп мдъфъзеъ дозмд) бчшб тщшд одземйн бчбецъ длешлеойп тн шоеъ ревгп вбедеъ о-20 вшн/мгцймйиш (дфзъд щм 12-30% бчшб зойщд одн). бчшб щаш дрбгчйн щриме лешлеойп (щбтд) ма змд йшйгд бшоъ древгп ебчшб дрбгчйн щриме фмсбе (ъщтд) ма змд йшйгд ебзмчн ау змд тмйд бшоъ древгп. бресу, бчшб 27% одрбгчйн бчбецъ длешлеойп змд дфзъд щм мотмд о-25% бфйшеч дтцн (мфй дсоп N-telopeptide of type I collagen бщъп). орвреп дфтемд щм дъесу едщАфтъе тм змч одрбгчйн ак ма тм лемн айрн бшешйн оп дозчш.
https://www.ncbi.nlm.nih.gov/pubmed/19737963
озчш чмйрй обечш фмсбе (2005) бзп аъ йтймеъ лешлеойп бийфем бгмчъ мбмб лшерйъ (tropical pancreatitis). огебш бгмчъ лшерйъ даефййрйъ мажешйн ачмйоййн ишефййн щодеед вешн сйлеп мдъфъзеъ сшип дмбмб. йщрд сбшд щтчд зоцерйъ дйа двешоъ мдефтъ дгмчъ длшерйъ бмбмб. 20 рбгчйн риме лешлеойп бойреп 500 о"в мйен бщймеб тн фйфшйп бойреп 5 о"в мйен ае фмсбе бощк щйщд щбетеъ. бтчбеъ риймъ длешлеойп змд йшйгд оебдчъ бзоцеп дщеорйн (мфй шоъ домергйамгдйгйн) етмйд оебдчъ бшоъ двмеиийеп бъай дгн дагеойн бдщееад моцб дбсйс. тн жаъ, ма рцфе щйреййн бшоъ длаб щгеезе дрбгчйн.
https://www.ncbi.nlm.nih.gov/pubmed/16394323
озчш чмйрй оцеоцн ебмъй обечш (2006) бзп аъ йтймеъ ъесу дощмб лешлеойп ечеешцийп борйтъ сшипщм дотй едзмземъ бчшб рбгчйн дсебмйн оъсоеръ фемйфежйс ощфзъйъ (Familialadenomatous polyposis). жедй ъсоеръ ъешщъйъ доъафййръ бдефтъ оаеъ фемйфйн ботй двс ебзмземъ еодеед вешн сйлеп мдъфъзеъ сшип. зойщд рбгчйн (брй 22-54) щтбше рйъез щбе десш змч одотй двс ещайрн реимйн сишеайгйн риме лешлеойп (сев ойцей ма цейп) бойреп 1440 о"в ечеешцийп бойреп 60 о"в мйен бощк щйщд зегщйн. бъен ддътшбеъ осфш дфемйфйн фзъ б-60.4% (p=0.043) евегмн фзъ б-50.9% (p=0.039) бдщееад моцб дбсйс. дийфем рсбм дйиб ершщое ъефтеъ мееай чмеъ бмбг.
https://www.ncbi.nlm.nih.gov/pubmed/16757216
озчш чмйрй ма обечш (2011) бзп аъ йтймеъ лешлеойп бийфем брвтйн ойчшесчефййн ишен сширййн ботй двс (ACF-colonic aberrant crypt foci) бчшб отщрйн. 44 рбгчйн отщрйн тн рвтйн ишен сширййн ботй двс риме лешлеойп бойреп 2 ае 4 вшн мйен бощк 30 йойн. 41 рбгчйн дщмйое аъ ддътшбеъ. бъен ддътшбеъ, бтчбеъ риймд щм щрй дойрерйн ма рцфд щйрей бшоеъ айчесреайгйн фше-чшцйреврйн (PGE2, 5-HETE) бгвйод щм шчоъ отй рчййд орвтйн ебшчоъ отй рветд, ак рцфъд дфзъд оебдчъ щм 40% босфш дрвтйн бтчбеъ риймъ лешлеойп бойреп двбед (p<0.005). лешлеойп рсбм дйиб бщрй дойрерйн, ак гшещйн озчшйн ресфйн лгй мчбет аъ орвреп дфтемд щм лешлеойп борйтъ сшип дотй двс бчшб отщрйн.
https://www.ncbi.nlm.nih.gov/pubmed/21372035
озчш чмйрй ачшай обечш (2010) ботшб брвм бзп аъ йтймеъ лешлеойп борйтъ ржчй DNA бтчбеъ зщйфд машсп. гвйоеъ гн щм 286 рбгчйн бшйайн (мма ъефтеъ штймеъ) брй 25-55 бажешйн дзщефйн мжйден ашсп оъощк дгвйое ржч ощотеъй м-DNA елп йцйшъ ROS езоцеп щеорйн. дрбгчйн земче ачшайъ мчбецъ дътшбеъ ечбецъ фмсбе. чбецъ ддътшбеъ римд лешлеойп бщймеб фйфшйп (йзс щм 20:1) бойреп щм 2.5 вшн мйен бощк щмещд зегщйн. бъен ддътшбеъ роца щлешлеойп дфзйъ (p<0.001) аъ ржчй д-DNA, шоеъ д-ROS еаъ зоцеп дщеорйн бгон щм дрбгчйн едвбйш аъ фтймеъ даржйойн ревгй дзоцеп (Catalase, SOD, glutathione reductase, glutathione S-tranferase, glutathione peroxidase) еаъ шоеъ ревгй дзоцеп дма аржйоъййн бдщееад мфмсбе.
https://www.ncbi.nlm.nih.gov/pubmed/20056736
бозчш чмйрй обечш (1992) рбзрд ддщфтд дарий-оеиврйъ щм лешлен бчшб отщрйн. 16 отщрйн лшерййн риме абчъ лешлен бойреп 1.5 вшн мйен бощк 30 йойн. бъен ддътшбеъ рцфъд дфзъд оебдчъ блоеъ дзеошйн доеиврйн доефшщйн бщъп. мзймефйп, бчшб щйщд рбгчйн ма отщрйн бшйайн щщйоще лчбецъ бйчешъ ма рцфд щйрей бдфшщъ доеиврйн бщъп. мриймъ длешлен ма дйъд дщфтд оебдчъ тм ъфчегй длбг (мфй шоеъ аржйой длбг бсшен AST е-ALT) едлмйд (мфй шоъ дчшйаийрйп), етм шоеъ двмечеж ефшефйм щеорй дгн. осчръ дзечшйн дйъд лй лешлен дрцшк бъжерд тщей мдйеъ йтйм бдфзъъ вешойн оеиврйн еборйтъ сшип.
https://www.ncbi.nlm.nih.gov/pubmed/1579064
озчш чмйрй ма обечш (1998) бзп аъ йтймеъ дийфем баоцтеъ лешлен морйтъ сшип дзк бтчбеъ тйщеп дфек (reverse smoking)*. роца щцшйлъ лешлен бойреп щм 1 вшн мйен бощк ъщтд зегщйн дфзйъд боебдч аъ осфш дрвтйн дишен сширййн.
* ордв дегй щм дзжчъ дчцд дбетш щм дсйвшйд бъек дфд.
https://www.ncbi.nlm.nih.gov/pubmed/9863273
ийфем
бсчйшд (2022) оцйвйн дзечшйн аъ дооцайн дфшд-чмйрййн дтесчйн бйтймеъ щм лешлеойп бдфзъъ ддщфтеъ дщмймйеъ щм лйоеъшфйд осев цйсфмаийп ебщйфеш йтймеъ дийфем. дзечшйн оцййрйн лй дийфем бцйсфмаийп отегг фвйтд б-DNA еафефиежйс щм ъайн сширййн, аемн тмемеъ мдйеъ ме дщфтеъ щмймйеъ тм айбшй двеу ебочшйн шбйн оъфъзъ тойгеъ мийфем дъшефъй. озчшйн фшд-чмйрййн ечмйрййн дгвйое лй млешлеойп фтймеъ ревгъ сшип дъешоъ морйтъ дъфъзеъ двйгем. босвшъ дсчйшд оцйвйн дзечшйн аъ орврерй дфтемд щм цйсфмаийп еофшийн лйцг дщйоещ блешлеойп тщей мъшен мдфзъъ ддщфтеъ дщмймйеъ бдъййзс мфтймеъ щм отшлъ дтцбйн, дмб, длбг, длмйеъ ефвйтд бщойтд. бдощк, оецвйн ооцайн мвбй дъфчйг щм лешлеойп бдвбшъ йтймеъ дийфем еборйтъ тойгеъ мийфем, еоцйвйн аъ дщйоещ брре-змчйчйн долймйн лешлеойп ецйсфмаийп, мийфем ооечг бвйгем дсширй.
дзечшйн ослойн лй оцибшеъ тгейеъ дошаеъ щдфтймеъ ревгъ дзоцеп еревгъ дгмчъ щм лешлеойп осййтъ мдфзъъ ддщфтеъ дщмймйеъ щм лйоеъшфйд осев цйсфмаийп емцоцен дфвйтд байбшй двеу.
https://pubmed.ncbi.nlm.nih.gov/34697839/
счйшд (2015) бзрд аъ лмм дтгейеъ бйзс мдщфтд дарий-сширйъ щм ъшлебеъ фремйеъ щереъ, ъек дъочгеъ блешлеойп, шжбшишем, айжефмберйн, EGCG, абчъ фим щзеш, ойцей аелорйеъ щзешеъ, ойцей в'йрв'ш еойцей шйоеп. оозчшй отбгд ебтмй зййн темд лй лешлеойп дйре дшлйб дъжеръй добийз бйеъш лийфем ъеок бсшип чемешчимй ларий гмчъй, ревг зоцеп, ощшд афефиежйс, оерт щвщев ргйгд ефмйщд щм ъайн еофзйъ ржчйн м-DNA. оъек 17 озчшйн чмйрййн шщеойн, ъщтд фешсое ешч зойщд оъелн дцбйте тм йтймеъ щм лешлеойп ае лешлеойреайгйн борйтъ ъдмйлйн ае дфзъъ сорйн дчщешйн бдъфъзеъсшип чемешчимй. дзечшйн сбешйн щдсйбд млк чщешд бжойреъ дбйемевйъ дроелд щм лешлеойп ебзесш дйцйбеъ длйойъ щме. дзечшйн ослойн лй баефп лммй озчшйн чмйрййн осфчйн ъойлд чмещд мвбй дйтймеъ щм ъшлебеъ фремйеъ лрвг сшип чемешчимй еосбйшйн лй ргшщйн ойрерйн вбедйн оаег тм оръ мвшен мдщфтд бтмъ ощотеъ чмйрйъ.
https://www.ncbi.nlm.nih.gov/25693744
озчш чмйрй ачшай лфем сойеъ еобечш фмсбе (2014) бзп аъ йтймеъ дийфем бсшип баоцтеъ ъесу лешлеореайгйн доъеесу мийфем длйоеъшфй. щоерйн рбгчйн земй сшип бтмй вйгемйн оецчйн (solid tumors) доиефмйн бийфем лйоеъшфй земче ачшайъ мриймъ ъесу лешлеореайгйн тн жойреъ бйемевйъ ощефшъ (сев ойцей ма йгет) бойреп 180 о"в мйен ае фмсбе бощк щоерд щбетеъ. бъен ддътшбеъ роца лй ъесу длешлеореайгйн дйд йтйм йеъш боебдч офмсбе бщйфеш айлеъ дзййн щм дрбгчйн (p<0.001) ебдфзъъ (p<0.001) оггй дгмчъ TNFΑ, дфзъъ (p<0.001) вешн двгймд TGFβ, дфзъъ (p<0.001) дзмбеп длйоеичий моерецйийн MCP-1, CRP, едфзъъ (p=0.005) оггй длаб substance P, едфзъъ (p<0.001) дффийг дчщеш мвп дчмцйиерйп CGRP. бресу, мъесу длешлеореайгйн рцфд йъшеп ма оебдч (p=0.061) тм фрй фмсбе бдфзъъ шоъ дцйиечйп дфше гмчъй IL-6. тн жаъ, мфмсбе рцфд йъшеп оебдч (p=0.012) тм фрй ъесу длешлеореайгйн бдфзъъ шоъ дцйиечйп IL-8.
https://www.ncbi.nlm.nih.gov/pubmed/24648302
озчш чмйрй ачшай обечш фмсбе (2011) бзп аъ йтймеъ лешлеойп бийфем бсшип дотй двс едзмземъ. 126 рбгчйн щаебзре лсебмйн осшип дотй двс едзмземъ мфрй рйъез земче ачшайъ мриймъ лешлеойп (сев ойцей ма цейп) бойреп 1080 о"в мйен ае фмсбе мощк 10-30 йойн. роца щриймъ лешлеойп дтмъд аъ ощчм двеу щм дрбгчйн (p<0.05), дфзйъд (p<0.05) аъ шоъ д-TNFɑ, дтмъд аъ бйией двп ревг двйгемйн p53 бшчоъ двйгем (p<0.05) едвбйшд афефиежйс щм ъайн сширййн (p<0.05) бдщееад мфмсбе.
https://www.ncbi.nlm.nih.gov/pubmed/21314329
озчш чмйрй бмъй обечш (2001) бзп аъ йтймеъ ойцей лешлен бийфем бсшип дотй двс едзмземъ. 15 рбгчйн тн сшип дотй двс едзмземъ бщмб оъчгн щма овйб мийфем лйоеъшфй иефме бъоцйъ ъчрйъ щм лешлен бойреп демк етемд щм 440-2200 о"в мйен (ойреп щеед тшк м-36-180 о"в лешлеойп) бощк 2-4 зегщйн. бтчбеъ дийфем дещвд озмд йцйбд бзойщд одоиефмйн едфзъд ощотеъйъ бшоеъ дарийвп дчшцйреаобшйерй (огг мооайшеъ ботшлъ дтйлем) боиефм азг.
https://www.ncbi.nlm.nih.gov/pubmed/11448902
озчш чмйрй ма обечш (2008) бзп аъ ддщфтд дарий гмчъйъ едарий сширйъ щм лешлеойп бчшб земйсшип мбмб оъчгн. тщшйн езойщд рбгчйн дземйн бсшип мбмб оъчгн риме лешлеойп бойреп 8 вшн мйен тг мдъчгоеъ дозмд, лащш блм зегщййн щмб дозмд детшк озгщ. 21 рбгчйн дщмйое аъ ддътшбеъ. оъелн риймъ лешлеойп дгвйод йтймеъ чмйрйъ оебдчъ бщрй оиефмйн бмбг: базг одн дещвд озмд йцйбд мощк мотмд о-18 зегщйн ебщрй змд рсйвд чцшъ иеез ак ощотеъйъ бвйгем (73%) мцг тмйд оебдчъ (фй 4-35) бшоеъ дцйиечйрйн бсшен (IL-6, IL-8, IL-10 е-IL-1). лешлеойп дгвйн ау дгвйн фтймеъ ревгъ гмчъ тм йгй дфзъъ дбйией дврий щм NFkB, Cox2 етйлеб осмем дайъеъ щм вешн дщтъеч STAT3 бъайн доереречмйашйн бгвйоеъ дгн дфшйфшйеъ щм дрбгчйн (щдйе оевбдйн мфрй ддътшбеъ бдщееад мрбгчйн бшйайн). риймд феойъ щм лешлеойп рсбмд дйиб ак рцфъд щереъ вбедд бжойреъ дбйемевйъ щм лешлеойп бчшб дрбгчйн.
https://www.ncbi.nlm.nih.gov/pubmed/18628464
бозчш фйймеи чмйрй ачшай лфем-сойеъ обечш фмсбе (2017) рбгчд ддщфтд щм ийфем бшлйбйн ибтййн (лешлен, шжбшишем, ъд йшеч ербий бшечемй) тм чцб тмййъ догг PSA бчшб вбшйн тн дйщреъ бйелйойъ щм сшип дтшоерйъ, доаефййрйн бтмййд бйрерйъ б-PSA. бозчш дщъъфе 22 вбшйн тн жоп длфмъ PSA щм 4-15 зегщйн емма тгеъ мвшешеъ. дрбгчйн земче ачшайъ мчбецъ дийфем ае мчбецъ дфмсбе мощк 12 щбетеъ. дийфем лмм риймъ 4 ибмйеъ мйен оъесу ибтй долйм 100 о"в лешлеойп, 30 о"в шжбшишем е-100 о"в ъд йшеч мибмйд, елп 4 лоесеъ мйен щм рбий бшечемй ошелжйн (щеед тшк м-8 вшн мйен рбийн ишййн). бъен ддътшбеъ роца лй дтойгд бфшеиечем дозчш дййъд иебд оаег едийфем рсбм дйиб, мма дбгм бйп дчбецеъ бйзс мдщфтеъ дщмймйеъ.
дзечшйн оцййрйн лй ма дййъд цйфййд бозчш дфйймеи мдбгмйн оебдчйн бйп дчбецеъ бйзс м-PSA емоггйн дчмйрййн. тн жаъ, брйвег моцефд, бчбецъ дийфем роцад дзошд бжоп длфмъ д-PSA, ак дзечшйн оцййрйн лй ддбгм айре оебдч сиийсийъ еиеез дитеъ дйре вгем лк щдн оцйтйн мдощйк ембзеп аъ дщфМтъ ъесфйн амд бозчш обечш бдйчу вгем йеъш.
https://www.ncbi.nlm.nih.gov/pubmed/28181675
озчш чмйрй ма обечш (1987) бзп аъ йтймеъ лешлен бриймд феойъ ебошйзд зйцерйъ бдчмд тм ъсойрйсшип дфд емейчефмчйд (рвтйн ишен сширййн доъафййрйн бщлбд мбрд отебд бшйшйъ змм дфд). 62 рбгчйн тн сшип ае рвтйн ишен сширййн бзмм дфд щма двйбе мийфем дчербрцйермй риме ойцей аъремй щм лешлен (шйлеж дойцей еойреп дриймд айрн йгетйн) ебресу ошзе ощзд долймд лешлеойп тм вбй дрвтйн. роца щдийфем баоцтеъ дойцей едощзд дфзйъе аъ дшйз дрмеед мрвтйн б-90% одочшйн едфзйъе аъ двшг еддфшщеъ лоти блм дочшйн. рвтйн йбщйн рцфе б-70% одочшйн, ак тецоъ длаб етебй дрвтйн фзъе шч б-10% одочшйн. бчшб шбйн одрбгчйн дщАфтъ дийфем рощлд осфш зегщйн мазш дфсчъе. ъвебъ мееай ма шцейд рцфъд шч боиефм азг.
https://www.ncbi.nlm.nih.gov/pubmed/2435036
дфзъъ ъефтеъ мееай
бсчйшд щйиъйъ (2020) отшйлйн дзечшйн аъ дйтймеъ дийфемйъ щм цозй ошфа, доелшйн тм йгй отшлъ дбшйаеъ ббшжйм, мдчмд тм ъефтеъ дмееай щм ийфемйн ревгй сшип (лйоеъшфйд ешгйеъшфйд). бсчйшд рлмме 29 озчшйн ачшаййн обечшйн, ащш ртшле б-15 огйреъ (9 одозчшйн ртшле байшап). бозчшйн амд детшле 12 цозй ошфа ае щймебйн щерйн обйп 71 дцозйн доелшйн ботшлъ дбшйаеъ дбшжймайъ: алймад аму дтмд (Achillea millefolium), щен (Allium sativum), амеешд (Aloe vera), чоеойм (Matricaria (Chamomilla) recutita), цйфешрй зъем (Calendula officinalis), лешлен (Curcuma longa), сейд (Glycine max), в'йрв'ш (Zingiber officinale), ртрт зшйфд (Mentha x piperita), емзк вгем (Plantago major).
мдмп дооцайн дтйчшййн бдъййзс млйоеъшфйд:
- обйп дозчшйн бдн детшлд дйтймеъ щм в'йрв'ш мдчмд тм бзймеъ едчаеъ, 6 озчшйн дцбйте тм дйтймеъ щм в'йрв'ш мбг ае бщймеб тн чоеойм лийфем ощмйн, мтеоъ 6 озчшйн бдн ма роцад йтймеъ оебдчъ.
- в'йрв'ш роца йтйм вн мдчмд тм тцйшеъ.
- бдъййзс моечежйийс бфд, щийфеъ фд, добессеъ тм алймад ае тм чоеойм, роцае йтймеъ мийфем ае морйтд, аемн дщйоещ бмзк вгем ае бщймеб щм чоеойм еорид ма роца йтйм.
- ъесу сейд (MicrSoy-20) ъшн мщйфеш ъсойрй тййфеъ езесш ъйабеп.
- дщйоещ бщен ма роца йтйм морйтъ зен рейишефрй (зен домеед ойтеи ъай гн мбрйн).
мдмп дооцайн дтйчшййн бдъййзс мшгйеъшфйд:
- бщрй озчшйн щйоещ зйцерй бцйфешп зъем ае бамеешд ма роца йтйм морйтъ ъвебд тешйъ ае мийфем бд, бчшб земй сшип шащ ецееаш. аемн, бщрй озчшйн азшйн дщйоещ бцозйн амд роца йтйм морйтъ гшоийийс емийфем бе.
- мийфем боечежйийс бфд, бозчш азг роцад йтймеъ мщйоещ блешлен ебозчш азш дщйоещ бщийфъ фд добессъ тм амеешд ма роца йтйм.
- ощзъ амеешд дййъд йтймд мийфем бгмчъ фй дибтъ (фшечийийс), бчшб земйн тн сшип бажеш давп, елп мдчмд тм сйбелйн дчщешйн блк лвеп лаб, ъзещъ цшйлд ае чещй мдъшечп.
дзечшйн ослойн лй йщрп тгейеъ доцбйтеъ тм дйтймеъ щм цозй ошфа осейойн морйтд емийфем бъефтеъ дмееай дчщешеъ бийфем ревг дсшип, еблк мъшен мщйфеш айлеъ дзййн щм доиефмйн.
https://pubmed.ncbi.nlm.nih.gov/32147034/
озчш чмйрй обечш (2014) бзп аъ йтймеъ ебийзеъ дщйоещ бъесу лешлеойп фесфемйфйгй (Meriva) мийфем бъефтеъ дмееай дребтеъ оийфемйн лйоеъшфййн ешгйеъшфййн бсшип. бозчш дщъъфе 160 рбгчйн земйсшип брй 35-70 мазш рйъез доевгшйн боцб вефрй рфщй еъфчегй иеб (цйеп щм 70 еотмд бсемн чшрефсчй) мма озмеъ мб, селшъ ае ъсоеръ оибемйъ, дтебшйн ийфемй лйоеъшфйд (5-fluorouracil, cisplatin, vinblastine, gemicitabine, CCNU, MOPP/ABVD/COPP) (сдл 80 рбгчйн) ешгйеъшфйд (80 рбгчйн). дрбгчйн земче ачшайъ мриймъ ъесу лешлеойп фесфемйфйгй (долйм 100 о"в лешлеореайгйн бйзс DMT:BDMT:curcumin щм 1:8:33 бдъаод е-200 о"в мцйийп сейд) бойреп 1500 о"в мйен ае фмсбе бощк тг ашбтд зегщйн (оъелн мфзеъ 60 йойн бшцйфеъ). 158 рбгчйн дщмйое аъ ддътшбеъ (2 рбгчйн очбецъ длйоеъшфйд рщше осйбеъ мевйсийеъ щайрп чщешеъ мийфем). бчбецъ длйоеъшфйд риймъ лешлеойп дфзйъд боебдч аъ ъефтеъ дмееай щм дийфем бдщееад мчбецъ дбйчешъ: бзймеъ едчаеъ, щмщем ае тцйшеъ, аебгп ъабеп ейшйгд бощчм, фвйтд бжлшеп ае щйреййн чеврйийбййн, швйщеъ мжйдеойн/амз гн, рейишефрйд, ъсойрйн щм фвйтд мббйъ, цешк бриймъ ъшефеъ мийфем бъефтеъ дмееай (p<0.05). бресу, лешлеойп дфзйъ боебдч аъ дтчд дзоцерйъ бгон щм дрбгчйн бтчбеъ дийфем бдщееад мчбецъ дбйчешъ (P<0.022) ебдщееад моцб дбсйс (p<0.021). бчбецъ дшгйеъшфйд риймъ лешлеойп дфзйъд боебдч аъ ъефтеъ дмееай щм дийфем бдщееад мчбецъ дбйчешъ: фвйтд бшчоеъ афйъм, фвйтд бфд, вшеп ещи еотййн, лабйн елйбйн бфд ебвшеп, чещй ббмйтд, лабйн бещи, щмщемебзймд, рфйзеъ/бцчъ бвфййн дъзъереъ, тййфеъ лммйъ, земщд, цешк бъшефеъ мийфем бъефтеъ дмееай (p<0.05). бресу, лешлеойп дфзйъ боебдч аъ дтчд дзоцерйъ бгон щм дрбгчйн бтчбеъ дийфем бдщееад мчбецъ дбйчешъ (P<0.022) ебдщееад моцб дбсйс (p <0.021). дийфем баоцтеъ лешлеойп рсбм дйиб едйд рием ъефтеъ мееай.
https://www.ncbi.nlm.nih.gov/pubmed/23775598
озчш чмйрй ачшай лфем сойеъ еобечш фмсбе (2013) бзп аъ йтймеъ лешлеойп бдфзъъ гмчъ теш зоешд дребтъ оийфемй шгйеъшфйд (severe radiation dermatitis) бземеъ сшип дщг. 30 рбгчеъ (вйм ооецт 58.1) дземеъ бсшип щг доевгш лсшип щг ма гмчъй ае чшцйреод in situ едоиефмеъ бийфемй шгйеъшфйд (мма лйоеъшфйд) земче ачшайъ мриймд феойъ щм лешлеойп бойреп 6 вшн мйен ае фмсбе бодмк дийфемйн. бъен ддътшбеъ роца лй лешлеойп дфзйъ боебдч аъ зеошъ дгмчъ (мфй огг RDS) бдщееад мфмсбе (p=0.008). щйтеш дрбгчеъ щсбме очймеу мз щм дтеш (moist desquamation) бтчбеъ дийфем дйд роек йеъш боебдч бчбецъ длешлеойп бдщееад мчбецъ дфмсбе (28.6% мтеоъ 87.5%, p=0.002).
https://www.ncbi.nlm.nih.gov/pubmed/23745991
озчш чмйрй (2013) дщееаъй ачшай зг сойеъ еобечш бзп аъ дйтймеъ щм лешлен морйтд едчмд тм оечежйийс бфд лъефтъ мееай щм ийфемй чшйрд ае лйоеъшфйд бземй сшип шащ ецееаш. 80 земйн земче ачшайъ мчбмъ лешлен мвшвеш (абчъ лешлен бойреп 400 о"в оеосъ б-80 о"м ойн оешъзйн еоцеррйн, ойреп мщийфд 10 о"м оп дъойсд) ае ийфем ъшефъй (фебйгеп йегйп) бодмк ийфемй дчшйрд/ лйоеъшфйд. бозчш роца лй щийфъ фд долймд лешлен йтймд йеъш одийфем дъшефъй мгзййд емдфзъъ оечежйийс бфд (p<0.001), лое вн мщойшд тм сгйшеъ дийфемйн башбтъ дщбетеъ дшащерйн мийфем (p<0.01) (отбш машбтд щбетеъ, ма рцфд дбгм оебдч бйп дчбецеъ) ещойшд тм ощчм двеу (p<0.001).
https://www.ncbi.nlm.nih.gov/pubmed/24165896
озчш чмйрй ачшай еобечш (2014) бзп аъ дйтймеъ щм абчъ лешлен бщймеб тн гбщ морйтд едчмд тм оечежйийс бфд лъефтъ мееай щм ийфемй чшйрд ае лйоеъшфйд бземй сшип. 60 рбгчйн земче мчбецъ дътшбеъ щиефмд бошйзд зйцерйъ щм абчъ лешлен егбщ тм дрвтйн емчбецъ бйчешъ щма иефмд бощк тщшд йойн. бъен ддътшбеъ рцфд йъшеп оебдч мийфем бдщееад моцб дбсйс емчбецъ дбйчешъ (p<0.05).
https://www.ncbi.nlm.nih.gov/pubmed/26182820
озчш чмйрй ма обечш (2013) бзп аъ йтймеъ ебийзеъ дщйоещ бълщйш мщийфъ дфд долйм лешлеойп (Curcumall) мийфем боечежйийс щм дфд бтчбеъ ийфемй лйоеъшфйд обессъ doxorubicin бчшб ймгйн земй сшип. щбтд ймгйн ертшйн земй сшип брй зощ еотмд (бърай щиефме бйзйгд даерчемевйъ фйгйаишйъ, вйм ооецт 15.2) вшвше 20 ийфеъ мйен щм ълщйш мщийфъ дфд (щдлйм ъоцйъ лешлеойпC3 бшйлеж 95% еойцеййн щм лешлен ев'йрв'ш оеосйн бвмйцшйп ебамледем бшйлеж 0.4%, ойреп щеед тшк м-330 о"в лешлеойп мйен) бресу мълщйш мщийфъ дфд дсиргший chlorhexidine 0.2% бодмк ийфемй длйоеъшфйд бощк 21 йойн. ашбтд оъек зойщд рбгчйн фйъзе оечежйийс щм дфд ак бгшвъ зеошд чмд. бчшб лм дашбтд зеошъ доечежйийс фзъд бдщееад моцб ддъзмъй емзеошд догеезъ дсфшеъ. дзечшйн оцййрйн лй бдтгш чбецъ бйчешъ ма рйъп мйзс аъ дъецаеъ млешлеойп беегаеъ ема моафййп азш щм даелмесйд лвеп дъзгщеъ ъайн одйшд бчшб ймгйн.
https://www.ncbi.nlm.nih.gov/pubmed/23709456
озчш фйймеи ма обечш (2015) бзп дан дщймеб щм цозй ошфа дйгетйн лотешшй ъйабеп осййтйн мдфзъъ арешчсйд бземй сшип оъчгн, щайрн оиефмйн блйоеъшфйд. бозчш дщъъфе 17 земйн ащш риме 1 вшн в'йрв'ш (Zingiber officinalis) е-1 вшн лешлен (Curcuma longa) фтоййн бйен, елп 1 о"м ойцей амледемй щм в'рийап (Gentiana lutea) щмещ фтойн бйен, мощк 14 йойн. 3 земйн ресфйн риме в'йрв'ш елешлен бойрерйн ждйн, мма в'рийап. оъек 20 дощъъфйн, шч 7 сййое 14 йой ийфем; щаш дощъъфйн дфсйче аъ дийфем мазш лод йойн, бтйчш бщм ъефтеъ мееай. ъефтъ дмееай дщлйзд бйеъш дййъд бзймд, лащш дощъъфйн гйеезе вн тм дчаеъ, земщд, щмщем езесш резеъ ббип. йъшд олк, дийфем ма роца йтйм мщйфеш дъйабеп. дзечшйн оцйтйн лй бозчшйн тъйгййн йщ мцоцн аъ дшлйбйн ае дойрерйн тм оръ мдфзйъ аъ ъефтеъ дмееай.
https://www.ncbi.nlm.nih.gov/pubmed/25324460
зжшд мъзймъ дозчшйн
фМишййъ шййщДй
счйшеъ | озчшйн чмйрййн
счйшеъ
бсчйшд щйиъйъ щм озчшйн чмйрййн (2020) детшлд ддщфтд щм биа-вмечп, доефч офишйеъ, лийфем ощмйн бчшб земй сшип дочбмйн ийфем ревг сшип чербрцйерамй. бсчйшд рлмме 16 озчшйн бдн 1,650 земйн доаебзрйн тн ъщтд севй сшип.
бозчшйн амд дщъоще ббиа-вмечп, доефч осевйн щерйн щм щошйн ефишйеъ, лащш дййъд щереъ вгемд бйп дозчшйн бойреп, аефп дриймд, еощк ддътшбеъ. баефп лммй роца щдщйоещ ббиа-вмечп дйд биез ерсбм дйиб. бшеб дозчшйн роца лй риймъ биа-вмечп бочбйм мийфемй лйоеъшфйд ае шгйеъшфйд дййъд омеед бойъеп дгйлей дзйсерй е/ае бдацъ дщйчен щм ъай дгн дмбрйн. йзг тн жаъ, бзмч одозчшйн ма роцад дщфтд оебдчъ.
ддщтшд дйа, щау тм фй щбиа-вмечп деа сйб щайре оътлм, ддщфтд щме дйа гшк чщйшд мъай арийвп (APC) ботй дгч, гбш двешн мъайн амд мщфш аъ фтймеъ дотшлъ дзйсерйъ.
дзечшйн ослойн, лй бщм ддишеврйеъ бйп дозчшйн егйеез змчй щм дръерйн, ма рйъп мчбет осчрд бшешд, ергшщйн озчшйн ресфйн мдтшлъ дйтймеъ щм биа-вмечп лийфем ощмйн бчшб земй сшип.
https://pubmed.ncbi.nlm.nih.gov/33309412/
оаош счйшд щйиъйъ (2012) бзп аъ дйтймеъ едбийзеъ щм дщйоещ бфишййъ шййщй (Ganoderma lucidum) босвшъ дийфем бземй сшип, елп ддщфтд тм ддйщшгеъ миеез дашек, тм ъвебъйеъ двйгем, тм дъфчег дзйсерй етм айлеъ дзййн щм доиефмйн. бсчйшд рлмме 5 озчшйн чмйрййн ачшаййн обечшй ийфем чербрцйермй (лйоеъшфйд/шгйеъшфйд) ае фмсбе щтсче блм севй дсшип еблм щмбйе.
боид-армйжд щртшлд тм дръерйн роца щбдщееад моиефмйн щчйбме ийфемй лйоеъшфйд/шгйеъшфйд бмбг, амд щриме бресу вн фишййъ шййщй (шйлежй дойцеййн еойрерйдн ма йгетйн) дйе бтмй сйлей вбед бл-50% мъвебд зйебйъ мийфем (p=0.02). лое лп, щйоещ бфишййъ шййщй бмбг дйд фзеъ йтйм одийфем дощемб. ма йгетд йтймеъ дийфем баоцтеъ шййщй бмбг мтеоъ йтймеъ дийфем дчербрцйермй мбге дйеъ щдоаош дочешй рлъб бсйрйъ еайре жойп мчшйад. лое лп, роца щриймъ фишййъ шййщй щйфшд аъ дъфчег дзйсерй (дтмъд аъ щйтеш ъай д-T осев CD3, CD4 е-CD8 б- 3.91%, 3.05% е- 2.02% бдъаод, p<0.01-0.03). шоеъ дмейчецйийн, фтймеъ ъай д-NK ейзс CD4/CD8 доцййп аъ зежч дъвебд дзйсерйъ тме бойгд ожтшйъ (шч дтмйд бйзс д-CD4/CD8 дйъд оебдчъ, p=0.03).
ашбтд озчшйн дцйве щйфеш байлеъ зйй дрбгчйн бтчбеъ дийфем бдщееад мчбецеъ дбйчешъ. ма рцфъд дщфтд щм дийфем бфишййъ шййщй тм вегм двйгемйн. дийфем тм фй шеб рсбм дйиб, озчш азг геез тм ъефтеъ мееай щемйеъ, бйрйдп бзймд ергегй щйрд. ма рцфъд штймеъ ощотеъйъ бгн ае блбг бтчбеъ дийфем.
дзечшйн ослойн лй роцад ъойлд мйтймеъ щм фишййъ шййщй лийфем ъеок мщйфеш дъвебд мийфем длоеъшфй ае дшгйеъшфй едфтймеъ дзйсерйъ. йзг тн жаъ, ма роцае тгейеъ доцгйчеъ щйоещ бфишййъ шййщй лийфем че шащеп бземй сшип еайп осфйч тгейеъ мдтшлъ ддщфтд тм ддйщшгеъ миеез дашек. дзечшйн оцййрйн лй баефп лммй дайлеъ доъегемевйъ щм дозчшйн дйрд роелд егйеез дъецаеъ мечд бзсш.
https://www.ncbi.nlm.nih.gov/pubmed/22696372
счйшд (2016) бзрд аъ йтймеъ риймъ шййщй бийфем бсшип. бсчйшд рлмме зойщд озчшйн щртшле бчшб 373 рбгчйн земй сшип едщее аъ йтймеъ шййщй бийфем бсшип бдщееад мфмсбе ае мийфем арий сширй. щмещд озчшйн лмме рбгчйн тн сшип шйаеъ оъчгн, озчш азг лмм рбгчйн щтбше рйъез бтчбеъ сшип дзмземъ еозчш ресу лмм рбгчйн тн севй сшип щерйн. шеб дозчшйн рощле 1-3 зегщйн, ак ощк ддътшбеъ едойрерйн дсфцйфййн щм шййщй ма дйе бшешйн. дайлеъ доъегемевйъ щм дозчшйн дйъд роелд тг роелд оаег бщм дтгш ойгт тм ачшайеъ ае щйек мчбецеъ дийфем ебщм огвойн чирй дйчу. лое лп, бочшйн осейойн дйд зесш тчбйеъ бооцайн. тм сок дтгейеъ дчййоеъ, йълп щдийфем бсшип баоцтеъ шййщй тщей мщфш аъ сйлейй дъвебд мийфем дъшефъй ак ооца жд айре зг ощотй. йълп щшййщй ощфшъ аъ дъвебд дзйсерйъ щм двеу, ебййзег аъ ъвебъ ъай д-T (башбтд озчшйн щртшле бчшб 213 рбгчйн рцфъд тмйд щм 2-4% бфтймеъ ъай д-T) ак дщфМтъ шйщй тм фтймеъ ъай NK айрд егайъ (оъек щрй озчшйн щртшле бчшб 89 рбгчйн, озчш азг дгвйн двбшд щм фтймеъ NK еозчш щрй дгвйн аъ ддйфк). лое лп, йълп щшййщй ощфшъ аъ айлеъ зйй дрбгчйн, баефп рием ае лоти рием ъефтеъ мееай (бозчш йзйг щмещд рбгчйн гйеезе тм дефтъ бзймеъ ергегй щйрд бтчбеъ риймъ шййщй) дозчшйн щрлмме бсчйшд дн чцшй иеез ема бзре аъ щйтешй дщшйгеъ бчшб земй дсшип додеейн огг зщеб мйтймеъ дийфем. дзечшйн оцййрйн лй йълп щшййщй йтймд йеъш бщймеб тн ийфемйн азшйн бсшип мтеоъ шййщй мбгд, ак рзецйн тег озчшйн лгй мащщ аъ дооцайн.
https://www.ncbi.nlm.nih.gov/pubmed/28083078
оаош счйшд (2005) гп бдщфтд дарий сширйъ щм фишййъ дшййщй дп бийфем едп борйтд лфй щрцфъд бозчшй отбгд еозчшй бтмй зййн щерйн елп бозчшйн чмйрййн тм земй сшип. тм ау дфеирцйам двмен бфишййъ дшййщй бийфем бземй сшип, тг мфшсен доаош ма делзд фтймеъ арий сширйъ йщйшд щм дфишййд. тм фй дсчйшд щрй озчшйн чмйрййн ачшаййн обечшй фмсбе еозчш азг фъез геезе тм двбшд щм дъвебд дзйсерйъ дъайъ етм тмйд бъвебъйеъ дойиеврйъ щм ъай отшлъ дзйсеп (mitogenic reactivity) бчшб земй сшип осевйн щерйн. бозчш азш айлеъ дзййн щм 65% оземй сшип дшйад дщъфшд бойгд обедчъ. рлеп мжоп фшсен доаош, дфтймеъ дцйиеиечсйъ едарий-арвйеврийъ* дйщйшд щм фишййъ дшййщй делзд шч бозчшй отбгд еишн рчбт ойреп афчийбй мийфем бземй сшип отбш мийфем дъеок.
*орйтъ дйеецшеъ лмй гн згщйн.
https://www.ncbi.nlm.nih.gov/pubmed/16351502
оаош счйшд (2013) гп бфтймеъ дарий сширйъ щм дшлйбйн дишйишфреайгйн щм шййщй. оозчшйн фшд-чмйрййн темд лй мишйишфреайгйн щоеце ошййщй фтймеъ арий сширйъ шзбд длеммъ фтймеъ цйиеиечсйъ йщйшд (тйлеб даржйн имеошаж едщшййъ ржч м-гра), тцйшъ озжеш дзййн щм дъайн дсширййн едщшййъ афефиежйс (босмем фрйой-ойиелергшйамй езйцерй-бдщфМтъ вешой вйгем едешоерйн щерйн) еаеиефвйд, орйтъ арвйевржд ефмйщъ ъайн сширййн егйлей дъфъзеъ вшешеъ, елп тм йгй фтймеъ ревгъ гмчъ еревгъ зоцеп. орврерй дфтемд леммйн бйп дйъш: чйщеш мзмберй 14-3-3 доеесъйн ъдмйлй щвщев ъайн еафефиежйс, тйлеб осмемй дайъеъ MAPK, ERK, AKT, JNK, FAK еосмемй дщтъеч щм AP-1 е-NFkB, ейсеъ бйией врйн отеггй щвщев, арвйевржд, ргйгд, дцогеъ ефмйщд щм ъайн сширййн (лвеп MMP-2,9, uPA, VEGF, TGFβ,c-Myc, IL-8), дфтмъ осмем дайъеъ щм змбеп Nrf2 едвбшъ бйией врйн щм змберйн дощъййлйн мотшк ддврд офрй тчд зоцерйъ бъайн.
https://www.ncbi.nlm.nih.gov/pubmed/23790022
оаош счйшд (2004) гп бдщфтеъ оажреъ зйсеп еревгеъ вйгемйн щм фишййъ дшййщй (Ganoderma lucidum). озчшй отбгд еозчшй бтмй зййн шбйн омогйн лй мфишййъ дшййщй йлемъ ейсеъ щм шлйбйн шбйн ботшлъ дзйсеп лвеп ъайн оцйвй арийврйн, ъай NK, емйофецйийн осев T е-B. дойцей дойой едрвжшъ дфемйслшйгйъ щм фишййъ дшййщй дцйве дщфтд ревгъ вйгемйн оебдчъ блод озчшй бтмй зййн щдещше бдн вйгемйн. ддщфтд ревгъ двйгемйн йезсд бтйчш мдвбшъ фтймеъ отшлъ дзйсеп.
мазшерд геез лй дойцей дамледемй едрвжшъ дишйишфрйъ щм фишййъ дшййщй дп бтмй дщфтд ревгъ вйгемйн, ллм дршад баоцтеъ фтймеъ цйиеиечсйъ йщйшд. озчш шащерй огеез тм орйтъ дйеецшеъ лмй гн згщйн бщйшеъ ъай дсшип (арий-арвйевржд) щллм дршад отешбъ бдщфтд ревгъ двйгемйн щм фишййъ дшййщй.
https://www.ncbi.nlm.nih.gov/pubmed/15525457
оаош счйшд (2015) бзп аъ дтгейеъ мвбй дщйоещ бъесфй ъжерд ецозйн дрйимйн баефп феой бчшб земеъ сшип дщг. дзечшйн бзре аъ дъшеод щм ъесфйн ибтййн мдчмд тм ъсойрй дозмд еъефтеъ дмееай щм дийфем, мщйфеш айлеъ дзййн, мщйфеш дбшйаеъ двефрйъ едшвщйъ емщйфеш щйтеш ддйщшгеъ едъоеъд. бсчйшд рлмме 22 озчшйн досфчйн ъойлд мщйоещ бвеашрд (Paullinia cupana) ебфишййъ шййщй (Ganoderma lucidum) мдчмд тм ъщйщеъ ебвмеиойп мщйфеш оечежйийс бфд. баефп лммй, дтгейеъ дйрп оевбмеъ еайрп оафщшеъ мвбщ домцеъ чмйрйеъ бшешеъ мвбй дйтймеъ едбийзеъ щм ъесфйн щерйн мземеъ сшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/25811312
озчшйн чмйрййн
озчш чмйрй ачшай еобечш (2017) бзп аъ ддщфтд дарий сширйъ еоеесъъ дзйсеп щм фишййъ шййщй (Ganoderma lucidum) бщймеб тн ийфем лйоеъшфй бчшб земеъ сшип дщг. 40 рщйн дсебмеъ осшип дщг земче ачшайъ мчбмъ ийфем лйоеъшфй мбге ае ийфем лйоеъшфй бщймеб тн риймъ ойцей фишййъ шййщй (сев дойцей ма цейп) бойреп 2000 о"в мйен мощк ашбтд озжешй ийфем лйоеъшфй. гвйоеъ гн рйиме оп дрбгчеъ мфрй еазшй ддътшбеъ. бчшб дрбгчеъ щиефме бийфем дощемб рцфъд тмйд щм фтймеъ зйсерйъ арий сширйъ щбад мйгй бйией бтмйд оебдчъ бшоъ дайришфшеп воа бсшен (p=0.0024) ебовоъ тмйд ма оебдчъ бшоъ дайришмечйп 8 щдре вешн лйоеичий доещк рейишефймйн евшремецйийн еодеед соп мфтймеъ фвецйийъ (p=0.019*). лое лп, бчшб дрбгчеъ дмме рцфъд йшйгд бгмчъйеъ щбад мйгй бйией бйшйгд оебдчъ бшоъ д-TNF амфа бсшен (p=0.0004) бдщееад моцб дбсйс. мтеоъ жаъ, бчшб дрбгчеъ щиефме бийфем лйоеъшфй мбге ма рцфд щйрей оебдч бшоеъ дцйиечйрйн дмме. лое лп, бщъй дчбецеъ ма рцфъд дщфтд оебдчъ тм шоъ дагйферчийп бсшен бтчбеъ ддътшбеъ бдщееад моцб дбсйс (чййн чщш дефлй бйп шоеъ агйферчийп мбйп ъдмйлйн сширййн).
* су доебдчеъ дчмйрйъ бозчш рчбт л-p<0.01.
https://oncologypro.esmo.org/Meeting-Resources/ESMO-Asia-2017-Congress/Ganoderma-Lucidum-has-immunostimulatory-and-antinflamatory-effect-in-breast-cancer-patients-4P
озчш чмйрй ачшай лфем сойеъ еобечш фмсбе (2012) бзп аъ йтймеъ дийфем баоцтеъ рбвй фишййъ шййщй (Ganoderma lucidum spore) бтййфеъ дребтъ одийфем даргечшйрй бчшб земеъ сшип дщг. 48 рбгчеъ земеъ бсшип дщг (бгшвд азъ тг щмещ) доиефмеъ бийфем аргечшйрй щйщд зегщйн мфзеъ еогеезеъ тм тййфеъ земче ачшайъ мчбецъ дътшбеъ ечбецъ бйчешъ. дрбгчеъ бчбецъ ддътшбеъ риме абчъ рбвй фишййъ шййщй бойреп 3 вшн мйен бощк ашбтд щбетеъ ечбецъ дбйчешъ римд фмсбе. бъен ддътшбеъ рцфд щйфеш оебдч бшоъ дтййфеъ (p<0.01), байлеъ дзййн дфйжйъ (p<0.01) едшвщйъ (p<0.05) ак ма дзбшъйъ, ебшоъ дъфчег догеезъ щм дрбгчеъ бтчбеъ дийфем бфишййъ шййщй. лое лп рцфд щйфеш бшоеъ дзшгд едгйлаеп догеезеъ щм дрбгчеъ (p<0.01). бчбецъ дбйчешъ ма рцфе щйреййн оебдчйн бау ма азг одоггйн. тег роца оъан бйп шоеъ дцйиечйрйн бсшен ебйп шоъ дтййфеъ щм дрбгчеъ. лое шоъ дтййфеъ, вн шоеъ дцйиечйрйн дфше гмчъййн TNF амфа еайришмейчеп 6 бсшен йшге бтчбеъ дийфем бшййщй (p<0.01 е- p<0.05 бдъаод) ак ма бтчбеъ дийфем бфмсбе. дийфем бшййщй рсбм дйиб мма дщфтд оебдчъ тм ъфчегй длбг едлмйеъ, ема геез тм ъефтеъ мееай ощотеъйеъ (моти сзшзешеъ ейебщ бфд) бтчбеъ дийфем.
https://www.ncbi.nlm.nih.gov/pubmed/22203880
озчш чмйрй ачшай обечш (2010) бзп аъ дщАфтъ ойцей ойой щм фишййъ шййщй (Ganoderma lucidum) тм вйгемйн щфйшйн ишен сширййн ботй двс ебзмземъ (Colorectal adenoma). дозчш лмм 225 рбгчйн тн вйгемйн щфйшйн ишен сширййн (агреоеъ) ботй двс едзмземъ ащш земче мчбецъ дътшбеъ (123 рбгчйн) ечбецд мма ийфем (102 рбгчйн). чбецъ ддътшбеъ римд ойцей ойой щм фишййъ шййщй бойреп 1.5 вшн мйен (ойреп щеед тшк м- 14 вшн фишййд ишййд) бощк 12 зегщйн. 96 рбгчйн бчбецъ ддътшбеъ дщмйое аъ дозчш. ббгйчъ чемересчефйд щбецтд бъен ъчефъ ддътшбеъ роца щойцей ойой щм фишййъ шййщй гйла аъ дъфъзеъ дагреоеъ ботй двс. рцфъд тмйд щм 0.66 босфш двйгемйн бчбецъ дбйчешъ, мтеоъ йшйгд щм 0.42 босфш двйгемйн бчбецъ дийфем дцозй (p<0.01). лое лп, вегм двйгемйн тмд б-1.73 о"о бчбецъ дбйчешъ ейшг б-1.40 о"о бчбецъ дийфем дцозй (p<0.01).
https://www.ncbi.nlm.nih.gov/pubmed/20518254
озчш чмйрй фъез (2006) бзп аъ дщфМтъ фемйслшйгйн щоеце ошййщй тм ъфчегйн зйсерййн бчшб земй сшип дотй двс едзмземъ бщмб оъчгн. 47 рбгчйн (вйм ооецт 48.4) дсебмйн осшип отй вс езмземъ бгшвд 3 е-4 щдийфем длйоеъшфй ае дшгйеъшфй дазшеп щмдн дйд мфрй мотмд озегщ ецйерн бсемн чшрефсчй мцйеп зеошъ дозмд 60 еотмд, иефме баоцтеъ дрвжшъ дфемйслшйгйъ щм шййщй (ойцей шййщй щдлйм 25% фемйслшйгйн) бойреп 5.4 вшн мйен (ойреп щеед тшк м-81 вшн фишййд) бощк 12 щбетеъ. бъен ддътшбеъ рбзре гвйоеъ щм ъайн оереречмашйн оп дгн дфшйфшй щм дрбгчйн. брйъез дъецаеъ рлмм ойгт щрасу о-41 рбгчйн (дщаш рщше оп дозчш ербгч азг рфиш). роца щийфем баоцтеъ шййщй двбйш бойгд ма оебдчъ аъ щвщев ъай дзйсеп мзеош дойиеврй фйиедоавмеирйп едтмд аъ сфйшеъ дмйофецйийн осев CD3, CD4, CD8 е-CD56 еаъ шйлеж дайришмечйрйн IL-2, IL-6 е-IFNɣ лое вн аъ фтймеъ ъай д-NK. мтеоъ жаъ дшйлеж бфмсод щм IL-1 е-TNFɑ фзъ ак бойгд ма оебдчъ. лм дщйреййн щзме боггйн дзйсерййн дйе ма оебдчйн бдщееад моцб дбсйс. лое лп, ма зм щйрей оебдч бйзс ъай д-T досййтйн едцйиеиечсйн CD4:CD8. тн жаъ, роца оъан оебдч бйп дщйреййн щзме бшйлеж IL-1 ебйп дщйреййн щзме б-IL-6, IFNɣ, CD3, CD4, CD8 ефтймеъ ъай д-NK баефп оебдч (p<0.05) елп роца оъан бйп дщйреййн щзме бшйлеж IL-2 ебйп дщйреййн щзме б-IL-6, CD8 ефтймеъ ъай д-NK. дзечшйн ъемйн аъ дтгш доебдчеъ бозчш бвегм догвн дчип ебщереъ двбедд бйп дрбгчйн.
https://www.ncbi.nlm.nih.gov/pubmed/16428086
озчш чмйрй шб ошлжй лфем сойеъ обечш фмсбе (2003) бзп аъ дйтймеъ едбийзеъ щм ълщйш цозй (®Ganopoly) тм дъфчег дзйсерй щм земйн бсшип шйаеъ оъчгн. Ganopoly дйа ъоцйъ ъчрйъ щм фишййъ шййщй (Ganoderma lucidum) оъечрръ мдлйм 25% фемйслшйгйн. 68 рбгчйн тн сшип шйаеъ щаещш ббгйчд дйсиемевйъ ема иефме бийфем арий сширй дщъъфе бозчш. дрбгчйн земче ачшайъ мчбмъ Ganopoly бриймд феойъ бойреп 1.8 вшн (ойреп щеед тшк м- 27 вшн фишййд)* ае фмсбе бощк 12 щбетеъ. роца щдийфем бфишййъ шййщй дйд йтйм йеъш боебдч офмсбе бтцйшъ дъчгоеъ дозмд (тцйшд бдъчгоеъ дозмд ршщод бчшб 35.1% одрбгчйн бчбецъ ддътшбеъ бдщееад м-22.6% бчбецъ дбйчешъ, шоъ доебдчеъ ма йгетд). лое лп, дийфем б- Ganopoly щйфш боебдч аъ ддтшлд дъфчегйъ щм дрбгчйн мфй семн чшрефсчй KPS-Karnofsky performance status (тмйд щм 10 рчегеъ бгйшев бчшб 50% одрбгчйн бчбецъ ддътшбеъ мтеоъ 14.3% бчбецъ дбйчешъ, p<0.05). щйтеш дрбгчйн щгйшев ддтшлд дъфчегйъ щмдн ма дщърд ае йшг дйд вбед йеъш бчбецъ дбйчешъ (46.4% е-39.3% бдъаод) бдщееад мчбецъ дийфем (28.1% е-21.9% бдъаод).
бресу, дийфем б-Ganopoly дйд йтйм йеъш боебдч бдщееад мфмсбе бщйлек ъсойрйн рмеейн мсшип лвеп зен, щйтем, земщд, джтеъ ергегй щйрд (щйтеш догеезйн тм щйфеш бъсойрйн бчбецъ ддътшбеъ дйд 84.4% ебчбецъ дбйчешъ 42.9%).
мбсеу, дийфем б-Ganopoly двбйш боебдч аъ дъвебъйеъ дойиеврйъ щм дъайн дмйофецйийн мзеош отегг дъзмчеъ, аъ фтймеъ ъай д-T еъай д-NK, едтмд аъ йзс д- CD4/CD8 (дотйг тм зежч дъвебд дзйсерйъ) бдщееад мфмсбе (p<0.05). ъефтеъ дмееай щгеезе бтчбеъ дийфем б- Ganopoly дйе бзймеъ ергегй щйрд.
*шае дтшъ дотшлъ мвбй Ganopoly.
https://researchbank.rmit.edu.au/view/rmit:19180
озчш чмйрй фъез ма обечш (2005) бзп аъ дщАфтъ ълщйш цозй (Ganopoly) тм дъфчег дзйсерй щм земйн бсшип шйаеъ оъчгн. Ganopoly дйа ъоцйъ ъчрйъ щм фишййъ шййщй (Ganoderma lucidum) оъечрръ мдлйм 25% фемйслшйгйн. 36 рбгчйн дземйн бсшип шйаеъ бгшвд 3 ае 4 риме Ganopoly бойреп 5.4 вшн мйен (ойреп щеед тшк м- 270 вшн фишйд)* бощк 12 щбетеъ бочбйм мийфемй лйоеъшфйд ае шгйеъшфйд. бчшб 30 дрбгчйн щсййое аъ дозчш, дийфем дцозй ма щйрд боебдч аъ дъвебъйеъ дойиеврйъ щм ъай отшлъ дзйсеп мфйиедовмеийрйп (мчийп дочещш мдвбшъ ойиежйс – змечд ъайъ), аъ сфйшъ ъай T осййтйн осев CD3-4-8-56, аъ шйлеж доъеелйн дзйсерййн бфмсод - IL2, IL-6, айришфшеп воа (IFN), еаъ фтймеъ ъай д-NK. тн жаъ рцфъд щереъ шбд бйп дрбгчйн езмч оземй дсшип дгвйое щйреййн оебдчйн бъфчег дзйсерй (p<0.05). осчръ дзечшйн дйъд щйълп щшч змч оземй дсшип овйбйн мийфем б-Ganopoly бщймеб ийфем лйоеъшфй ае дчшреъ.
*шае дтшъ дотшлъ мвбй Ganopoly.
https://www.ncbi.nlm.nih.gov/pubmed/16117607
озчш чмйрй фъез ма обечш (2003) бзп аъ дщАфтъ дрвжшъ дфемйслшйгйъ щм фишййъ дшййщй (Ganoderma lucidum) тм дъфчег дзйсерй бчшб земй сшип оъчгн. 34 рбгчйн (брй 45-64) дземйн бсшип оъчгн риме 5.4 вшн оп дълщйш Ganopoly, ъоцйъ ъчрйъ щм фишййъ дшййщй оъечрръ мфй 25% фемйслшйгйн (ойреп щеед тшк м-270 вшн фишйд)*, бощк 12 щбетеъ. ърай мдщъъфеъ бозчш дйд щдрбгчйн йдйе 12 щбетеъ мфзеъ мазш ийфем лйоеъшфй е-60 йен мазш ийфем шгйеъшфй. ръерй дъвебд дзйсерйъ щм 30 рбгчйн рбзре бъен ъчефъ ддътшбеъ. роца лй мълщйш дцозй йтймеъ осейоъ бщйфеш дъвебд дзйсерйъ. бтчбеъ риймъ дълщйш дцозй, змд тмйд оебдчъ бшйлеж дайришмейчерйн IL-2, IL-6 еайришфшеп воа бдщееад моцб дбсйс (p<0.05). бтег шоеъ д-IL-1 ед- TNF-alpha йшге боебдч (p<0.05). дщереъ бооцайн бйп дрбгчйн дйъд вбедд бйзс мсфйшеъ дмйофецйийн. бтчбеъ дийфем змд тмйд оебдчъ босфш ъай д-NK осев CD56+ (тмйд о- 238.3 м-277.4, p<0.05), ак дтмйд босфш ъай д-T осев CD3+, CD4+, CD8+ дйъд вбемйъ ейзс CD4/CD8 (огг доцййп аъ зежч дъвебд дзйсерйъ) реъш мма щйрей. лое лп, бчшб ошбйъ дземйн (80%) рцфъд тмйд бъвебъйеъ дойиеврйъ щм ъай отшлъ дзйсеп м-phytohemmaglutinin (мчийп дочещш мдвбшъ ойиежйс – змечд ъайъ) (p<0.05) етмйд бфтймеъ ъай д -NK бъецаеъ щм 34.5% мтеоъ 26.6% (p<0.05), бдщееад моцб дбсйс. бчшб 20% дреъшйн: дъвебъйеъ дойиеврйъ щм ъай отшлъ дзйсеп мфйиедовмеийрйп реъшд мма щйрей (6.7%) ае йшгд (13.3%).
*шае дтшд мвбй Ganopoly
https://www.ncbi.nlm.nih.gov/pubmed/12916709
озчш течбд (cohort) фшесфчийбй (2012) щртшк бсйп бзп аъ дчщш бйп дщйоещ бв'йрсрв ебфишййъ шййщй (Ganoderma lucidum) ебйп айлеъ дзййн щм земеъ сшип дщг мазш дабзеп бозмд. 4149 рщйн дщмйое 36 зегщй отчб отъ абзерп.
роца щрщйн щбзше базг дцозйн ма рие мйием аъ дцоз дщрй, емлп мцешк дсчйшд ръочг бгйеез тм дрщйн щриме аъ фишййъ дшййщй. лтбеш щйщд зегщйн оабзеп дозмд 58.8% одрбгчеъ геезе тм риймд щм фишййъ шййщй, елтбеш 36 зегщйн азеж дреимеъ аъ дфишйд тог тм 36.2%. одщееаъ ръерй дрбгчеъ щриме аъ дфишйд тн амд щма риме аеъд роца щдреимеъ аъ дфишйд дйе цтйшеъ еощлймеъ йеъш, рщеаеъ, бтмеъ длрсд вбедд йеъш, тн фзеъ озмеъ шчт, мазш дфсчъ десъ етн ъсойрй орефаежд. дп рие мфреъ мийфемй лйоеъшфйд ешгйеъшфйд емйием ейиойрйн, ма мтщп, дътоме бчбйтеъ еиефме бшфеад сйрйъ осешъйъ. бащш мчщш щбйп риймъ фишййъ шййщй еайлеъ дзййн, ма роца оъан оебдч бйп риймъ дцоз лтбеш зцй щрд ещмещйн ещйщд зегщйн ебйп айлеъ дзййн длммйъ ае айлеъ дзййн бдйби дфсйлемевй лтбеш 36 зегщйн. тн жаъ роца оъан зйебй оебдч (p<0.05) бйп айлеъ дзййн бдйби дзбшъй едлмлмй ебйп риймд чбетд щм фишййъ шййщй, еоъан щмймй оебдч (p<0.05) бйп айлеъ дзййн бдйби дфйжй ебйп риймд чбетд щм фишййъ шййщй. зежч доъаойн дещфт оъгйшеъ дриймд еоойреп дриймд доцибш (p<0.001 бщрйдн).
https://www.ncbi.nlm.nih.gov/pubmed/22745737
озчш фъез (1992)щртшк бчшб 48 оиефмйн ащш сбме осшип оъчгн (щг, чйбд, лмйеъ) ечйбме ийфем блйоеъшфйд ешгйеъшфйд ебочбйм шййщй (ойреп ма йгет) дгвйн ййцеб щм сфйшеъ гн мбреъ бдщееад мчбецъ дбйчешъ. лое лп, бчшб дчбецд дрбгчъ дегвн щйфеш бъйабеп ещйфеш лммй баршвйд мтеоъ чбецъ дбйчешъ. доиефмйн ащш ржчче мрйъез зее дъаещщеъ одйшд йеъш ещйфеш байзейй дфцтйн бдщееад мчбецъ дбйчешъ. фшийн ресфйн айрн йгетйн.
озчш сйрй щртшк бчшб 175 земйн ащш сбме омейчефрйд дшад тмййд бсфйшеъ дгн дмбреъ бчшб 72.5% одрбгчйн. фшийн ресфйн айрн йгетйн дйеъ щдоаош дочешй рлъб бсйрйъ.
https://www.abebooks.com/Chinese-Medical-Herbology-Pharmacology-John-Chen/16278843054/bd
бозчш отбгд (2008) рбзрд штймеъ фишййъ шййщй ефемйслшйгйн щоеце одфишййд бойрерйн щерйн тм щешеъ ъай зйсеп (ъайн оереречмйашйн оп дгн дфшйфшй) щм зойщд обевшйн бшйайн, зойщд ймгйн бшйайн (иеез вймайн 8-18) ещйщд ймгйн земй сшип дтебшйн ийфемйн лйоеъшфййн* (иеез вймайн 13-18). рцфъд овод отешбъ щм дщфтд тм зйеъ дъайн бойрерйн щерйн щм шййщй едрвжшъ дфемйслшйгйъ: бойрерйн роелйн (1-50 ойчшевшн моймймйиш) ма ршщод дфзъд бзйеъ дъайн ебщвщевн бчшб рбгчйн бшйайн еау ршщод тмйд бщвщев дъайн, ак вн ма ршщод тмйд бзйеъ дъайн ебщвщевн бчшб ймгйн бшйайн еймгйн земй сшип. тн дтмййд бойреп щм шййщй ещм дфемйслшйгйн (бойрерйн вбедйн о-100 ойчшевшн моймймйиш) змд дфзъд ъмеййъ ойреп бзйерйеъ дъайн щргвое олм чбецеъ дрбгчйн, омбг бчшб ймгйн земй сшип бойрерйн 50, 100 е-200 оймйвшн ммйиш ащш ацмн рцфъд тмйд оебдчъ бзйеъ дъайн ебщвщевн. осчръ дзечшйн дйъд щбойрерйн вбедйн щм шййщй едрвжшъ дфемйслшйгйъ щм дфишййд, ма рйъп мчбет зг ощотйъ лй дфишййд отеггъ щвщев щм ъайн зсерййн.
* дийфем длйоеъшфй дйд азйг млемн: mercaptopurine-6 огй йен бриймд феойъ, methotrexate огй щбет е-vincristine огй щбет бощк ашбтд щбетеъ, елп methotrexate боъп ъек ъйчй (мъек режм дщгшд) азъ м-12 щбетеъ.
https://www.ncbi.nlm.nih.gov/pubmed/18603664
*дтшъ дотшлъ мвбй Ganopoly®:
бозчшйн дщерйн ебсчйшеъ щртшле тм дцоз оцаре щрй геезйн сеъшйн мвбй дълщйш. мфй дгйеез дшащеп огебш блоесеъ щблм азъ одп ъоцйъ ъчрйъ щм шййщй оъечрръ мфй 25% фемйслшйгйн бойреп 600 о"в (щеед тшк м-30 вшн фишйд). мфй дочешеъ дмме дйеъ щдфишйд дщмод олймд 0.5% фемйслшйгйн, йзс дъоцйъ мфишййд дщмод обзйръ дълемд дфемйслшйгйъ деа 50:1, емлп ойреп щм 600 о"в деа щеед тшк м-30 вшн фишйд(48,120).
тн жаъ, бочешеъ азшйн (119,125) рлъб щогебш блоесеъ щблм азъ одп ъоцйъ ъчрйъ щм шййщй оъечрръ мфй 25% фемйслшйгйн бойреп 600 о"в (щеед тшк м- 9 вшн фишйд). мфй тоег дйцшп (Alpha Group рйе жймрг) йълп щресфе мълщйш шлйбйн ресфйн бойреп ма йгет (Cordyceps sinensis, Astragalus membranacus, Trametes versicolor, Lycium chinense, Chitosan).
рлеп мрчегъ жоп же ма дъчбмд ъвебъ дйцшп еайп бафщшеъре мййщб аъ дсъйшд.
зжшд мъзймъ дозчшйн
вД'йрсрв
вД'йрсрв лммй | в'Дйрсрв чеЙшйарй
вД'йрсрв лммй
счйшд (гцобш 2015) доцйвд аъ дщйоещ босфш шлйбйн цозййн доелшйн басйд мийфем еорйтд щм сшип ботшлъ дтйлем, лемм в'йрсрв чешйарй (Panax ginseng), лешлеойп, ъд щзеш, ъд йшеч (Camellia sinensis), в'рйсийап доцей биефе, дшлйбйн дфтймйн бщен (Allium sativum), чфсайцйп, в'йрв'шем есймйошйп.
http://www.ncbi.nlm.nih.gov/pubmed/26651248
счйшд (аечиебш 2015) ащш ретгд мбзеп дан дщйоещ бцозй ошфа бтмй фтймеъ арий-гмчъйъ тщей мдйеъ йтйм морйтд ае тйлеб дъфъзеъ щм ооайшеъ блбг (чшцйреод щм длбг - HCC).
дзечшйн осбйшйн лй йщрп тгейеъ доцбйтеъ тм лк щоцб гмчъй лшерй чщеш бдъфъзеъ щм ооайшейеъ осевйн щерйн ботшлъ дтйлем елп лй шоеъ вбедеъ щм даржйн ALT чщешеъ бсйлеп вбед йеъш м-HCC.
отбш млк, боцб щм гмчъ лшерйъ цфей лй йземе щйреййн вриййн баефп одйш йеъш еддъфъзеъ щм вйгемйн тмемд мдйеъ оеацъ лащш шоеъ ALT вбедеъ баефп лшерй.
олап, мцозй ошфа бтмй фтймеъ арий-гмчъйъ тщейд мдйеъ дщфтд ойийбд тм дъфъзеъ HCC.
бсчйшд офешиеъ дтгейеъ мвбй дщйоещ босфш фешоемеъ цозйеъ доелшеъ бйфп: Sho-saiko-to, Juzen-taiho-to, SNMC елп шлйбйн доефчйн одцоз чтшешйъ сйрйъ (Scutellaria baicalensis) ев'йрсресйгйн доефчйн оцоз дв'йрсрв.
дзечшйн ослойн лй цозй дошфа доелшйн мийфем бдфштеъ блбг дйрн бтмй дщфтд арий-гмчъйъ оелзъ аемн йщ мдощйк ембзеп аъ йтймеън морйтд ае тйлеб дъфъзеъ HCC.
http://www.ncbi.nlm.nih.gov/pubmed/26457019
озчш ощеъу мзечшйн йщшамййн емзечшйн оогйреъ дожшз дъйлеп (ребобш 2015) тесч бсйлерйн дафщшййн дчщешйн бщйоещ бшфеаъ цозйн осешъйъ босвшъ дийфем бземй сшип.
дзечшйн бгче аъ дщйоещ бцозй ошфа бдъан мгйеез доифм даерчемевй едтшйле аъ дсйлерйн лъецад ощйоещ жд. мщн лк, оифмйн аерчемевййн б-16 огйреъ божшз дъйлеп дъбчще мома щамеп бе дъбчще мдтшйк оецшйн цозййн бдн оиефмйдн тещйн щйоещ. баоцтеъ отрд щм 339 оифмйн (80.3%), жеде 44 ъесфйн цозййн е-3 шлйбйн щайрн цозййн, лащш дцозйн дщлйзйн бйеъш дйе сшфг (Urtica dioica), щен (Allium sativum), чцз (Nigella sativa) елешлен (Curcuma longa) елп шлйбйн лое змб рачеъ егбщ.
осчйшъ дсфшеъ огеезйн дзечшйн лй щйоещ б-29 одоецшйн тмем мдйеъ омеед бсйлерйн щерйн.
баефп сфцйфй, бдъййзс м-15 цозй ошфа роцае сйлерйн дчщешйн бъвебд дггйъ бйп дийфем дцозй едъшефъй, бтйчш бщм дщЃфтън тм аржйой цйиелЃшен P450. цозй ошфа аме леммйн: Allium sativum, Camellia sinensis, Curcuma longa, Foeniculum vulgare, Ginkgo biloba, Hypericum perforatum, Matricaria recutita (chamomilla), Melissa officinalis, Mentha piperita, Panax ginseng, Polygonum, Silybum marianum, Thymus vulgaris, Trifolium pratense, Vitis vinifera.
18 цозй ошфа тмемйн мвшен мштймеъ баефп йщйш, бтйчш тм йгй двбшъ дсйлеп мгйоен ефвйтд бфтймеъ дисйеъ: Allium sativum, Camellia sinensis, Cuminum cyminum, Curcuma longa, Ferula asafetida, Foeniculum vulgare, Ginkgo biloba, Hippophaerhamnoides, Linum usitatissimum, Nerium oleander, Nigella sativa, Olea europaea, Panax ginseng, Thymus vulgaris, Trifolium pratense, Trigonella foenum-graecum, Vitis vinifera, Zingiber officinale.
е-7 цозй ошфа тмемйн мдщфйт тм йтймеъ длйоеъшфйд: Curcuma longa, Ganoderma lucidum, Linum usitatissimum, Nigella sativa, Panax ginseng, Silybum marianum, Viscum album.
бщм сйлерйн ощотеъййн амд, чешайн дзечшйн моифмйн аерчемевййн мдбрд шзбд еотойчд йеъш щм дщйоещ бцозй ошфа лащш щймеб щм оифмйн айрившийбййн тн длщшд ййтегйъ тщей мъшен дп мземйн едп моифмйн даерчемевййн емсййт бчбмъ дзмиеъ оещлмъ бйзс мйтймеъ едбийзеъ щм дщйоещ бцозй ошфа.
дтшъ дотшлъ: мазш чшйад йсегйъ щм доаош, ршад лй ошбйъ ддомцеъ дребтеъ ооре обессеъ тм дрзеъ ъйаешийеъ, еайрп овебеъ бшайеъ чмйрйеъ. йзг тн жаъ, тчб зщйбеъе щм дреща, лгай бдзми мрдев ждйшеъ бочеоеъ бдн щешд ай еегаеъ.
змч вгем одръерйн еодаждшеъ догеезйн боаош лбш оцей боеревшфйн дшмеериййн байргчс дцозйн щмре. аре оощйлйн мтбг аъ дръерйн ащш фешие боаош, ебойгъ дцешк ртглп аъ доеревшфйн дшмеериййн бдъан.
http://www.ncbi.nlm.nih.gov/pubmed/26599199
бозчш отбгд (оай 2016), щбецт тм ъай сшип чемешчимй арещййн, роца лй мойцей в'йрсрв (Panax notoginseng) фтймеъ арий-сширйъ едщфтд тм дъчщешъ дъайъ дчщешд бдъфъзеъ вшешеъ.
https://www.ncbi.nlm.nih.gov/pubmed/27222068
озчш отбгд (2015) доцбйт тм дфтймеъ дарий-сширйъ щм в'йрсрв сйбйшй лрвг ъай сшип арещййн осевйн щерйн.
http://www.ncbi.nlm.nih.gov/pubmed/26107240
бсчйшд (йреаш 2017) оецвеъ дтгейеъ дтглрйеъ бдъййзс мъфчйг щм в'йрсрв чешйарй (Panax ginseng) ешлйбйе дфтймйн бтйлеб ъдмйлй арвйевржд, бгвщ тм ъдмйлйн дчщешйн мъдмйлй гмчъ, еблк мъшен мийфем бсшип.
https://www.ncbi.nlm.nih.gov/pubmed/28068835
бсчйшд (ребобш-гцобш 2016) грйн дзечшйн бфтймеъ дшфеайъ щм в'йрсрв (Panax), бгвщ тм дфтймеъ дарий-сширйъ. дзечшйн оцййрйн лй мв'йрсрв ойезсеъ дщфтеъ шбеъ, лемм дшвтд, дщшаъ щйрд, двбшъ ъщечд ойрйъ, дщфтд ревгъ гйлаеп, ощъръ еотешшъ елп феирцйам мийфем бовееп бтйеъ шфеайеъ лвеп селшъ, амцдййош, дфштеъ бжчфд ежйдеойн. бщрйн дазшереъ рйъп гвщ мдтшлъ дйтймеъ щм в'йрсрв морйтд еийфем бсшип емдфзъъ ъсойрйн дчщешйн бозмд.
бщмб жд ма роцад ъойлд озчшйъ мфтймеъ дарий-сширйъ щм в'йрсрв, аемн деа роца йтйм мдфзъъ ъзещъ земщд тм шчт озмъ дсшип едийфем дарий-сширй. бресу, йщрп тгейеъ оевбмеъ, доцбйтеъ тм дщфтд ойийбд боцбйн щм гмчъ лшерйъ щм дау едмет, селшъ, амцдййош едфштеъ бжчфд. тн жаъ, дзечшйн оцййрйн лй в'йрсрв тмем мвшен мъвебеъ дггйеъ тн ъшефеъ, мошеъ щоъеаш лбиез баефп йзсй. дзечшйн ослойн лй тм сок дтгейеъ дчййоеъ, рйъп мдщъощ бв'йрсрв мийфем бземщд бчшб земй сшип ъек отчб щм даерчемев доифм.
https://www.ncbi.nlm.nih.gov/pubmed/28039696
в'йрсрв чешйарй
бозчш отбгд (2018)дегвод дфтймеъ ревгъ дсшип щм змчйчй лсу доефчйн отмй в'йрсрв чешйарй (Panax ginseng).
https://www.ncbi.nlm.nih.gov/pubmed/27643558
вД'йрсрв аошйДчай
счйшд | орйтд | дфзъъ ъщДйщеъ | щшйгеъ еайлеъ зййн
счйшд
оаош (йемй 2013) доцйв аъ дтгейеъ дозчшйеъ дтглрйеъ бревт мфтймеъ дарий-сширйъ щм в'йрсрв аошйчай, ъек дъочгеъ бозчшйн дтесчйн бсшип дотй.
бресу, йщрн ооцайн доцбйтйн тм дъшеод щм в'йрсрв аошйчай лзмч одийфем дъеок бземй сшип, лемм дфзъъ ъефтеъ дмееай щм ийфемй длйоеъшфйд ещйфеш айлеъ зйй дземйн.
дзечшйн оцййрйн лй йщ мдощйк емждеъ аъ дшлйбйн дфтймйн еаъ ъецшй дфйшеч щмдн ембзеп аъ дщфМтън боишд мфъз ийфемйн арий-сширййн згщрййн.
http://www.ncbi.nlm.nih.gov/pubmed/24133965
орйтд
бозчш (афшйм 2017) бе дщъъфе 6 оъргбйн бшйайн, дцешлйн баефп щвшъй ъжерд отшбйъ ае асййъйъ, роца лй риймъ в'йрсрв аошйчай мощк 7 йойн дебймд мдбгмйн бшоеъ доибемйийн лъмеъ бсев дъжерд. дсйбд млк дйа щсев дъжерд дрцшлъ ощфйт тм дшлб дзййгчйн ботй емамд йщ ъфчйг ошлжй бфйшеч ебсфйвд щм в'йрсрв аошйчай. бчшб рбгчйн щцшле ъжерд дасййъйъ шоъ д-Rb1 бгн дйъд вбедд боебдч оащш бчшб рбгчйн щцшле ъжерд отшбйъ, ак шоъ д-Compound K щроца бозчшйн шбйн лшлйб арий сширй тйчшй дйъд роелд боебдч. осчръ дзечшйн дйъд щв'йрсрв аошйчай тщей мдйеъ бтм феирцйам арий-сширй вбед йеъш бчшб ощъъфйн дцешлйн гйаид отшбйъ.
https://www.ncbi.nlm.nih.gov/pubmed/27606833
бозчш фйймеи чмйрй ачшай еобечш фмсбе (2015), 14 оъргбйн бшйайн (иеез вймайн 22-52) бцен земче ачшайъ мщъййд зг фтойъ щм змйиъ в'йрсрв аошйчай (щчйч ебе 1800 о"в цоз вшес щдещшд б-200 о"м ойн шеъзйн бощк зцй щтд) ае фмсбе (200 о"м ойн шеъзйн оцеррйн). гвйоеъ гн расфе одрбгчйн мфрй дщъйд ещтъййн мазшйд ерзщфе мчшйрд аемишд свемйъ. роца лй щъййъ змйид щм в'йрсрв аошйчай дврд тм д-DNA офрй фвйтд зоцерйъ бтчбеъ дзщйфд мчшйрд. щйтеш дфвйтд б-DNA йшг б-17% (p=0.0156) щтъййн мазш дщъйд бчбецъ дв'йрсрв даошйчай, ема йшг лмм бчбецъ дбйчешъ. ддбгм бйп дчбецеъ лтбеш щтъййн дйд оебдч (p=0.0021).
https://www.ncbi.nlm.nih.gov/pubmed/26393910
дфзъъ ъщДйщеъ дчщешд бсшАип
озчш чмйрй ачшай лфем-сойеъ (аевеси 2013) бзп аъ йтймеъ ебийзеъ дщйоещ бъесфй в'йрсрв аошйчай мийфем бъсойрй ъщйщеъ одн себмйн земй сшип шбйн. дозчш лмм 364 ощъъфйн о-40 ошлжйн бшзбй ашд"б щдзмйое оозмъ дсшип еземче ачшайъ мщъй чбецеъ – чбецд азъ чйбмд ойреп йеой щм 2000 о"в в'йрсрв аошйчай едщрййд чйбмд фмсбе мощк 8 щбетеъ. бъен ддътшбеъ чбецъ дозчш дшаъд щйфеш рйлш бъщйщеъ мтеоъ чбецъ дбйчешъ (p=0.003). щйтеш дрбгчйн щгеезе тм щйфеш рйлш бтййфеъ (щйфеш щм 30% еотмд) дйд вбед бчбецъ дв'йрсрв бдщееад мфмсбе (30% мтеоъ 20%). лое лп, рбгчйн бодмк ийфемйн лйоеъшфййн геезе тм щйфеш рйлш йеъш боцб дтййфеъ бдщееад мфмсбе (p=0.01) мтеоъ оиефмйн щсййое аъ дийфемйн длйоеъшфййн (p=0.07).
https://www.ncbi.nlm.nih.gov/pubmed/23853057
озчш чмйрй лфем сойеъ обечш фмсбе (фбшеаш 2010) бзп аъ дщфМтъ в'йрсрв аошйчай бойрерйн щерйн тм ъщйщеъ дчщешд бсшип. 290 рбгчйн земй сшип щгеезе тм ъщйщеъ (4 еотмд бсемн оафс тг тщш) земче ачшайъ мчбмъ ъоцйъ ъчрйъ щм в'йрсрв аошйчай (оъечрръ мфй 5% Ginsenosides) бойреп 750, 1000 ае 2000 о"в мйен ае фмсбе бощк щоерд щбетеъ. 175 рбгчйн дщмйое аъ дозчш. рцфъд овод зйебйъ ма оебдчъ щм щйфеш бъщйщеъ (p=0.08) етмйд бзйерйеъ p=0.39)) бтчбеъ риймъ щрй дойрерйн двбедйн (1000 е- 2000 о"в) бдщееад мфмсбе емойреп дроек (750 о"в). щйтеш дрбгчйн щдбйте щбйтеъ шцеп одийфем ешае бе оетйм дйд лфем бчбецъ дв'йрсрв бдщееад мчбецъ дфмсбе (40% мтеоъ 17%).
https://www.ncbi.nlm.nih.gov/pubmed/19415341
озчш чмйрй фъез ма обечш (йреаш 2017) бзп аъ йтймеъ ебийзеъ дщйоещ бв'йрсрв аошйчай бщймеб тн дъшефд шйимйп (Methylphenidate) бийфем бъщйщеъ дчщешд бсшип (Cancer related fatigue). дозчш бгч 28 рбгчйн земй сшип щгеезе тм гйшев ъщйщеъ щм 3 еотмд (оъек 10) бсемн ддтшлд щм агоериеп (ESAS- Edmonton symptom assessment scale) бтчбеъ ийфемй шгйеъшфйд е/ае лйоеъшфйд иефме бъоцйъ в'йрсрв аошйчай бойреп 2000 о"в мйен (сев дъоцйъ ае шйлежд ма цейре боаош) бщймеб тн дъшефд шйимйп (бойреп 10-40 о"в мйен) бощк 30.5 йен бооецт. 15 рбгчйн дщмйое аъ ддътшбеъ (тщшд рбгчйн ма риме аъ дийфем дощемб лргшщ, щрй рбгчйн фйъзе ъефтеъ мееай щм зшгд ещмщем щдебйме мдфсчъ дщъъфеън, ербгч азг оъ лъецад одъчгоеъ озмъе). 60% одрбгчйн геезе тм щйфеш оебдч бшоъ дъщйщеъ, егйшев дъщйщеъ дооецт йшг ау деа боебдч бдщееад мгйшев мфрй ддътшбеъ (дфзъд щм 2.8 рчегеъ бгйшев бооецт p<0.0002).
https://www.ncbi.nlm.nih.gov/pubmed/28299946
щшйгеъ еайлеъ зййн
озчш течбд (Cohort) ъцфйъй (2006) щртшк бсйп бдщъъфеъ 1455 земеъ сшип дщг бзп аъ дчщш бйп риймъ ойрй в'йрсрв (Panax ginseng е- Panax quenqefoilum) мфрй еазшй дабзеп бсшип ебйп ръерй щшйгеъ (Survival) еайлеъ зййн (Quality of life). л-27% орбгчеъ дозчш риме в'йрсрв баефп чбет мфрй дабзеп бсшип. роца чщш бйп риймъ в'йрсрв мфрй дабзеп ебйп сйлеп оефзъ моееъ баефп лммй (0.71) есйлеп оефзъ мдйщреъ дозмд еоееъ оп дозмд (0.70) бодмк щщ щреъ дозчш. лое лп, роца чщш оебдч бйп риймъ в'йрсрв мфрй еазшй дабзеп бсшип, бтйчш бчшб дрбгчеъ щтгййп риме в'йрсрв щщ щрйн оъзймъ дозчш, ебйп щйфеш байлеъ дзййн, бтйчш бдйби дфсйлемевй едзбшъй (p<0.01-0.04). дщйфеш байлеъ дзййн дйд ъмей ойреп (p=0.01). йзг тн жаъ, зщеб мцййп щщйтеш дрщйн щиефме б-Tamoxifen (ъшефд ариверйсийъ мчемирй асишевп бшчоъ дщг) дйд вбед боебдч бчшб реимеъ дв'йрсрв бдщееад мрщйн щма риме в'йрсрв (p=0.02).
https://www.ncbi.nlm.nih.gov/pubmed/16484447
зжшд мъзймъ дозчшйн
чгг чшеоДй
ийфем бсшАип | ийфем бъефтеъ мееай щм лйоеъшфйд
ийфем бсшАип
боаош счйшд щйиъйъ (2006) рбзрд йтймеъ ълщйшй цозй ошфа сйрййн длеммйн асишвмес бдвбшъ йтймеъ ъшефеъ лйоеъшфйеъ бийфем бземй сшип шйад (NSCLC) ебдфзъъ дщфтеъйдп дщмймйеъ. 34 озчшйн ачшаййн обечшйн щртшле бчшб 2815 рбгчйн рлмме боиа армйжд. лм дозчшйн дмме тсче бдщееад бйп ийфем ощемб бълщйшй цозйн сйрййн обессй асишвмес тн ъшефеъ лйоеъшфйеъ обессеъ фмийрен ебйп ийфем бъшефеъ длйоеъшфйеъ мбгп. осчръ дзечшйн дйъд щийфем дощмб дшлбй цозйн сйрййн обессй асишвмес мцг ъшефеъ лйоеъшфйеъ обессеъ фмийрен тщей мдвбйш аъ йтймеъ дийфем (ъвебъйеъ двйгем), аъ щйтеш дщшйгеъ еаъ ъфчег дземйн, мтеоъ ийфем ъшефъй бмбг. зщеб мцййп лй ошбйъ дозчшйн сбме обтйеъ оъегемевйеъ щм дйтгш ачшайеъ есойеъ, езесш гйеез тм рщйшъ рбгчйн.
https://www.ncbi.nlm.nih.gov/pubmed/16421421
бозчш чмйрй ачшай обечш фмсбе (2003) рбзрд дщфМтъ жшйчеъ асишвмес бщймеб лйоеъшфйд тм айлеъ зйй оиефмйн дсебмйн ощмб оъчгн щм сшип шйад. 60 земй сшип шйад щм дъайн дма чирйн (NSCLC – Non Small Cell Lung Cancer) бщмб оъчгн земче ачшайъ мчбецъ дътшбеъ емчбецъ бйчешъ. щъй дчбецеъ иефме баоцтеъ лйоеъшфйд (Mitomycin C, Vinblastine, Cisplatin). чбецъ ддътшбеъ иефмд бресу бтйшей ъек ешйгй щм асишвмес бойреп 60 о"м мйен. шйлеж дъоцйъ айре йгет аемн ллм дршад дойреп щеед тшк м-120 вшн цоз йбщ. дийфем лмм 2-3 сббйн щм 21-28 йойн лм азг. дийфем дощемб роца йтйм йеъш баефп оебдч (40%) оащш дийфем длйоеъшфй мбге (36.7%) бдашлъ ощк рсйвъ дозмд, бщйфеш жоп дщшйгеъ дзцйерй ещйтеш дщшйгеъ лтбеш щрд, ебщйфеш дъецаеъ дчмйрйеъ еайлеъ дзййн щм земй сшип шйад осев NSCLC бщмб оъчгн.
https://www.ncbi.nlm.nih.gov/pubmed/14626183
бозчш чмйрй ачшай обечш фмсбе (2014) рзчшд дщфМтъ риймъ асишвмес тм йтймеъ дийфем длйоеъшфй етм ъефтеъ дмееай щм дийфем бземйн тн вйгемйн ооайшйн. 120 рбгчйн бтмй вйгемйн ооайшйн земче ачшайъ мщъй чбецеъ. щъй дчбецеъ иефме блйоеъшфйд, ак чбецъ ддътшбеъ иефмд бресу баоцтеъ тйшей 250 о"м ъойсъ омз щдлймд 20 о"м ъоцйъ асишвмес. дтйшей рйъп фтн бйен бощк ашбтд сббй ийфем брй 21 йойн лм азг. роца щдийфем дощемб тщей мтлб аъ дъфъзеъ двйгем емдфзйъ аъ ддщфтеъ дштймеъ дрмееъ мийфем (йшйгд фзеъд бсфйшъ ъай дгн дмбрйн ебсфйшъ дисйеъ), елп мзжч аъ дъфчег дзйсерй щм дрбгчйн емщфш аъ айлеъ зййдн(22).
бозчш течбд шишесфчийбй рбзрд йтймеъ тйшей асишвмес лийфем оесу млйоеъшфйд бмечойд мйофебмсийъ зшйфд (ALL – Acute Lymphoblastic Leukemia) бчшб ймгйн. рйъез шишесфчийбй бецт ъек щйоещ бръерйн чмйрййн щрасфе тм 105 ймгйн щаебзре лсебмйн о-ALL бйп йреаш 2009 ебйп гцобш 2012. дймгйн сееве мщмещ шоеъ сйлеп (сйлеп роек, сйлеп бйрерй есйлеп вбед) еземче ачшайъ мчбецъ ддътшбеъ емчбецъ дбйчешъ, лащш лм чбецд лммд ймгйн олм чбецеъ дсйлеп. щъй дчбецеъ иефме баоцтеъ лйоеъшфйд, бдъан мшоеъ дсйлеп щм дймгйн. чбецъ ддътшбеъ чйбмд бодмк дийфем вн тйшей асишвмес (бойреп 0.5-1 о"м мч"в мйен). шйлеж дъоцйъ айре йгет аемн ллм дршад дойреп щеед тшк м-1-2 вшн цоз йбщ млм чйме ощчм веу. айме чбецъ дбйчешъ чйбмд тйшей фмсбе. бйен д-19 мийфем, ртшле дщееаеъ бйп дчбецеъ. роца щдийфем басишвмес ма щйрд аъ дъфмвеъ двешойн дфшевресиййн ае аъ щйтеш дрсйвд домад (щтог тм 79% одрбгчйн мма дбгм оебдч бйп дчбецеъ), ак дфзйъ бойгд оебдчъ аъ щйтеш дозмд дщйешйъ дойрйомйъ* длммй еаъ щйтеш дозмд дщйешйъ дойрйомйъ тбеш лм азъ очбецеъ дсйлеп.
*щйтеш дозмд дщйешйъ дойрйомйъ деа аоцтй орба мзжшъ двйгем емдйщреъ дозмд.
https://www.ncbi.nlm.nih.gov/pubmed/24568906
ийфем бъефтеъ мееай щм лйоеъшфйд
боаош счйшд щйиъйъ (2005) рбзрд дщфМтъ риймъ ълщйшй цозйн сйрййн длеммйн асишвмес тм ъефтеъ мееай щм ъшефеъ лйоеъшфйеъ мийфем бсширй дотй двс едзмземъ. ъефтеъ дмееай лмме бзймеъ едчаеъ, лабйн бфд, щмщемйн, штймеъ лбгйъ, гйлей оз дтцн егйлей зйсерй. лое лп, рбзрд дщфМтъ дийфем дцозй тм айлеъ зйй доиефмйн. мцешк доиа армйжд рсчше озчшйн ачшаййн щтсче бийфем бсшип дотй двс едзмземъ, едщее бйп ийфем лйоеъшфй бмбг ае бцйшеу ъшефеъ ревгеъ дчад (Tropisetron, Sulpiride етег) ебйп ийфем лйоеъшфй бцйшеу ълщйшй цозйн сйрййн.
боиа армйжд рлмме ашбтд озчшйн щртшле бчшб 342 рбгчйн. мошеъ дайлеъ доъегемевйъ дйшегд щм дозчшйн, дсйче дзечшйн щълщйшй цозйн длеммйн асишвмес тщеййн мтешш аъ ъфчег ъай отшлъ дзйсеп емдфзйъ ъефтеъ мееай щмймйеъ (бзймеъ едчаеъ) бземйн доиефмйн баоцтеъ лйоеъшфйд. ма геез тм ъефтеъ мееай ма шцейеъ бтчбеъ дщйоещ бълщйшй дцозйн.
https://www.ncbi.nlm.nih.gov/pubmed/15674951
бозчш чмйрй ге щмбй ачшай лфем сойеъ еобечш фмсбе (2012) рбзрд йтймеъ ътшебъ фемйслшйгйн щоеце оасишвмес (PG2) лийфем ощмйн еоерт мтййфеъ дчщешд бсшип. 75 рбгчйн дземйн бсшип оъчгн щсбме отййфеъ бшод бйрерйъ тг зоешд земче мщъй чбецеъ. чбецъ ддътшбеъ чйбмд PG2 бойреп щм 500 о"в, щмещ фтойн бщбет, мощк ашбтд щбетеъ. дълщйш PG2 (дзбшд доййцшъ: PhytoHealth Corp., Taiwan) дре ътшебъ фемйслшйгйн щоеце оасишвмес лабчд едеосе бъойсъ омз. чбецъ дбйчешъ чйбмд ъойсъ омз брфз ждд. мазш олп, бщмб дфъез щм дозчш чйбме лм дрбгчйн мощк ашбтд щбетеъ ресфйн ийфем бтйшей щм PG2. оъецаеъ дозчш темд щдийфем баоцтеъ PG2 щйфш баефп оебдч аъ шоъ дтййфеъ дчщешд бсшип бчшб дрбгчйн щиефме баоцтеъ фмсбе мфрй лп. бчбецъ д-PG2 рцфд щйтеш вбед йеъш (57% мтеоъ 32% бщбет дшащеп бмбг) щм щйфеш бтййфеъ, бдщееад мчбецъ дфмсбе. лое лп, 82% одрбгчйн щгйеезе тм щйфеш бъсойрй дтййфеъ бтчбеъ дсбб дшащеп щм дийфем баоцтеъ PG2 зще щйфеш ресу бтчбеъ дсбб дщрй. л-71% одрбгчйн щиефме баоцтеъ PG2 ема гйеезе тм щйфеш бъсойрйн бсбб дшащеп, гйеезе тм щйфеш оебдч бтчбеъ дощк дийфем бсбб дщрй. дооцайн омогйн тм йъшеп афщшй мийфем ооещк (мотмд оашбтд щбетеъ) баоцтеъ PG2 етм дщфМтъе дрбрйъ маешк жоп. ма ршщое ъефтеъ мееай ощотеъйеъ ае бмъй дфйлеъ бтчбеъ дийфем (ъефтеъ дмееай догеезеъ дйе фшйзд, ачжод етчцецйн).
https://www.ncbi.nlm.nih.gov/pubmed/22309959
бозчш чмйрй ачшай обечш фмсбе (2012) рбзрд йтймеъ джшчъ фемйслшйгйн щоеце оасишвмес бийфем бсшип шйаеъ оъчгн длемм ъшефеъ лйоеъшфйеъ обессеъ фмийрен ебцоцен ъефтеъ дмееай дщмймйеъ дребтеъ оийфем жд. 136 рбгчйн щаебзре бсшип шйаеъ оъчгн осев NSCLC земче ачшайъ мщъй чбецеъ. чбецъ ддътшбеъ чйбмд ъшефеъ лйоеъшфйеъ обессеъ фмийрен (Vinorelbine е-Cisplatin) бщймеб тн жшйчъ фемйслшйгйн щоеце оасишвмес. шйлеж еойреп дъоцйъ айрн йгетйн. чбецъ дбйчешъ чйбмд аъ дийфем дъшефъй бмбг. бъен щмещд озжешй ийфем ршщое дбгмйн оебдчйн бйп дчбецеъ богг айлеъ дзййн (QOL), богг дъфчег дфйсй, бшоъ дтййфеъ, ебгйеез тм бзймеъ едчаеъ, тм лабйн етм аебгп ъйабеп. ма роцае дбгмйн оебдчйн бйп дчбецеъ бщйтеш дъвебд даебйчийбйъ мийфем, бжоп дщшйгеъ дзцйерй ебщйтеш дщшйгеъ лтбеш щрд.
https://www.ncbi.nlm.nih.gov/pubmed/21928106
бозчш ачшай обечш фмсбе (2014) рбзрд дщфМтъ жшйчъ асишвмес брчегъ дгйчеш ST36 (мцг ийфем чербрцйермй) тм ъефтеъ мееай щмймйеъ щм ийфем лйоеъшфй бсшип дчйбд. 67 рбгчйн бтмй вйгем сширй бчйбд земче мщъй чбецеъ. щъй дчбецеъ иефме баоцтеъ лйоеъшфйд еъшефеъ чербрцйермйеъ морйтъ дчаеъ, мщйфеш дъйабеп емдфзъъ мейчефрйд. чбецъ ддътшбеъ чйбмд бресу мийфемйн аме жшйчъ асишвмес брчегъ дгйчеш ST36. ръерйн ресфйн аегеъ ойреп ае аефп ойцей дцоз щрйим зсшйн. дщееад бйп дчбецеъ мазш ддътшбеъ дгвйод щйфеш оебдч боцб дмейчефрйд бчбецъ ддътшбеъ мтеоъ чбецъ дбйчешъ. бресу, мазш дийфем длйоеъшфй ршщод тмйд оебдчъ бшоеъ дзрчп аешйад бщъп (BUN) щм дрбгчйн бчбецъ дбйчешъ. мтеоъ жаъ, ма ршщн щйрей оебдч бшоеъ дзрчп аешйад бщъп щм дрбгчйн бчбецъ ддътшбеъ. ооца жд тщей мдтйг лй масишвмес фтймеъ доврд тм ъфчег длмйеъ бодмк чбмъ ийфемйн лйоеъшфййн.
http://en.cnki.com.cn/Article_en/CJFDTotal-SHZJ201402024.htm
бозчш ачшай (2005) рбзрд дщфМтъ джшчъ ъоцйъ асишвмес мрчегеъ дгйчеш ST36 мтеоъ ийфем чербрцйермй еосешъй тм ъфчег отшлъ дзйсеп бземй сшип. 78 рбгчйн земй сшип щсбме омейчефрйд земче мщъй чбецеъ. чбецъ азъ чйбмд 4 о"м ъоцйъ асишвмес режмйъ бджшчд мазъ ощъй рчегеъ дгйчеш ST36 мсйшевйп (сев дъоцйъ ешйлежд ма цейре боаош аемн ллм дршад дойреп щеед тшк м-8 вшн цоз йбщ), азъ мйен бощк щмещд щбетеъ. дчбецд дщрйд чйбмд ийфем феой ощемб щлмм ъшефеъ отшбйеъ чербрцйерамйеъ (Leucogen, Lithium carbonate) еосешъйеъ (Gan Xue Bao). бчбецъ ддътшбеъ ршщод тмйд бшоеъ дмейчецйийн дзм одйен дщмйщй мийфем ешод ъчйрд щм мейчецйийн дещвд бйен дщбйтй мийфем. бчбецъ дбйчешъ ршщод тмйд айийъ еоъерд бшоеъ дмейчецйийн ешод ъчйрд щм мейчецйийн дещвд бйен д-15 мийфем. жшйчъ ъоцйъ дасишвмес брчегъ дгйчеш ST36 детшлд лйтймд еодйшд йеъш одийфем дшфеай дощемб бдтмаъ шоеъ дмейчецйийн. лое лп, бчбецъ ддътшбеъ ршщод тмйд оебдчъ бшоъ фтймеъ ъай NK ейшйгд оебдчъ бшоеъ дчемирйн майришмейчеп 2.
https://www.ncbi.nlm.nih.gov/pubmed/15889516
бозчш ачшай лфем сойеъ обечш фмсбе (2014) рбзрд дщфМтъ тйшей асишвмес тм оггй жйден бодмк ийфемйн лйоеъшфйн бчшб ймгйн тн мечойд мйофебмсийъ зшйфд. 91 ймгйн щсбме омечойд мйофебмсийъ зшйфд земче ачшайъ мщъй чбецеъ. чбецъ ддътшбеъ чйбмд тйшей щм асишвмес (0.5 о"м мчймевшн мйен) бощк 35 йойн, ечбецъ дбйчешъ чйбмд ойреп очбйм щм ъойсъ омз. йъш дийфем дъеок дйд ждд бщъй дчбецеъ. дийфем баоцтеъ асишвмес роца йтйм йеъш офмсбе бдфзъъ гйлей оз дтцн дребт оийфемйн лйоеъшфййн ебдтмаъ шоеъ дрейишефймйн мазш дийфем. баефп жд осййт дийфем басишвмес бцоцен щйтеш ддгбчеъ бжйдеойн, ебчйцеш ощк джйдеойн.
https://www.ncbi.nlm.nih.gov/pubmed/24568907
щеМщ чйшз
озчш чмйрй ачшай лфем сойеъ еобечш фмсбе (2017) бзп аъ йтймеъ дийфем бтжшъ щещ чйшз борйтъ оечесйийс щм дфд бтчбеъ ийфемй шгйеъшфйд бземй сшип дшащ едцееаш. 37 рбгчйн дземйн бсшип дшащ едцееаш дтебшйн ийфемй шгйеъъшфйд земче ачшайъ мошйзд очеойъ щм ъоцйъ ойойъ щм щещ чйшз бшйлеж 50% ебойреп щм 20 о"м ае фмсбе фтоййн бйен бощк щбетййн оъзймъ дийфемйн. бъен ддътшбеъ рцфд дбгм оебдч бзеошъ дрвтйн (p=0.04) ебъзещъ двйшей бшйшйъ дфд мфй гйеез дрбгчйн (p=0.03) бйп чбецъ ддътшбеъ мбйп чбецъ дбйчешъ. лое лп, рцфд дбгм оебдч бщйтеш дрбгчйн щфйъзе рвтйн бгшвд 2-3 бчшб щъй дчбецеъ (p<0.001).
https://www.ncbi.nlm.nih.gov/pubmed/29296112
озчш чмйрй дщееаъй ачшай лфем сойеъ еобечш (2017) бзп аъ йтймеъ ебийзеъ дщйоещ бшцетеъ дрцогеъ мшйшйъ долймеъ дрвжшъ дфемйфремйъ щм щещ чйшз бдщееад мъшефд дсишеайгйъ triamcinolone acetonide бийфем боечежйийс щм дфд бтчбеъ ийфемй шгйеъшфйд бчшб земй сшип дшащ едцееаш. 60 рбгчйн (вйм ооецт 57.33) щтбше ийфемй дчшреъ ефйъзе бодмлн оечежйийс щм дфд бгшвъ зеошд 2-3 (бсемн щм 0-4) земче ачшайъ мдгбчъ шцетеъ долймеъ 0.5 о"в triamcinolone acetonide ае ъоцйъ фемйфреЙмйн щоецъд ощещ чйшз бойреп 0.18 о"в ашбт фтойн бйен мцг ийфем сиргший (щлмм щийфд ълефд бойн оешъзйн, цзцез щйрййн ещйоещ бзеи гримй бчбйтеъ едсшъ абп щп еабрйъ) бощк зегщ ае тг мдйтмоеъ оезмиъ щм дрвтйн. бодмк дозчш дрбгчйн ма иефме бъшефеъ лйоеъшфйеъ, ъшефеъ рсйерйеъ ае ъшефеъ мгйлей зйсерй ема дешще мйием ощллй лабйн. бъен ддътшбеъ зеошъ доечежйийс детшлд тм йгй щрй отшйлйн очцетййн бмъй ъмеййн етецоъ длаб щм дрбгчйн роггд баоцтеъ семн армевй зжеъй (VAS). бщъй дчбецеъ рцфд щйфеш оебдч боцб дрвтйн бдщееад моцб дбсйс (p<0.05) мма дбгм оебдч бйрйдп, ещрй севй дийфемйн дйе афчийбййн баеъд ойгд бщйлек длабйн мфй гйеез дрбгчйн (p<0.05 бдщееад моцб дбсйс бщрйдн, мма дбгм оебдч бйп дълщйш дцозй мълщйш дъшефъй).
https://www.ncbi.nlm.nih.gov/pubmed/25347930
озчш чмйрй (2011) бзп аъ йтймеъ длрд айешеегйъ осешъйъ щм абчъ щещ чйшз бвдй егбщ борйтъ оечежйийс щм дфд бодмк ийфемй шгйеъшфйд елйоеъшфйд мземй сшип дшащ едцееаш. бозчш дщъъфе 75 рбгчйн (85.3% оъелн вбшйн, иеез вймайн 30-60) ащш земче ачшайъ машбт чбецеъ: чбецд 1: ошйзд очеойъ щм абчъ щещ чйшз бвдй егбщ бзмм дфд мфрй ддчшреъ ебресу риймд феойъ щм абчъ щещ чйшз бгбщ ебвдй бойреп 20 о"м мйен. чбецд 2: ошйзд очеойъ щм абчъ щещ чйшз бвдй егбщ бзмм дфд бмбг. чбецд 3: ошйзд очеойъ щм гбщ бзмм дфд бмбг, ечбецд 4: чбецъ бйчешъ щчйбмд ийфем ъшефъй. лм дрбгчйн иефме бийфемй шгйеъшфйд елйоеъшфйд бощк ъчефд очсйомйъ щм щбтд щбетеъ ериме ийфем ъшефъй мфй дцешк. лм дрбгчйн фйъзе оечежйийс евйшей щм дтеш бгшвеъ ощъреъ. зеошъ дрвтйн фзъд ощотеъйъ бчбецеъ щиефме баоцтеъ щещ чйшз бдщееад мийфем дъшефъй (p<0.001 чбецд 1 лбш бщбет дщрй, чбецд 2 дзм одщбет дщбйтй), ак ма фзъд бчбецд щиефмд бгбщ бмбг бдщееад мийфем дъшефъй.
https://www.ncbi.nlm.nih.gov/pubmed/22408302
зжшд мъзймъ дозчшйн
сеЙйд
бозчш течбд (ошх 2017) рбгч дчщш бйп цшйлъ айжефмберйн бъжерд (фйиеасишевп доцей бсейд) мбйп дсйлеп мъоеъд бчшб рщйн тн дйсиешйд щм сшип дщг. дзечшйн осбйшйн лй моецшй сейд вн дщфтд асишеврйъ евн арий-асишеврйъ, ечййоъ озмечъ мвбй цшйлъ оецшй сейд бчшб рщйн тн сшип дщг, бойезг аме дочбмеъ ийфем дешоермй.
бозчш рлмме дръерйн щм 6,235 рщйн тн сшип дщг, ошбйъп оймае щамерй ъжерд мфрй абзеп дсшип. бъчефъ отчб щм л-9.4 щрйн 1,224 одрщйн рфише. роца лй рщйн тн шоъ цшйлъ айжефмберйн двбедд бйеъш (отм 1.5 о"в мйен) дйе бтмеъ сйлеп роек бл-21% мъоеъд бдщееад мрщйн тн дцшйлд дроелд бйеъш (тг 0.3 о"в мйен). чщш жд ощотеъй йеъш тбеш рщйн тн вйгемйн щмймййн мчемирйн мдешоерйн емрщйн щма чйбме ийфем дешоермй (лое иоечсйфп). дзечшйн ослойн лй цшйлъ оецшй сейд долймйн айжефмберйн дййъд чщешд бсйлеп роек йеъш мъоеъд бчшб рщйн тн дйсиешйд щм сшип дщг.
дтшъ дотшлъ: озчш жд оцишу мщешд щм озчшйн, щдвйте маеъд досчрд.
https://www.ncbi.nlm.nih.gov/pubmed/28263368
счйшд (гцобш 2015) доцйвд аъ дщйоещ босфш шлйбйн цозййн доелшйн басйд мийфем еорйтд щм сшип ботшлъ дтйлем, лемм в'йрсрв чешйарй (Panax ginseng), лешлеойп, ъд щзеш, ъд йшеч (Camellia sinensis), в'рйсийап доцей биефе, дшлйбйн дфтймйн бщен (Allium sativum), чфсайцйп, в'йрв'шем есймйошйп.
http://www.ncbi.nlm.nih.gov/pubmed/26651248
счйшд (ребобш 2015) доцйвд аъ дтгейеъ дозчшйеъ бревт мдщфтд щм овееп вгем щм шлйбйн ибтййн ецозййн лрвг ъай вжт сширййн. чййоъ вйщд мфйд дочеш мвйгем сширй деа бчбецд чирд щм ъайн тн оафййрйн щм ъай вжт еорврерйн щм дйщшгеъ едъзгщеъ елъецад олк ъайн амд тойгйн бфрй ошбйъ дъшефеъ длйоеъшфйеъ.
озчшйн щерйн оцбйтйн тм лк щшлйбйн ибтййн щерйн тщеййн мдщфйт тм осмемйн дотешбйн ббйией дврий щм ъайн амд еблк осфчйн ъойлд мчщш бйп ъжерд одцеоз мбйп дфзъъ щйтеш дооайшейеъ.
бсчйшд офешийн дооцайн мвбй шлйбйн шбйн, бйрйдн смйреойцйп, семфешафп, айжефмберйн осейд, EGCG (ъд йшеч), шлйбйн саферйрйн, чеешцийп, лешлеойп, фемйфреЙмйн лое в'йрв'шем етег.
http://www.ncbi.nlm.nih.gov/pubmed/26503998
счйшд (сфиобш 2015) доцййръ лй йщ щфт щм тгейеъ оозчшйн отбгъййн (in vitro) ебвеу дзй (in vivo) дъеолеъ бдщфтеъ ревгеъ дсшип щм в'рйсиайп (айжефмбеп сейд).
двйгемйн дощотеъййн боещфтйн ов'рйсиайп ерсчшйн бсчйшд дн: щг, фшесиид, отй вс, лбг, щзмеъ, щмфезйъ дщъп, чйбд, оез, рейшебмсиеод емейчойд мйофецйийъ лшерйъ. аемн, ма ъойг бшеш ан еоъй в'рйсиайп йтйм лрвг вйгемйн ае мдйфк, оъй аеъд оемчемд вешоъ мдщфтеъ щмймйеъ еотеггъ щвщев ъай.
счйшд же отшйлд баефп бйчешъй аъ дреща мрелз дорврерйн доемчемшйн дщерйн щм в'рйсиайп, ащш оъшзщйн лщдоемчемд рйъръ бойрерйн роелйн (дщфтеъ ревгеъ сшип) ае бойрерйн вбедйн (дщфтеъ фшочемевйеъ).
мчшйад ршзбъ бреща сейд есшип мзце лап - http://www.naturopedia.com/article.asp?rId=880
http://www.ncbi.nlm.nih.gov/pubmed/26593532
счйшд дойетгъ мбзеп одй ддщфтд дбшйаеъйъ щм фйиеасишеврйн, дрчщшйн мчемирй дасишевп евешойн мдщфтд арий-асишеврйъ.
одсчйшд темд лй мфйиеасишеврйн овееп дщфтеъ ойийбеъ, лемм дфзъъ ъсойрй вйм дотбш (лвеп вмй зен), дфзъъ дсйлеп маесиаефешежйс, дфзъъ дсйлеп мъзмеад чшгйеесчемшйъ, мщореъ, мъсоеръ доибемйъ, мселшъ сев 2 емдфштеъ бъфчег доез елп дфзъъ дсйлеп мсевй сшип щерйн, лемм сшип дщг, сшип дтшоерйъ есшип дотй. тн жаъ, бозчшйн ббтмй зййн, роца чщш мбтйеъ фешйеъ (айп ажлеш бсчйшд аегеъ дщфтд щмймйъ же бозчшйн тм брй агн).
тег оцййрйн дзечшйн лй зщйфд масишевп баефп лммй чщешд бсйлеп вбед мфъз сшип щзмеъ брщйн есшип тшоерйъ еащлйн бвбшйн етм бсйс ооцайн амд дн ослойн лй ддщфтеъ дойийбеъ щм фйиеасишеврйн ма бдлшз темеъ щм ддщфтеъ дщмймйеъ едръерйн дчййойн айрн осфйчйн тм оръ мбцт рйъез тмеъ оем ъетмъ, емлп ма рйъп мчбет осчрд зг-ощотйъ мвбй ддщфтд дойийбд щм фйиеасишеврйн.
дтшъ дотшлъ: зщеб мдбгйм бйп зщйфд масишевп баефп лммй мбйп зщйфд мфйиеасишеврйн елп бйп зщйфд мфйиеасишеврйн божеп лгевоъ сейд ае фщъп мбйп фйиеасишеврйн обеггйн бъесфй ъжерд. мдшзбъ дчшйад бреща фйиеасишеврйн есшип мзце лап: http://www.naturopedia.com/article.asp?rId=880
https://www.ncbi.nlm.nih.gov/pubmed/27723080
бозчш, щртшк бчшб земгеъ (фбшеаш 2017), роца лй цшйлъ в'рйсиайп, шлйб тйчшй бсейд, бодмк лм дзййн (бгеод мъжерд дасййъйъ) овбйшд аъ йтймеъ дийфем дарий-сширй биоечсйфп, бдщееад мцшйлъ в'рйсиайп шч мазш дъфъзеъ двйгем.
https://www.ncbi.nlm.nih.gov/pubmed/28148690
бозчш зък (гцобш 2017) рбгчд дъшеод щм цшйлъ сейд ейшчеъ оцмйбйн бъжерд мдчмд тм дъсойрйн дчщешйн бийфем дарий-сширй бчшб рщйн дозмйоеъ осшип дщг. бозчш рлмме 365 рщйн, щаебзре тн сшип дщг бйп дщрйн 2006-2012 едщмйое аъ дийфем дшащерй бозмд (рйъез, дчшреъ, лоеъшфйд) 1-5 щрйн чегн мвйесп мозчш.
тм сок щамерй ъжерд щоймае дощъъфеъ егйеез аегеъ шоъ дъсойрйн, дзечшйн бгче аъ дчщш бйп цшйлъ сейд ейшчеъ оцмйбйн мбйп шоъ ъсойрй вйм дотбш, бтйеъ фшчйн, тййфеъ, щйтш гмйм ае рщйшъ щйтш ебтйеъ жйлшеп. роца лй дцшйлд щм сейд ещм йшчеъ оцмйбйн ртд бйп лмм ма мбйп 431 вшн/йен е-865 вшн/йен, бдъаод. тег роца лй цшйлд вбедд йеъш щм сейд (отм 24 вшн/йен) дййъд чщешд бшод роелд йеъш щм ъсойрй вйм дотбш ещм тййфеъ. тн жаъ, брйъез мфй щййлеъ аърйъ чщш жд дйд оебдч шч бчшб рщйн мбреъ ема бчшб рщйн ооеца сйрй. бресу, цшйлд вбедд йеъш щм йшчеъ оцмйбйн (отм 70 вшн/йен) дййъд чщешд бсйлеп роек йеъш мсбем оъсойрй вйм дотбш бчшб лмм дрщйн.
https://www.ncbi.nlm.nih.gov/pubmed/29230660
зжшд мъзймъ дозчшйн
чтшешДйъ сДйрйъ
счйшд (аечиебш 2015) ащш ретгд мбзеп дан дщйоещ бцозй ошфа бтмй фтймеъ арий-гмчъйъ тщей мдйеъ йтйм морйтд ае тйлеб дъфъзеъ щм ооайшеъ блбг (чшцйреод щм длбг - HCC).
дзечшйн осбйшйн лй йщрп тгейеъ доцбйтеъ тм лк щоцб гмчъй лшерй чщеш бдъфъзеъ щм ооайшейеъ осевйн щерйн ботшлъ дтйлем елп лй шоеъ вбедеъ щм даржйн ALT чщешеъ бсйлеп вбед йеъш м-HCC.
отбш млк, боцб щм гмчъ лшерйъ цфей лй йземе щйреййн вриййн баефп одйш йеъш еддъфъзеъ щм вйгемйн тмемд мдйеъ оеацъ лащш шоеъ ALT вбедеъ баефп лшерй.
олап, мцозй ошфа бтмй фтймеъ арий-гмчъйъ тщейд мдйеъ дщфтд ойийбд тм дъфъзеъ HCC.
бсчйшд офешиеъ дтгейеъ мвбй дщйоещ босфш фешоемеъ цозйеъ доелшеъ бйфп: Sho-saiko-to, Juzen-taiho-to, SNMC елп шлйбйн доефчйн одцоз чтшешйъ сйрйъ (Scutellaria baicalensis) ев'йрсресйгйн доефчйн оцоз дв'йрсрв.
дзечшйн ослойн лй цозй дошфа доелшйн мийфем бдфштеъ блбг дйрн бтмй дщфтд арий-гмчъйъ оелзъ аемн йщ мдощйк ембзеп аъ йтймеън морйтд ае тйлеб дъфъзеъ HCC.
http://www.ncbi.nlm.nih.gov/pubmed/26457019
бозчш, (2019) щртшк бчшб тлбшйн, огвйойн дзечшйн лй чтшешйъ сйрйъ (Scutellaria baicalensis) ъешоъ мщйфеш ддщфтд ревгъ дсшип щм лйоеъшфйд осев цйсфмийп, елп мдфзъъ аебгп ощчм еосъ щшйш (члчсйд) ефвйтд лмййъйъ лъецад одийфем.
https://www.ncbi.nlm.nih.gov/pubmed/31291609
озчш отбгд (2016) бе роца осмем оемчемшй згщ гшле дцоз чтшешйъ сйрйъ оййцш шлйбйн фтймйн бтмй дщфтд арий-сширйъ.
http://advances.sciencemag.org/content/2/4/e1501780
зжшд мъзймъ дозчшйн
еДйърйд
бсчйшд (2021) грйн дзечшйн борврерй дфтемд ревгй дсшип щм ейърйд ощлшъ (Withania somnifera) ешлйбйд дфтймйн.
https://pubmed.ncbi.nlm.nih.gov/33949906/
бсчйшд (аечиебш 2016) оецвйн цозй дошфа дощощйн бшфеад ддегйъ досешъйъ мщойшд тм фешйеъ двбш едгзу дойрй, мийфем бозмеъ лшерйеъ еморйтд щм озмеъ ойп есшип ботшлъ дшбййд. дцозйн доежлшйн бсчйшд леммйн: ейърйд ощлшъ (Withania somnifera), чиб оцей (Tribulus terrestris), асфшвес дегй (Asparagus racemosus), рйн (Azadirachta indica), шйзп чгещ (Ocimum sanctum) ев'йрв'ш (Zingiber officinale).
https://www.ncbi.nlm.nih.gov/pubmed/27681646
счйшд (гцобш 2015) доцйвд аъ дщйоещ досешъй бейърйд, аъ дтгейеъ оозчшй отбгд дъеолеъ бдщфтд дарий-сширйъ елп гйеп болщемйн дтеогйн бфрй дщйоещ бейърйд лвешн арий-сширй бийфем дчмйрй ббрй агн.
http://www.ncbi.nlm.nih.gov/pubmed/26718910
озчш чмйрй дщееаъй фъез ма ачшай (йемй 2013) бзп аъ дъшеод щм ойцей ейърйд ощлшъ мдчмд тм ъщйщеъ емщйфеш айлеъ дзййн бземеъ сшип щг дтебшеъ ийфемй лйоеъшфйд. бозчш рлмме 100 земеъ сшип щг бщмбйн щерйн щм дозмд ащш иефме блйоеъшфйд бмбг ае блйоеъшфйд бщймеб ойцей ейърйд бойреп 2 вшн лм 8 щтеъ мощк лм ъчефъ длйоеъшфйд. двйм дзцйерй щм дрбгчеъ дйд 51 бчбецъ дозчш (иеез вймайн 36-70) е-50.5 бчбецъ дбйчешъ (иеез вймайн 32-71). 77% одземеъ сбме осшип щг бгшвд 2 е-3. дъшефеъ длйоеъшфйеъ щщйоще бозчш дйе: Taxotere, Adriamycin е-Cyclophosphamide ае 5-Fluorouracil, Epirubicin е-Cyclophosphamide. одщееад бйп щъй дчбецеъ темд лй бчбецд щчйбмд ейърйд оггй дъщйщеъ дйе роелйн йеъш боебдч (p<0.001 богг д-Piper Fatigue Scale , е-p<0.003 богг Schwartz Cancer Fatigue Scale) езм щйфеш оебдч б-7 оъек 18 стйфйн богг айлеъ дзййн EORTC QLQ-C30 (бшоъ оебдчеъ щм p<0.001). дзечшйн ослойн лй ейърйд тщейд мъшен мдчмд тм ъефтеъ дмееай щм лйоеъшфйд бземеъ сшип щг аемн ргшщйн озчшйн обечшйн еачшаййн бдйчу вгем йеъш тм оръ мащщ аъ осчреъ дозчш.
https://www.ncbi.nlm.nih.gov/pubmed/23142798
озчш отбгд (сфиобш 2015) доцйв аъ орврерй дфтймеъ дарий-сширйъ щм ейърйд ощлшъ (Withania somnifera) лрвг ъай сшип дтеш осев омреод.
http://www.ncbi.nlm.nih.gov/pubmed/26334881
зжшд мъзймъ дозчшйн
вгДймп оцей
ийфем | орйтъ ъефтеъ мееай
вгДймп оцей - ийфем
щрй ъйаешй очшд (оай 2016) бзре аъ дщфМтъ ълщйш цозй (®Legasil) долйм сймйбйп (Silybin) тм дъфъзеъ вшешеъ оезйеъ бземй сшип шйаеъ щм дъайн дма чирйн (NSCLC-Non Small Cell Lung Cancer). лм лоесд щм Legasil® олймд 210 о"в щм Eurosil 85е(60% айжеош щм сймйбйп*) доефч овгймп оцей (Silybum marianum).
дземд дшащерд бъ 62 аебзрд бсшип ерцфе боезд зощ вшешеъ. мазш ийфем шащерй б- dexamethasone (ъшефд сишеайгйъ), тбшд дайщд дчшреъ бщймеб ийфем лйоеъшфй обесс фмийрен (Carboplatin) едъшефд Pemetrexed. мазш 16 йен ебтчбеъ ъмереъ щм дайщд тм дзошд бъсойрйн дрейшемевййн, тбшд дащд бгйчъ MRI щвймъд йшйгд щм 20% брфз двшешеъ доезйеъ етмйд ббцчъйеъ дочйфд аеъп. дийфем длйоеъшфй дефсч едайщд дефръд мийфем рйсйерй бълщйш дцозй ®Legasil. мазш щбет щм дъаоеъ ойреп мма геез тм ъефтеъ мееай ма шцейеъ етег щбетййн щм ийфем щезшшд дайщд обйъ дземйн тн щйфеш бъсойрйд. лтбеш зегщ оъзймъ дийфем дезми бдъййтцеъ тн шефад щм дайщд мщмб бйп дъшефд Pemetrexed ебйп дийфем бълщйш дцозй (5 лоесеъ бйен). лтбеш 4 зегщй ийфем рцфъд дфзъд щм 79% брфз двшешеъ доезйеъ. дийфем б-®Legasil мбге рощк 6 зегщйн ресфйн едебйм мдфзъд щм 84% брфз двшешеъ.
дземд дщрй бп 67 аебзп бсшип шйаеъ ерцфъд боезе вшешд азъ. деа иефм бдчшреъ бщймеб дъшефд Pemetrexed. лтбеш 4 зегщй ийфем тбш дайщ бгйчъ MRI щвймъд йшйгд брфз двшешд ак тмйд ббцчъйеъ дочйфд аеъд (сд"л 15% йшйгд). доиефм тбш мийфем баоцтеъ ®Legasil емазш дъаоъ ойреп рчбт ойреп риймд ошбй щм 3 лоесеъ бйен (бщм щмщемйн бойрерйн вбедйн йеъш). лтбеш зегщ гйеез доиефм тм щйфеш бъсойрйн дрейшемевййн. лтбеш зегщййн рцфъд йшйгд рйлшъ брфз двшешд едбцчъ (69% йшйгд).
йщ мцййп щтм ау ддщфтд дрйлшъ щм дълщйш тм двйгемйн доезййн щм щрй доиефмйн, ма рцфъд дщфтд ощотеъйъ щм дълщйш тм дозмд дшащерйъ бшйаеъ.
*мфй фший шйщен дфири Eurosil 85 овбйш аъ щзшеш дзеош дфтйм еаъ жойреъе дбйемевйъ б- 80%.
https://www.ncbi.nlm.nih.gov/pubmed/26959886
бсчйшд (2019) грйн дзечшйн борврерйн доемчемшййн дотешбйн бдщфтд ревгъ дсшип щм сймйошйп, бгвщ тм дщфтд ревгъ щвщев еотеггъ ъоеъъ ъайн сширййн, ъек дъййзсеъ мщйоещ дчмйрй бсймйошйп мийфем бсевй сшип щерйн еморйтън.
https://www.ncbi.nlm.nih.gov/pubmed/31407422
вгДймп оцей - орйтъ ъефтеъ мееай
озчш чмйрй (ребобш 2016) ачшай лфем сойеъ обечш фмсбе бзп аъ дйтймеъ щм сймйошйп (Livergol®), дшлйб дфтйм бвгймп оцей (Silybum marianum), борйтъ оечежйийс* бфд дребт оийфемй чшйрд бземй сшип шащ ецееаш. 27 рбгчйн земй сшип бодмк ийфемй чшйрд земче мчбецъ дътшбеъ ечбецъ бйчешъ. чбецъ ддътшбеъ иефмд бсймйошйп бойреп 420 о"в мйен бриймд феойъ мощк щйщд щбетеъ. бъен ддътшбеъ, роца щбдщееад мфмсбе сймйошйп дфзйъ боебдч аъ дгйшев дооецт щм доечежйийс бсемн дгйшев щм ашвеп дбшйаеъ дтемой едолеп дмаеой мсшип (World Health Organization and National Cancer Institute-Common Terminology-Criteria oral mucositis grading scale) (бшоъ оебдчеъ щм: p<0.05). гйшев жд тмд аорн бойгд оебдчъ бщъй дчбецеъ бодмк ийфемй дчшйрд, ак бчбецъ дсймйошйп дйд тйлеб бдъфъзеъ доечежйс ебдъчгоеъе.
https://www.ncbi.nlm.nih.gov/pubmed/27555604
озчш чмйрй (йреаш 2010) ачшай лфем сойеъ еобечш фмсбе бзп аъ дщфМтъ ълщйш цозй (.Siliphos® Thorne Research, Inc) долйм сймйбйрйп (Silibinin) тм ъфчегй длбг щм ймгйн еоъбвшйн тг вйм 21 дсебмйн омечойд мйофебмсийъ зшйфд (ALL-Acute Limphoblastic Leukemia) еоиефмйн блйоеъшфйд. 50 ймгйн еоъбвшйн дсебмйн о- ALL тн штймеъ лбгйъ лъецад одийфем длйоеъшфй земче ачшайъ мчбецъ дътшбеъ ечбецъ бйчешъ. чбецъ ддътшбеъ иефмд б- Siliphos®, бойреп 80-320 о"в (5.1 о"в сймйбйрйп млм ч"в ощчм двеу мйен бриймд феойъ) ечбецъ дбйчешъ иефмд бфмсбе бощк 28 йойн. дълщйш дцозй Siliphos® олйм ъоцйъ ъчрйъ щм вгймп оцей (Silybum marianum) оъечрръ мфй 33% сймйбйрйп ефесфийгймлемйп доефч осейд бйзс щм 1:2 мщйфеш джойреъ дбйемевйъ щм двгймп доцей. бъен ддътшбеъ роца лй дийфем дцозй ма дйд йтйм йеъш офмсбе бщйфеш ъфчегй длбг (йшйгд бшоеъ аржйой длбг ALT, AST, ебшоеъ дбймйшебйп длммй). тн жаъ, 28 йойн мазш ъен ддътшбеъ (56 йойн оъзймъд), рцфд йъшеп оебдч мчбецъ дълщйш дцозй бйшйгд бшоеъ д- AST (бшоъ оебдчеъ щм: p=0.05) еовод ма оебдчъ щм йшйгд бшоеъ д- ALT (бшоъ оебдчеъ щм: p=0.07). тм ау щддбгм бйп дчбецеъ ма дйд оебдч, ойрерй дъшефеъ длйоеъшфйеъ дефзъе (бвмм штймеъ лбгйъ) бчшб 61% одймгйн бчбецъ дълщйш дцозй мтеоъ 72% одймгйн бчбецъ дфмсбе.
https://www.ncbi.nlm.nih.gov/pubmed/20014183
озчш чмйрй (аевеси 2011) дщееаъй ма ачшай бзп аъ йтймеъ дийфем баоцтеъ чшн цозй Leviaderm(®) долйм сймйошйп (Silymarin) бошйзд зйцерйъ морйтъ гшоийийс ервтйн тешййн лъецад оийфемй дчшреъ бчшб земеъ сшип дщг. 101 рбгчеъ земеъ сшип щг мазш рйъез доиефмеъ бдчшреъ земче мчбецъ ийфем баоцтеъ чшн сймйошйп (0.25% сймйошйп) ечбецъ ийфем баоцтеъ чшн шфеай обесс Panthenol (щдерзъд мошез аъ дчшн бтъ дцешк). сев дойцей щм дчшн дцозй едрзйеъ дошйзд щме айрн йгетйн лйееп щдоаош дома айре рвйщ мчшйад. бтчбеъ дийфем баоцтеъ дчшн дцозй, ощк джоп тг мдефтъ дрвтйн дтешййн деашк бойгд оебдчъ (45 йойн бчбецъ дсймйошйп мтеоъ 29 йойн бчбецъ дчшн дшфеай, p<0.0001). бъен ийфемй ддчшреъ 23.5% одземеъ бчбецъ дсймйошйп ма фйъзе ъвебд тешйъ лмм мтеоъ 2% бчбецъ дчшн дшфеай. рвтйн тешййн бгшвд 3 дефйте бчшб 2% одземеъ бчбецъ дсймйошйп мтеоъ 28% бчбецъ дчшн дшфеай.
https://www.ncbi.nlm.nih.gov/pubmed/21786113
зжшд мъзймъ дозчшйн
щшбДйип оцеМй
озчш шб-ъзеой ешб ошлжй ащш ртшк тм йгй зечшйн йщшамййн, йдегйн етшбйн (оай 2016), дбезп аъ дщйоещ бцоз щшбйип оцей мийфем бсшип.
очеш дщйоещ бцоз бземй сшип дйре баелмесййд дфмсийрйъ, лащш бщрйн дазшереъ дщйоещ демк еоъфщи бчшб чбецеъ щереъ бйщшам еблм ажеш дожшз дъйлеп лийфем тоой осешъй щайре бфйчез шфеай.
босвшъ дозчш рсчшд дсфшеъ дшфеайъ, досешъйъ едоегшрйъ, мжйдей очшйн бдн ртщд щйоещ чмйрй бщшбйип оцей мийфем бсшип.
бдощк бецте бгйчеъ отбгд мъшефд мцешк жйдей шлйбйн штймйн ембгйчъ дфтймеъ дарий-сширйъ, лемм ддщфтд тм ийфем лйоеъшфй (цйсфмийп ечшбефмийп) бгвйоеъ ъай сшип дщг. дзечшйн огеезйн лй ма роцае лмм ажлешйн бсфшеъ дшфеайъ бйзс мщйоещ бщшбйип оцей мийфем бземй сшип. ббгйчеъ дотбгд ма жеде шлйбйн штймйн бъшефд (лвеп амчмеайгйн доцеййн бщшбйип дсйрй).
тн жаъ, роца лй зщйфд мъшефд дебймд мйшйгд бдщфМтъ дийфем длйоеъшфй тм гвйоеъ щм ъай сшип дщг.
дзечшйн ослойн лй вйщд озчшйъ айрившийбйъ осййтъ боъп дгшлд обессъ шайеъ мземй сшип, еблк оафщшъ щйоещ йтйм ебиез бцозй ошфа, бойезг лзмч айрившмй одийфем дшфеай дчербрцйермй.
дтшъ отшлъ: зесш ойгт айре щеед мойгт щмймй. дтебгд лй цоз дщшбйип ишн рзчш бйсегйеъ мвбй дщфтеъйе ревгеъ дсшип айрд аеошъ лмен отбш мжд щдеа ишн рзчш. чййоеъ ма оти тгейеъ мвбй йтймеъе езесш штймеъе щм дцоз лфй щофеши боаош оешзб лап.
http://www.ncbi.nlm.nih.gov/pubmed/27155666
зжшд мъзймъ дозчшйн
фешоемеъ цозйн сйрйеъ
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2018) детшлд дъшеод щм фешоемъ цозйн мдвбшъ йтймеъ дийфем ревг дсшип. фешоемъ дцозйн дсйрйъ Xi huang олймд абрй ошд щм бчш ойебщеъ (Calculus Bovis), оещч/оасч аййм (She Xiang - дфшщд щм зеошйн ашеоиййн дощощъ мбйщен), мберд (Boswellia) еоеш (Commiphora molmol). бсчйшд рлмме 15 озчшйн бдн рбгчд ддщфтд щм дфешоемд бщймеб лйоеъшфйд бдщееад млйоеъшфйд бмбг бчшб 815 обевшйн тн вйгем ооайш (ещи, чйбд, чемешчимй, щзмеъ, щг, шйад етег).
брйъез лемм щм дръерйн роца лй дийфем дощемб дйд йтйм йеъш одлйоеъшфйд бмбг едйд омеед бсйлей вбед б-35% мдвбшъ дъвебд мийфем еб-13% мщйфеш дщмйид бозмд, елп бсйлей вбед б-20% мдашлъ ощк ддйщшгеъ. бресу, дийфем дощемб роца йтйм йеъш олйоеъшфйд бмбг мщйфеш айлеъ дзййн щм доиефм емщйфеш сфйшъ ъай дгн дмбрйн едисйеъ бтчбеъ длйоеъшфйд. дзечшйн ослойн лй щйоещ бфешоемд лийфем ъеок млйоеъшфйд тщей мъшен мдвбшъ йтймеъ дийфем елп мдашлъ ощк ддйщшгеъ емдфзъъ ддщфтеъ дщмймйеъ щм дийфем, аемн ргшщйн озчшйн ресфйн байлеъ вбедд тм оръ мбсс аъ дооцайн.
https://www.ncbi.nlm.nih.gov/pubmed/30539838
озчш чмйрй ачшай (оай 2014) щретг мбзеп аъ ддщфтд щм шфеад сйрйъ лийфем ощош тм ощк ддйщшгеъ длммй еощк ддйщшгеъ мма дзошд бземйн тн сшип шйаеъ оъчгн осев NSCLC мазш ийфемй че шащеп лйоеъшфййн.
бозчш дщъъфе 69 земйн, озцйън иефме бъшефеъ лйоеъшфйеъ (Gemcitabine, Alimta ае docetaxel) еозцйън чйбме ийфем ощемб бшфеад сйрйъ длемм фешоемд ббмйтд (ошъз), фешоемд бджрд ъек-ешйгйъ еийфем овт брчегеъ мзйцд.
дийфем дъчййн бозжешйн щм 21 йен тг мдзошд бозмд, мдефтъ ъефтеъ мееай ае штймеъ, ае бдъан мшцеп дземд. роца лй бщъй дчбецеъ дийфем рощк лщрй озжешйн лащш ощк ддйщшгеъ мма дзошд дйд 12.43 щбетеъ бчбецд щиефмд бшфеад сйрйъ мтеоъ 10 щбетеъ бчбецд щиефмд блйоеъшфйд. ма роца дбгм оебдч бйп дчбецеъ бйзс мощк ддйщшгеъ длммй.
дозчш оцбйт тм лк щшфеад сйрйъ дйрд геод бйтймеъд млйоеъшфйд лийфем ощош бземй сшип шйаеъ боцб оъчгн, еау тщейд мщфш аъ оощк ддйщшгеъ мма дзошд.
http://www.ncbi.nlm.nih.gov/pubmed/24941837
озчш чмйрй (афшйм 2015) щретг мбзеп аъ дйтймеъ едбийзеъ щм фешоемъ цозй ошфа сйрйъ мийфем бъщйщеъ (щайрд лъецад оаройд) бчшб земй сшип.
бозчш дщъъфе 33 земйн ащш гйеезе тм шод бйрерйъ-вбедд щм ъщйщеъ бсйен дийфем дарий-сширй.
лм дощъъфйн риме ошъз долйм 12 цозй ошфа фтоййн бйен бощк 6 щбетеъ. бодмк дозчш ма геез тм штймеъ етм ъефтеъ мееай ощотеъйеъ.
роца лй риймъ дъесу дййъд омеед бйшйгд оебдчъ бшоъ дъщйщеъ (ошод ооецтъ щм 7.06 мшод щм 3.30). дзечшйн оцййрйн лй ргшще 2-3 щбетеъ мдщфтд ойийбд щм дийфем.
зщеб мцййп лй дозчш ма лмм чбецъ бйчешъ ейщ мбзеп аъ дйтймеъ вн оем ийфем фмсбе тм оръ маещщ аъ дооцайн.
http://www.ncbi.nlm.nih.gov/pubmed/25918996
бозчш чмйрй обечш, щайре ачшай (гцобш 2016), рбгчд ддщфтд щм фешоемъ дцозйн дсйрйъ Kuan-Sin-Yin тм шоъ даршвйд бчшб земй сшип дотй доиефмйн блйоеъшфйд.
дфешоемд Kuan-Sin-Yin дйрд ошъз, долйм щбтд цозй ошфа: чегерефсйс (Codonopsis pilosula), аишчиймегс (Atractylodes macrocephala), щещ сйрй (Glycyrrhiza uralensis), фишййъ фешйд (Poria cocos), асишвмес (Astragalus membranaceus), мйвесишен (Ligustrum lucidum) е-Agastache rugose.
бозчш рлмме 52 оиефмйн обйъ земйн биайееап, ащш земче баефп щайре ачшай мриймъ дфешоемд - фтн бйен мазш ашезъ дбечш бощк щбетййн, бйп ийфемй длйоеъшфйд - ае мчбецъ дбйчешъ, щиефмд шч блйоеъшфйд. дзечшйн осбйшйн лй дбзйшд бзмечд ма ачшайъ мчбецеъ обессъ тм лк щдийфем дрбгч айре ийфем сиргший бсшип дотй двс, емлп дн афщше мземйн мбзеш дан мчбм ийфем жд лийфем ощмйн ае мае.
йтймеъ дийфем рбгчд бдъан мщйфеш бшоъ даршвйд бошйгйарйн (баоцтеъ огйгъ ддемлд дзщомйъ) ебдщъреъ чцб дмб (heart-rate variability) логг мфтймеъ даеиереойъ, елп баоцтеъ дтшлъ шоъ дъсойрйн еайлеъ дзййн.
оъецаеъ дозчш темд лй риймъ дфешоемд ъшод мщйфеш бшоъ даршвйд ебдщъреъ чцб дмб елп дййъд омеед бйшйгд бшоъ дъсойрйн лое ъщйщеъ, тцйшеъ ебзймеъ ебтмййд богг айлеъ дзййн. дзечшйн ослойн лй ооцайн амд оцбйтйн тм йтймеъ дфешоемд мдвбшъ даршвйд емщйфеш доцб двефрй бчшб земй сшип доиефмйн блйоеъшфйд, аемн ргшщйн озчшйн бдйчу вгем йеъш ебайлеъ вбедд йеъш тм оръ мащщ аъ досчреъ.
https://www.ncbi.nlm.nih.gov/pubmed/27912948
бозчш течбд (афшйм 2015) бе рлмме л-26,000 земеъ сшип дщг доиефмеъ биоечсйфп роца лй рщйн дреимеъ ъшефеъ сйрйеъ цозйеъ долймеъ чеосишем, врйсиайп ае гайгжйп айрп бтмеъ сйлеп вбед йеъш мдъфъзеъ сшип дшзн.
http://www.ncbi.nlm.nih.gov/pubmed/25934515
оид-армйжд (йреаш 2016) дослоъ аъ дооцайн осчйшеъ щм озчшйн ачшаййн обечшйн ащш бзре аъ дйтймеъ щм шфеаъ цозйн сйрйъ мщйфеш айлеъ дзййн бчшб земй сшип шйаеъ осев NSCLC (чйцеш щм Nonsmall Cell Lung Cancer) лийфем ъеок йзг тн лйоеъшфйд, бдщееад млйоеъшфйд бмбг.
боид-армйжд рлмме 14 счйшеъ длеммеъ 61 озчшйн тн 4,247 ощъъфйн.
обйп 11 фешоемеъ щрбгче, 6 фешоемеъ роцае йтймеъ: Kang-lai-te injection, Shei-qi-fu-zheng injection,Shen-fu ingection, Zi-jin-long tablet, Compound Ku-shen injection (долйм сефешд), Kang-ai- injection (долймд асишвмес). озчш ресу оцбйт тм дйтймеъ щм дфешоемд Hai-shen-su доефчъ озмбеп доцей бцгфд Tegillarca granosa. дзечшйн чешайн мчйен озчшйн ресфйн лфемй-сойеъ обечшй фмсбе тм оръ мащщ аъ дооцайн мвбй дйтймеъ щм шфеаъ цозйн сйрйъ мземй сшип шйаеъ.
http://www.ncbi.nlm.nih.gov/pubmed/26735544
озчш фшд-чмйрй (аевеси 2016) бе рбгчд ддщфтд дсйршвйсийъ щм фешоемд сйрйъ згщд SH003 мдвбшъ дщфМтъ длйоеъшфйд мийфем бсшип щг щмймй мчемирйн дешоермййн. дфешоемд SH003 обессъ тм ойцей:
Astragalus membranaceus ,Angelica gigas ,Trichosanthes kirilowii Maximowicz.
бозчш чегн оцае дзечшйн лй дфешоемд дййъд йтймд мтйлеб дцойзд щм двйгем дсширй.
бозчш дрелзй щртшк тм гвйоеъ ъайн, ошайн дзечшйн лй мфешоемд дщфтд сйршвйсийъ тн дъшефд длйоеъшфйъ гечсешебйцйп, бтйгег ъоеъъ ъайн сширййн етйлеб цойзъ двйгем.
http://www.ncbi.nlm.nih.gov/pubmed/27476488
бозчш сиийсий (аевеси 2016) дтшйле дзечшйн одй дъшеод щм дщйоещ бшфеаъ цозйн сйрйъ мдйщшгеъ оиефмйн тн сшип чйбд оъчгн (щмб 4) еодн дшлйбйн дйтймйн бйеъш бфешоемеъ бдн ртщд щйоещ.
бозчш рлмме 154 оиефмйн, щчйбме ийфем лйоеъшфй мфзеъ щмещ фтойн, е-58 обйп доиефмйн чйбме вн ийфем цозй. ощк ддйщшгеъ дзцйерй щм лмм доиефмйн дйд 12 зегщйн, лащш ощк ддйщшгеъ щм доиефмйн щчйбме ийфем цозй дйд 18 зегщйн, мтеоъ 9 зегщйн бчшб оиефмйн щчйбме аъ дийфем дчербрцйерамй бмбг (p<0.001).
дзечшйн жйде 13 цозй ошфа, обйп 204 цозйн щрлмме бфешоемеъ, ащш дйе чщешйн бъецаеъ дзйебйеъ щм дийфем, бйрйдн щещ чйшз (Glycyrrhiza glabra), чтшешйъ бшбид (Scutellaria barbata), чтшешйъ сйрйъ (Scutellaria baicalensis), чегерефсйс (Codonopsis pilosula), цмт дщеш (Bupleurum spp), ошеед сйрйъ (Salvia miltiorrhiza) елешлен (Curcuma longa).
дзечшйн осбйшйн одн досмемйн дбйемевййн еорврерй дфтемд ащш чщешйн бдщфтд дойийбд щм цозйн амд. дн ослойн лй ооцай дозчш оцбйтйн тм цозй ошфа лбтмй феирцйам мийфем бсшип дчйбд еодеейн бсйс мозчшй дощк емфйъез ийфемйн згщрййн.
https://www.ncbi.nlm.nih.gov/pubmed/27583849
счйшд (йерй 2018) оецвйн дооцайн дтглрййн мвбй шлйбйн доцеййн бцозй ошфа сйрййн, ащш тщеййн мъшен мдъоеггеъ тн бтййъ дтойгеъ млйоеъшфйд, лвеп Gambogic acid, лешлеойп, Tanshinon, чеешцийп, в'йрсресйгйн, Tetramethylpyrazine, шжбшишем ефешоемеъ сйрйеъ щереъ.
https://www.ncbi.nlm.nih.gov/pubmed/29860581
счйшд (фбшеаш 2015) доцйвд аъ дтгейеъ бревт мщйоещ бшфеад сйрйъ осешъйъ лийфем ощмйн бщмбйн дщерйн щм озмъ дсшип. роца лй йщрн ийфемйн (TJ-41, Liu-jun-zi-tang, PHY906, Coumarin, Aescine) ащш роцае йтймйн мдчмд тм ъсойрйн мазш рйъез лвеп ъщйщеъ, лаб, ъйабеп, щмщем, бзймеъ, дчаеъ емйофгод. ийфемйн осейойн (в'йрсрв, асишвмес, чтшешйъ бшбид, TJ-48, джшчъ Huachansu, джшчъ Shenqi fuzheng, джшчъ Kanglaite) ъешойн мдвбшъ йтймеъ дийфем длйоеъшфй ае ийфемй дчшйрд емдфзъъ ъефтеъ дмееай едсйбелйн лъецад одийфем.
баефп лммй, щймеб щм шфеад сйрйъ бийфем бземй сшип роца йтйм мтцйшъ дъчгоеъ двйгем, мдчмд тм дсйбелйн, мдвбшъ йтймеъ дийфем, мщйфеш дъвебд дзйсерйъ емдфзъъ дфвйтд лъецад одийфем дфемщрй.
щйоещ бшфеа сйрйъ дйд йтйм мдфзъъ мйофгод бземеъ сшип щг, мдфзъъ ъщйщеъ елаб, мдфзъъ дфвйтд бгшлй дрщйод едтйлем лъефтеъ мееай щм дийфем, мдврд тм длбг, еау мщйфеш дгйлей щм оз дтцн.
http://www.ncbi.nlm.nih.gov/pubmed/25787906
счйшд (оай 2015) доъочгъ босфш фешоемеъ цозй ошфа сйрйеъ бтмеъ дщфтд арий-сширйъ, бдъбсс тм дщЃфтъп тм оееъ ъайн сширййн (афефиежйс).
http://www.ncbi.nlm.nih.gov/pubmed/26056434
озчш щртшк тм зйеъ отбгд (афшйм 2015) бе рбгчд ддщфтд щм дфешоемд дсйрйъ SQDBT (чйцеш щм Shi Quan Da Bu Tang) мазш дсшъ вйгем сширй шащерй.
дфешоемд леммъ 12 цозй ошфа: Panax ginseng, Atractylodes macrocephala, Wolfiporia extensa, Glycyrrhiza glabra, Rehmannia glutinosa prepatarta (Shu di huang), Paeonia lactiflora, Angelica sinensis, Ligusticum chuanxiong, Cinnamomum cassia, Astragalus membranaceus, Zingiber officinale, Ziziphus jujube.
бтлбшйн щчйбме аъ дфешоемд роца тйлеб бдъфъзеъ ъай сшип вшешъййн блбг. отбш млк, дзечшйн жйде оде дшлйб едорвреп дтеог ббсйс дщфтд жаъ. озчш жд оцбйт тм лк щвешн двгймд дщмййъй (placental growth factor) дчщеш бъдмйлй арвйевржд тщей мдееъ оишд мийфем бсшип вшешъй.
http://www.ncbi.nlm.nih.gov/pubmed/25895458
дфешоемд Shenling Baizhu San (бчйцеш: SBS) дйа фешоемд доелшъ бшфеад дсйрйъ мийфем бдфштеъ тйлем лбш оаеъ щрйн. дфешоемд олймд 10 цозй ошфа: Panax ginseng, Atractylodes macrocephala, Wolfiporia extensa, Glycyrrhiza glabra, Dioscorea opposite, Dolichos lablab, Nelumbinis Nucifera, Coix lacryma-jobi, Amomum, Platycodon grandifloras.
бозчш дрелзй (афшйм 2015), ащш ртшк бчшб зйеъ отбгд, оцйвйн дзечшйн одн орврерй дфтймеъ бдн дфешоемд ъешоъ мдфзъъ дъоеъд едъфъзеъ вйгемйн сширййн ботй лсйбек щм чемйийс.
http://www.ncbi.nlm.nih.gov/pubmed/25897964
озчш щртшк тм зйеъ отбгд (аевеси 2014) оцбйт тм ддщфтд щм фешоемъ цозй дошфа дсйрйъ Chang-Wei-Qin мдвбшъ дйтймеъ щм дъшефд дарий-сширйъ Oxaliplatin.
http://www.ncbi.nlm.nih.gov/pubmed/25103530
озчш щртшк тм зйеъ отбгд (ошх 2015) оцбйт тм дйтймеъ щм дфешоемд дсйрйъ PHY906-KD018 мщйфеш дфтймеъ дарий-сширйъ щм дъшефд Sorafenib.
http://www.ncbi.nlm.nih.gov/pubmed/25819872
бозчш шишесфчийбй (аевеси 2016) рбгчд дйтймеъ щм дошъз Jianpi Ligan лийфем ъеок мземй сшип лбг шащерй щма рйъп млшйъд (unresectable hepatocellular carcinoma).
бозчш рлмме 103 земйн, ащш чйбме ийфем лйоеъшфй ййзегй доежшч йщйшеъ мтешч длбг (transarterial chemoembolization) ббйъ земйн бсйп бйп дщрйн 2007-2013. обйп дземйн, 50 чйбме аъ длйоеъшфйд бмбг е-53 чйбме ийфем ощемб щм лйоеъшфйд еошъз. дошъз лмм тщшд цозй ошфа: чегерефсйс (Codonopsis pilosula), аишчиймегс (Atractylodes macrocephala), фишййъ фешйд (Poria cocos), щещ чйшз (Glycyrrhiza glabra) бииъ бш (Dioscorea villosa), фйрмйд (Pinelliae Ternatae),тежшш (Crataegus spp), жштй меиес (Nelumbinis), мтрд (Artemisia scoparia) е-Pericarpium Arecae.
роца лй дземйн щриме аъ дийфем дощемб рие фзеъ мтцйшеъ, рфйзеъ бирйъ едтгш ъйабеп, бдщееад мземйн щриме аъ длйоеъшфйд бмбг. лое лп, дземйн бчбецъ дийфем дощемб рие фзеъ мштймеъ блбг емдфштеъ бгшлй дтйлем, лвеп бзймеъ едчаеъ. щйтеш дцмзъ дийфем дйд вбед йеъш (51/53 земйн мтеоъ 40/50 бчбецъ длйоеъшфйд бмбг) ещйтеш ддйщшгеъ маешк 3 щрйн дйд вбед йеъш (38% мтеоъ 26%).
дзечшйн ослойн лй риймъ дошъз дййъд йтймд мдфзъъ ддщфтеъ дщмймйеъ щм дийфем емщйфеш ддйщшгеъ тбеш земй сшип лбг вшешъй.
https://www.ncbi.nlm.nih.gov/pubmed/27536066
зжшд мъзймъ дозчшйн
щорйн аъшййн
бсчйшд щйиъйъ (2019) детшлд ддщфтд щм ашеоъшфйд мийфем бъсойрйн ебдщфтеъ щмймйеъ, бчшб земй сшип. бсчйшд рлмме 43 озчшйн, бдн 3,239 земй сшип о-13 огйреъ, лащш 31 одозчшйн дйе ачшаййн обечшйн. б-21 одозчшйн ртщд щйоещ башеоъшфйд бдшзд, б-22 одозчшйн бтйсей ашеоъшфй ебщмещд озчшйн - бщйиеъ азшеъ. сд"л ртщд щйоещ б-32 севй щорйн, дщлйзйн бйеъш дйе мбргш (18 озчшйн), чоеойм (6 озчшйн) ев'йрв'ш (5 озчшйн).
одъецаеъ темд лй щйоещ башеоъшфйд ъшн мдчмд бовееп шзб щм ъсойрйн вефрййн ерфщййн щрбгче - лемм зшгд, лаб, айлеъ зййн, бзймеъ едчаеъ, гйлаеп, дчмд бъсойрйн фсйлемевййн евефрййн, айлеъ дщйрд, тййфеъ, сйорйн ейиамййн, оечежйийс бфд, дфштеъ тешйеъ, ъзещъ шеезд, оцб ъжеръй, оггйн зйсерййн, оцб шез, тцйшеъ, фвйтд ббмеиеъ дшеч, гмчъ ешйгйн тм шчт лйоеъшфйд, ешоъ чешийжем ефшемчийп. йзг тн жаъ, дзечшйн оцййрйн лй босфш озчшйн ма роцад дщфтд машеоъшфйд тм дъвебд дтешйъ.
дооцайн дчййойн оцбйтйн тм дфеирцйам щм ашеоъшфйд лийфем ъеок мдчмд тм ъсойрйн едщфтеъ щмймйеъ бчшб земй сшип, аемн ргшщйн озчшйн ресфйн тм оръ мбсс аъ фшеиечем дийфем еаъ сев дашеоъшфйд едойрерйн дргшщйн.
https://pubmed.ncbi.nlm.nih.gov/31779991/
бсчйшд щйиъйъ (2019) детшлд ддщфтд щм ашеоъшфйд тм дъфъзеъ сйбелйн бчшб земй сшип. бсчйшд рлмме 43 озчшйн (31 оъелн дйрн ачшаййн обечшйн), ащш фешсое бйп дщрйн 1995-2019 ебдн 3,239 земй сшип о-13 огйреъ. б-21 одозчшйн ртщд щйоещ башеоъшфйд бдшзд бойреп щм бйп 1 м-6 ийфеъ мощк 2-20 гчеъ. б-22 одозчшйн ртщд щйоещ бтйсей бойреп щм 2-50 о"м / 3-10 ийфеъ, лащш бщмещд одозчшйн ртщд щйоещ ощемб бдшзд ебтйсей, ебщмещд озчшйн ресфйн ртщд щйоещ бщйиеъ азшеъ лвеп аоби ае вшвеш. бозчшйн дщерйн ртщд щйоещ бщоп бегг ае бътшебъ щорйн, сд"л рлмме мотмд о-32 севй щорйн, лащш дщорйн дщлйзйн бйеъш дйе мбргш (18 озчшйн), чоеойм (6 озчшйн) ев'йрв'ш (5 озчшйн). дсйбелйн щрбгче лмме сйбелйн фсйлемевййн ае вефрййн.
роца лй машеоъшфйд дййъд дщфтд ойийбд тм овееп шзб щм ъсойрйн есйбелйн бчшб земй сшип, лемм зшгд, лаб, айлеъ зййн, бзймеъ едчаеъ, гйлаеп, айлеъ щйрд, тййфеъ, оггйн ейиамййн, оечежйийс бфд, ъсойрйн тешййн, ъзещъ шеезд, оцб ъжеръй, оггйн зйсерййн, оцб шез, тцйшеъ, етег.
дзечшйн ослойн лй ооцайн амд оцбйтйн тм дфеирцйам щм щймеб ашеоъшфйд бийфем бземй сшип, аемн ргшщйн озчшйн ресфйн тм оръ мдвгйш богейч аъ фшеиечем дийфем едойрерйн дойибййн.
https://www.sciencedirect.com/science/article/abs/pii/S0965229919308647
озчш чмйрй (аевеси 2014) бе рбгчд дъшеод щм ашеоъшфйд етйсей мщйфеш дъсойрйн еайлеъ дзййн бчшб земеъ сшип дщг ащш тбше ийфемй лйоеъшфйд.
бозчш рлмме 280 рщйн щиефме блйоеъшфйд ббйъ земйн фший биешчйд. дощъъфеъ земче ачшайъ м-3 чбецеъ дийфем: дшзд щм щорйн аъшййн, тйсей чмасй ае тйсей ашеоъшфй, емчбецъ дбйчешъ щчйбмд шч аъ дийфем дщвшъй бйзйгъ длйоеъшфйд ббйъ дземйн.
дийфем бдшзд лмм щдййд бзгш свеш мощк 5 гчеъ 3 фтойн бщбет мощк зегщ едшзъ ътшебъ щм щоп мбргш, орид, чоеойм, йсойп, сДйвмйеъ, шежошйп еачмйфиес бйзс щм 2:2:2:1:1:1, бшйлеж щм 1.1% одемд бщоп щчгйн. дтйсей дчмасй рощк 35 гчеъ 3 фтойн бщбет мощк зегщ елмм щйоещ бщоп жйъ мтеоъ дтйсей дашеоъшфй щбецт баеъд цешд ак тн ътшебъ дщорйн лое бчбецъ ддшзд.
мазш 6 е-10 щбетеъ оъзймъ дийфем роцад дщфтд зйебйъ блм чбецеъ дийфем лащш роца дбгм миебъ чбецеъ дийфем бдщееад мчбецъ дбйчешъ бйзс мцйерй ъзеой айлеъ дзййн: ъзещъ шеезд лммйъ, ъйабеп еъфчег ойрй (p<0.001) елп бйзс мъсойрйн фйжйемевййн ешоъ фтймеъ, сйет шфеай ецйеп айлеъ дзййн длммй (p<0.05). ма роцае дбгмйн бйзс мъзеой дщйрд, ъфйсд тцойъ есбйбъйъ, йзсйн збшъййн еъфчег бтбегд.
баефп сфцйфй, бчбецъ дбйчешъ змд йшйгд бцйеп айлеъ дзййн длммй (о-123.2 м-112.5) мтеоъ тмййд бчбецъ ддшзд, дтйсей дчмасй едтйсей дашеоъшфй (о-117.4 м-123.0, о-125.8 м-136.0 ео-110.9 м-146.0, бдъаод). овод геод роцад бйзс мцйеп дъсойрйн дфсйлемевййн едфйжйемевййн елп бйзс мцйеп дъсойрйн длммй ащш дзойш бчбецъ дбйчешъ (о-60.8 м-67.2) мтеоъ щйфеш бчбецеъ дийфем, ебойезг бчбецъ дтйсей дашеоъшфй (о-65.5 м-61.0 бчбецъ ддшзд, о-60.3 м-54.8 бчбецъ дтйсей дчмасй ео-67.3 м-47.3 бчбецъ дтйсей дашеоъшфй).
аеорн тйсей ашеоъшфй дйд дйтйм бйеъш ак дзечшйн оцйтйн лй дшзд щм щорйн аъшййн ае тйсей бщоп жйъ тщеййн мдйеъ йтймйн боцбйн бдн джоп оевбм ае щщорйн аъшййн айрн жойрйн.
http://www.ncbi.nlm.nih.gov/pubmed/25157942
бозчш ъцфйъй детшлд ддщфтд щм сфшйй ау долйм щоп аъшй шеж-вшрйен тм бсйс щоп щеощен мдчмд тм ъсойрйн бзмм дау бчшб земеъ сшип дщг дтебшеъ ийфемйн лйоеъшфййн. бдъбсс тм дшщеоеъ дшфеайеъ, дзечшйн айъше земеъ сшип щг ащш чйбме домцд мдщъощ бсфшйй шеж-вшрйен ещмзе мдп щамеп мдтшлъ дийфем. обйп 40 доиефмеъ, 20 оиефмеъ дщмйое аъ дщамеп. дъсойрйн дтйчшййн бзмм дау тмйдн гйеезе доиефмеъ лмме гйоен (90%), йебщ (86%), лаб (81%), вшг (67%) ефцтйн (52%).
лм доиефмеъ ащш дщъоще бсфшйй гйеезе тм дчмд бъсойрйн, оиефмъ азъ гйеезд тм дчмд чмд, 11 оиефмеъ гйеезе тм дчмд бйрерйъ е-8 оиефмеъ гйеезе тм дчмд ощотеъйъ етг дйтмоеъ омад щм дъсойрйн. дзечшйн оцййрйн лй баефп лммй дийфем рсбм дйиб. дзечшйн ослойн лй сфшйй ау долйм щоп шеж-вшрйен тщей мдчм тм ъсойрйн бзмм дау дчщешйн бийфемй лйоеъшфйд.
дтшъ отшлъ: огебш бозчш ъцфйъй ема дътшбеъй елп мма чбецъ бйчешъ.
https://www.ncbi.nlm.nih.gov/pubmed/30377210
бозчш фйймеи ачшай обечш фъез (2020) рбгчд ддщфтд щм щоп орид мдчмд тм бзймеъ едчаеъ, бчшб земй сшип дочбмйн ийфемй лйоеъшфйд. бозчш рлмме 90 оиефмйн, ащш земче ачшайъ мчбецъ ддътшбеъ ае мчбецъ дбйчешъ. дощъъфйн бчбецъ ддътшбеъ дъбчще мщйн ийфд азъ одщоп (щоп орид бшйлеж 3% тм бсйс щоп щчгйн) оъзъ мау, щмещ фтойн бйен бощк зойщд йойн мазш дийфем длйоеъшфй, бресу мийфем дчербрцйерамй щрйъп морйтъ бзймеъ едчаеъ. дощъъфйн бчбецъ дбйчешъ чйбме аъ дийфем дчербрцйерамй бмбг. дощъъфйн дъбчще мгеез тм зеошъ дбзймд тм семн щм 0 тг 10.
роца лй бдщееад мчбецъ дбйчешъ зм щйфеш оебдч бзеошъ дбзймд бчшб доиефмйн бчбецъ ддътшбеъ ащш чйбме севйн щерйн щм лйоеъшфйд (Folfirinox, Paclitaxel-Trastuzumab, Carboplatin-Paclitaxel, Cyclophosphamide-Adriamycin), омбг оиефмйн щчйбме лйоеъшфйд одсев Cisplatin. овод геод роцад богг (INRV (Index of Nausea, Vomiting, and Retching.
дзечшйн ослойн лй щоп орид тщей мдйеъ йтйм, лийфем ощмйн, мдчмд тм бзймеъ едчаеъ тм шчт ийфемй лйоеъшфйд.
https://pubmed.ncbi.nlm.nih.gov/33197662/
озчш фйймеи (ошх 2014) бе рбгчд ддщфтд щм ътшебъ щорйн аъшййн, мтеоъ дийфем дсиргший, тм дъвебд дтешйъ щм земеъ сшип дщг, дтебшеъ ийфемй чшйрд.
босвшъ дозчш 24 оиефмеъ земче ачшайъ мийфем дсиргший (ощзд RadiaPlexRx™) ае мщйоещ бътшебъ щорйн аъшййн бошйзд зйцерйъ 3 фтойн бйен, тг зегщ мазш сйен ийфемй дчшйрд.
дътшебъ лммд 4 щорйн аъшййн: дмйчшйсен (2.5%), мберд (5%), мбргш (5%) евшрйен (5%) брща щм щоп зезебд (32.5%), амеешд (30%), ъоре (10%) ерш дмймд (10%).
доиефмеъ ръбчще мошез аъ дщоп тг лгй лйсей лм айжеш ддчшрд 3 фтойн бйен (бечш, аоцт дйен емфрй дщйрд) тг фвйщъ дотчб щмдп, щдъчййод лтбеш зегщ. лое лп, дп ръбчще мдсйш аъ дщоп тм йгй щийфд тн ойн есбеп мфрй ддчшреъ тцоп.
дзечшйн дтшйле аъ дъвебд дтешйъ огй щбет едощъъфеъ дъбчще мома щамеп айлеъ зййн мазш 3, 6 е-10 щбетеъ оъзймъ дийфем.
роца лй дщйоещ бщорйн аъшййн дйд бтм йтймеъ геод мийфем дсиргший дп обзйръ дъвебд дтешйъ едп обзйръ щбйтеъ дшцеп еайлеъ дзййн.
http://www.ncbi.nlm.nih.gov/pubmed/24668063
зжшд мъзймъ дозчшйн
ъесфй ъжерд
лммй | аеЙовд 3 | еДйиойп D | зеМоцд фемДйъ | смрйеМн
лммй
оид-армйжд щм озчшй течбд фшесфчийбййн (оай 2016) ащш ретгд мдтшйк аъ дчщш бйп шоъ цшйлъ дсйгп (оъжерд еъесфйн) мбйп дсйлеп мсшип дщг. рйъез дръерйн обесс тм 11 озчшйн длеммйн 26,606 очшйн щм сшип дщг обйп л-873,000 рщйн тн ъчефъ отчб щм мфзеъ 7 щрйн. баефп лммй роца лй рщйн тн дшод двбедд бйеъш щм цшйлъ сйгп (345-1750 о"в ае йеъш) дйе бсйлеп роек бл-8% мсшип дщг бдщееад мшод дроелд бйеъш щм цшйлъ дсйгп (203-807 о"в ае фзеъ). чщш жд дйд ощотеъй тбеш очшйн щм сшип дщг мфрй вйм дотбш (сйлеп оефзъ щм 25% мтеоъ 6% азшй вйм дотбш). брйъез дръерйн мфй ойреп роца лй лм тмййд щм 300 о"в/йен бцшйлъ дсйгп дййъд чщешд бйшйгд щм 2% бсйлеп длммй мсшип щг ебйшйгд щм, 8% е-2% бсйлеп мсшип дщг мфрй вйм дотбш еазшй вйм дотбш, бдъаод. дтшъ дотшлъ: бтег щойрерйн вбедйн щм сйгп роцае бозчш жд оешйгйн сйлеп мсшип щг, бозчшйн азшйн щбгче дщфтеъ щм ъесу сйгп роца сйлеп оевбш моееъ оозмеъ мб елмй гн. реща бийзеъ дщйоещ бъесфй сйгп бойрерйн вбедйн тгййп айре бшеш ейщ мдощйк мтчеб азш дозчшйн бреща.
http://www.ncbi.nlm.nih.gov/pubmed/27170091
бсчйшд щйиъйъ щм озчшйн чмйрййн (2020) детшлд дйтймеъ щм фмбереайгйн лзмч одийфем ревг дсшип. дзечшйн осбйшйн лй мфмбереайгйн феирцйам мийфем бсшип бщм фтймеън дсмчийбйъ лрвг ъайн сширййн, мма фвйтд бъайн бшйайн. бсчйшд рлмме 22 озчшйн чмйрййн бщмб 2 еозчш азг бщмб 3, бдн ртщд щйоещ бфмбереайгйн лрвг вйгемйн сширййн ае лрвг сшип гн емйофд. одсчйшд темд лй дшлйб дщлйз бйеъш бе ртщд щйоещ деа Flavopiridol ъек-ешйгй бойреп 50 mg/m2. роца лй баефп лммй щйтешй дъвебд дйе роелйн, аемн дщйоещ бфмбереайгйн дйд омеед бъецаеъ зйебйеъ йеъш боцбйн щм сшип гн емйофд мтеоъ вйгемйн сширййн семйгйн:
- сшип гн емйофд - ъвебд омад бчшб 140 оиефмйн еъвебд змчйъ бчшб 88 оиефмйн обйп сд"л 615 оиефмйн б-11 озчшйн.
- вйгемйн сширййн семйгйн - ъвебд омад бчшб 4 оиефмйн еъвебд змчйъ бчшб 21 оиефмйн обйп сд"л 525 оиефмйн б-12 озчшйн.
дзечшйн ослойн лй дййъд щереъ вгемд бйп дозчшйн, ергшщйн озчшйн ресфйн тм оръ мдбйп аъ ддщфтд дойийбд щм фмбереайгйн бчшб земй сшип.
https://pubmed.ncbi.nlm.nih.gov/31752046/
бсчйшд щйиъйъ щм озчшйн фшд-чмйрййн (2021), детшле дтгейеъ дозчшйеъ бдъййзс мфтймеъ ревгъ дсшип щм ъйарйп оочеш ибтй. ъйарйп дйрд зеоцд аойрйъ доцейд бтйчш бъд, лащш озчшйн чегойн дгвйое аъ дщЙАфтъд дбшйаеъйъ дойийбд бдъййзс моцбйн лвеп щореъ, селшъ, ъзмеад чшгйеесчемшйъ, ъфчег чеврйийбй етег. йщрп тгейеъ шбеъ мдщфтд ревгъ дсшип щм ъд ешлйбйе дфтймйн, лвеп феЙмйфреЙмйн, аемн ма рбгчд дйтймеъ щм ъйарйп идеш оочеш ибтй морйтд ае ийфем бсшип. бсчйшд рлмме 14 озчшйн щртшле тм гвйоеъ ъайн ае боегмйн щм зйеъ отбгд. бошбйъ дозчшйн жедъд фтймеъ ревгъ сшип, лемм дщфтд ойийбд тм ъдмйлй щвщев ъай сширййн, ъоеъъ ъайн, щмйзъ вшешеъ, ргйгд ефмйщд, лащш боегмйн щм зйеъ отбгд роцад ъойлд мъшеод щм ъйарйп морйтъ дъфъзеъ едъфщиеъ двйгем. босвшъ дсчйшд грйн дзечшйн борврерй дфтемд дбйемевййн дотешбйн. дзечшйн ослойн лй ооцайн амд оцбйтйн тм дфтймеъ ревгъ дсшип щм ъйарйп, ергшщйн озчшйн ресфйн мбйшеш дйтймеъ морйтъ сшип ембзйръ дорврерйн дотешбйн боегмйн зййн.
https://pubmed.ncbi.nlm.nih.gov/33891786/
бсчйшд (2021) грйн дзечшйн бййщеойн дчмйрййн щм че-аржйн Q10 бовееп оцбйн бшйаеъййн, отбш мъзмеад чшгйеесчемшйъ. че-аржйн Q10 дйре че-фчиеш зйерй бъдмйк дрщйод дъайъ (бщмб долерд жшзеп зоцерй) ащш роца бшйлеж вбед блбг, бмб еблмйеъ. мче-аржйн Q10 фтймеъ ревгъ гмчъ еревгъ зоцеп, досййтъ морйтъ дфвйтд дзоцерйъ щм шгйчмйн зефщййн еъдмйлйн гмчъййн. мфйлк, озчшйн щерйн дгвйое лй шйлеж вбед йеъш бгн щм че-аржйн Q10 дйре бтм дщфтд ойийбд бовееп оцбйн бшйаеъййн. босвшъ дсчйшд офешийн дооцайн дчмйрййн бдъййзс мдщфтд щм че-аржйн Q10 бдъййзс мойвшрд; моцбйн щерйн щм тййфеъ; мозмеъ рейше-гвршийбйеъ лемм фшчйрсеп, дрийрвиеп, амцдййош, ишщъ рфецд ерейшефъйд; мсшип; мфешйеъ; мозмъ гефйишп; емслйжефшрйд. бдъан мооцайн дчййойн, дзечшйн чебтйн лй че-аржйн Q10 дйре ъесу ашвеврй (ощфш бйцетйн) бтм фшефйм бийзеъ вбед вн бзщйфд лшерйъ щм 900 о"в мйен емма ъвебеъ дггйеъ фшочемевйеъ йгетеъ. зсш роца чщеш боцбйн фъемевййн, дтйчшй бдн дйре ъзмеад чшгйеесчемшйъ, еъйсеу тщей мъшен мщйфеш айлеъ дзййн еау мщйфеш дъецаеъ дчмйрйеъ. дн ослойн лй оцг азг тгейеъ чмйрйеъ ъеолеъ бдщфтд дойийбд щм риймъ че-аржйн Q10 бойреп щм мфзеъ 200 о"в/йен бдчщш дчшгйеесчемшй. оцг щрй, дтгейеъ мвбй дщйоещ бъесфйн бдчщш щм озмеъ рейше-гвршийбйеъ, сшип ае оцбйн бшйаеъййн азшйн дйрп обийзеъ аемн айрп осфйч обессеъ. мфйлк, дооцайн дофешийн бсчйшд оцбйтйн тм дфеирцйам щм дщйоещ бъесфй че-аржйн Q10 бдчщшйн щайрн чшгйеесчемшййн.
дзечшйн огеезйн тм дтгш ойоеп зйцерй мозчш.
https://pubmed.ncbi.nlm.nih.gov/34067632/
озчшйн афйгойемевййн оцбйтйн тм чщш бйп цшйлъ йшчеъ ефйшеъ баефп лммй, ак ма бйп ъшлебеъ фремйеъ осейоеъ, мбйп сйлеп роек йеъш мсшип чемешчимй. мтеоъ жаъ, озчшйн фшд-чмйрййн бдн ртщд щйоещ бгвйоеъ ъайн ае бзйеъ отбгд оцбйтйн тм дфтймеъ дарий-сширйъ щм ъшлебеъ фремйеъ щочешп бъжерд.бозчш дрелзй (ошх 2015) безрйн дзечшйн аъ лмм дтгейеъ бйзс мдщфтд дарий-сширйъ щм ъшлебеъ фремйеъ щереъ, ъек дъочгеъ блешлеойп, шжбшишем, айжефмберйн, EGCG, абчъ фим щзеш, ойцей аелорйеъ щзешеъ, ойцей в'йрв'ш еойцей шйоеп.одсчйшд темд лй лешлеойп дйре дшлйб дъжеръй добийз бйеъш лийфем ъеок бсшип чемешчимй. дзечшйн ослойн лй баефп лммй озчшйн чмйрййн осфчйн ъойлд чмещд мвбй дйтймеъ щм ъшлебеъ фремйеъ лрвг сшип чемешчимй еосбйшйн лй ргшщйн ойрерйн вбедйн оаег тм оръ мвшен мдщфтд бтмъ ощотеъ чмйрйъ.
http://www.ncbi.nlm.nih.gov/pubmed/25693744
бозчш чмйрй щртшк бчшб 12 земй сшип дсебмйн олабйн рейшефъйн, ойреп щм 500 о"в ае 1 вшн овржйен семфаи ъек ешйгй дрйъп баефп зг фтой, дфзйъ бойгд рйлшъ аъ ъсойрй длаб мощк тг 4 щтеъ ошвт чбмъ дойреп бчшб 11 земйн ероца биез ейтйм мщйоещ.
https://www.ncbi.nlm.nih.gov/pubmed/17172008
озчш (оай 2016) бе рбгче дбгмйн бшйлежй оибемйийн бгн бйп земйн тн вмйебмсиеод (вйгем оезй ооайш), щаебзре тг 22 щрд мазш бйцет бгйчеъ дгн, бдщееад мрбгчйн бшйайн.одъецаеъ темд лй шоеъ вбедеъ йеъш щм ейиойп E чщешеъ бсйлеп оевбш мвмйебмсиеод.
http://www.ncbi.nlm.nih.gov/pubmed/27175595
бсчйшд (2021) детшлд дъойлд дозчшйъ мфшчийчд дщлйзд щм оъп ъек-ешйгй щм ейиойп C бойреп вбед мземй сшип, боишд мдвбйш аъ ддщфтд ревгъ дсшип емдфзйъ аъ ддщфтеъ дщмймйеъ щм длйоеъшфйд. босвшъ дсчйшд дзечшйн офшийн аъ дооцайн ддйсиешййн бдъййзс мфтймеъ ревгъ дсшип щм ейиойп C, грйн бдбгмйн бйп щйоещ ъек-ешйгй мтеоъ риймд феойъ, оъашйн аъ доафййрйн дбйемевййн щм ейиойп C, еаъ шоеъ ейиойп C щроцае бчшб земй сшип сефрййн. бдощк дн грйн бфеирцйам дийфемй щм ейиойп C ъек дъййзсеъ мфтймеъ ревгъ дсшип, мщйфеш йтймеъ длйоеъшфйд, дфзъъ ддщфтеъ дщмймйеъ щм дийфем, щйфеш айлеъ дзййн, дчмд тм ъзещъ дтййфеъ едлаб, елп грйн бдйбийн щм бийзеъ.
одсчйшд темд лй:
-
мошеъ дъецаеъ дзйебйеъ щроцае бозчшйн фшд-чмйрййн бдъййзс мдщфтд ревгъ дсшип, тйлеб дъфъзеъ двйгем ещйфеш ддйщшгеъ, ма роцад ъойлд млк бозчшйн чмйрййн.
-
ма роцад ъойлд чмйрйъ мдвбшъ дйтймеъ щм длйоеъшфйд емдфзъъ ддщфтеъ дщмймйеъ щм дийфем.
-
йзг тн жаъ, бийфем фмйаийбй рйъп мщчем оъп ъек-ешйгй щм ейиойп C бойреп вбед мщйфеш айлеъ дзййн емдчмд тм ъсойрйн лое тййфеъ елабйн бтцоеъ. мошеъ жаъ, бдтгш озчшйн обечшй фмсбе, ма рйъп мчбет лй ддътшбеъ йтймд отбш мафчи дфмсбе.
дзечшйн огеезйн тм дтгш ойоеп зйцерй мозчш етм дтгш рйвегй айришсйн.
https://pubmed.ncbi.nlm.nih.gov/33652579/
счйшд (фбшеаш 2016) доцйвд аъ дтгейеъ бйзс мйтймеъ щм овееп шлйбйн цозййн морйтд еийфем бомреод. дсчйшд оъочгъ бфмберем дрчша fisetin, EGCG, шжбшишем, лешлеойп, фшеаръецйарйгйрйн, сймйошйп, афйврйп, чфсайцйп, врйсиайп, айргем-3-чшбйрем емеиаемйп.
http://www.ncbi.nlm.nih.gov/pubmed/26864554
счйшд (2016) дтесчъ бфтймеъ дарий-сширйъ щм шлйбйн ъжеръййн щерйн, бгвщ тм ъшеоън мийфем бсшип дщг. дсчйшд леммъ фйшеи мвбй зеоцъ щеоп аеовд 3 доефчъ огвйн, шжшбишем доцей бтрбйн е-EGCG доцей бъд йшеч елп оефч одцоз Ziziphus jujube. босвшъ дсчйшд оцйвйн дзечшйн аъ орврерй дфтемд доемчемшййн бдн шлйбйн амд отлбйн ъдмйлйн сширййн, бйрйдн ейсеъ дфтймеъ щм аржйойн ревгй зоцеп ейцйшъ дщфтд арий-фшемйфшийбйъ (тйлеб щвщев ъайн сширййн) еафефиеийъ (тйгег оееъ ъайн сширййн). дзечшйн чешайн мчйен озчшйн ресфйн мдтшлъ дщйоещ дчмйрй бшлйбйн амд лзмч одийфем бсшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/26156544
бозчш лфем-сойеъ обечш фмсбе (2019) детшлд ддщфтд щм ъесу фшебйеийчд оджп Clostridium butyricum бчшб земй сшип шйаеъ дтебшйн лйоеъшфйд. дзечшйн осбйшйн лй лйоеъшфйд февтъ бшйшйъ дотй елъецад олк вешоъ мдщфтеъ щмймйеъ бгшлй дтйлем, лащш йгет лй Clostridium butyricum осййт мдфзъъ ъсойрйн щм щмщем боцбйн лое озмеъ отй гмчъйеъ. бозчш жд рлмме 41 оиефмйн, ащш земче ачшайъ мчбецъ дфшебйеийчд ае мчбецъ дфмсбе. дзм ойен азг мфрй дсбб дшащеп щм длйоеъшфйд, дощъъфйн чйбме 3 ибмйеъ, лм азъ бойреп 420 о"в - щм фшебйеийчд ае фмсбе - 3 фтойн бйен мощк 3 щбетеъ. бгйчеъ гн егвйоеъ цеад расфе бъзймъ дозчш ебсйеое. роца лй зеошъ дбзймеъ еддчаеъ ещйтеш доиефмйн дсебмйн ощмщеМмйн дйе роелйн йеъш бчбецъ дфшебйеийчд мтеоъ дфмсбе. бдъййзс мсфйшъ дгн, роца лй бчбецъ дфшебйеийчд змд йшйгд бйзс рейишефймйн ммйофецйийн ебйзс исйеъ ммйофецйийн, едйзс мйофецйийн моерецйийн дйд вбед йеъш. ма роцае дбгмйн ощотеъййн бйп дчбецеъ бдъййзс мовееп зййгчй дотй, мошеъ щжедъд овод щм тмййд бзййгчйн доййцшйн зеоцеъ щеоп чцшеъ щшщшъ ейшйгд бжрйн фъеврййн бчбецъ дфшебйеийчд, мтеоъ овод дфелд бчбецъ дфмсбе. бресу, роцад тмййд бзййгчйн иебйн оджрйн Clostridium е-Lactobacillus бчбецъ дфшебйеийчд. дзечшйн ослойн лй ооцайн амд огвйщйн аъ дъшеод щм Clostridium butyricum мдфзъъ щмщем еъвебд гмчъйъ тм шчт лйоеъшфйд бчшб земй сшип шйаеъ. дозчш оеоп тм йгй чшп озчш сйрйъ (National Natural Science Foundation of China).
https://www.ncbi.nlm.nih.gov/pubmed/30854059
бозчш, щртшк бчшб земгеъ (ошх 2017), рбгчд дйтймеъ щм ъесу шжбшишем морйтъ фйшеч тцн лъецад оийфем боъеишчсаи, лйоеъшфйд щлйзд бшфеаъ ймгйн аерчемевйъ. босвшъ дозчш земгеъ цтйшеъ чйбме ъесу шжбшишем 7 йойн мфрй дийфем боъеишсаи ебодмк 5 йой дийфем. роца лй оъеишчсаи дебйм мфвйтд босфш оггйн щм бшйаеъ дтцн, лемм тмййд бдйеецшеъ аесиаечмсийн еагйфецйийн довбйшйп фйшеч тцн. риймъ ъесу шжбшишем бойреп 10 о"в/ч"в ощчм веу ма дщфйтд тм бшйаеъ дтцн бчшб земгеъ бшйаеъ, аемн дзойшд аъ дфвйтд бтцн бчшб земгеъ доиефмеъ боъеишачси. тн жаъ, ойреп щм 1 о"в/ч"в орт аъ дфвйтд щм оъеишчсаи боггй бшйаеъ дтцн еорт дйеецшеъ аесиаечмсийн. дщфтеъ оревгеъ амд йлемеъ мдйеъ чщешеъ майришачцйд щм шжшбишем тн доъеишчсаи ае мдщфтд сйршвйсийъ щмдн – бдчщш щм шчоъ дтцн. мазш чшйаъ дсфшеъ бреща дзечшйн оцйтйн лй шжшбишем бойреп роек йлем мфтем лзеош арий-афефиеий, досфч дврд тм дмб ейъшереъ бшйаеъййн азшйн, еайме бойреп вбед йлем мфтем тм ъайн бшйайн есширййн лфше-афефиеий. дзечшйн ослойн лй ооцай дозчш ъеолйн бъшеод щм шжбшишем мдврд тм бшйаеъ дтцн бодмк дийфем боъеишчсаи.
https://www.ncbi.nlm.nih.gov/pubmed/28282956
озчш отбгд (ребобш 2015) ащш оцбйт тм ддщфтд дощотеъйъ щм зййгчй дотй тм йтймеъ дийфемйн дзйсерййн мсшип.
http://www.ncbi.nlm.nih.gov/pubmed/26541610
озчш отбгд (фбшеаш 2015) доцбйт тм дфтймеъ дарий-сширйъ щм ойцей трбйн лрвг ъай сшип дотй.
http://www.ncbi.nlm.nih.gov/pubmed/25705818
озчш отбгд (ошх 2015) доцбйт тм дфтймеъ дарий-сширйъ щм абчъ лшеб сйрй лрвг сшип длбг.
http://www.ncbi.nlm.nih.gov/pubmed/25976785
озчш отбгд (фбшеаш 2015) доцбйт тм дйтймеъ щм ъесу цозй долйм чеешцийп, лешлеойп, ъд йшеч, ойцей йшчеъ оцмйбйн ешжбшишем мийфем бсшип шащ ецееаш бземй аройд т"щ фрчерй (озмд врийъ чщд доъбиаъ бзесш ъай гн).
http://www.ncbi.nlm.nih.gov/pubmed/25695860
бозчш отбгд (фбшеаш 2017) роцад йтймеъе щм ейиойп C лрвг ъай вжт сширййн. баефп сфцйфй, роца лй ейиойп C ъшн мтйлеб ъдмйлй двмйчемйжд бъайн дсширййн елъецад олк морйтъ вгймъ дъа, емлп одеед шлйб обийз мдощк озчш чмйрй.
https://www.ncbi.nlm.nih.gov/pubmed/28223550
лзмч оозчш течбд фшесфчийбй шб-ошлжй (сфиобш 2016), дтесч бсшип дщг, бозчш дрелзй рбгч дан щйоещ бшфеад ощмйод еайрившийбйъ бчшб земеъ сшип дщг чщеш бщйтеш роек йеъш щм дъзмъ ийфем лйоеъшфй.бозчш рлмме 685 рщйн оъзъ мвйм 70 тн сшип щг фемщрй ма вшешъй, лащш 45% одп дйе бтмеъ дъеейд чмйрйъ мчбмъ ийфем лйоеъшфй бдъан мдрзйеъ дмаеойеъ даошйчайеъ. бъзймъ дозчш ртшле шайереъ тн лмм дощъъфеъ бревт мщйоещ бзойщд ъзеойн щм шфеад ощмйод еайрившийбйъ: риймъ ейиойрйн еойршмйн, риймъ цозй ошфа, риймъ шлйбйн ибтййн азшйн, бйцет ъшвем тцой щм илрйчеъ веу-рфщ ае ъшвем илрйчеъ веу-рфщ бдгшлд очцетйъ. дзечшйн тчбе азш дъзмъ ийфемй лйоеъшфйд бодмк ъчефъ отчб щм щрд. обйп лмм дощъъфеъ бозчш, 87% одрщйн (598 рщйн) гйеезе тм щйоещ бшфеад ощмйод еайрившийбйъ. бресу, огйеез тцой щм дрщйн темд лй 89% (272) одрщйн тн дъеейд чмйрйъ мийфем лйоеъшфй алп дзме аъ дийфем бъчефъ дотчб мтеоъ 36% (135) одрщйн мма дъеейд чмйрйъ.
обйп дрщйн тн дъеейд чмйрйъ мийфем лйоеъшфй, роца лй рщйн щрие бойгд шбд мдщъощ бшфеад ощмйод еайрившийбйъ, ебойезг риймъ ъесфй ъжерд ак ма илрйчеъ веу-рфщ, рие фзеъ мдъзмъ ийфем. дзечшйн чешайн мшефайн аерчемевййн мгеп тн доиефмеъ бщйоещ бшфеад ощмйод еайрившийбйъ лзмч оъдмйк чбмъ ддзмиеъ мвбй ийфемй лйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/27243607
боид-армйжд щм озчшй течбд фшесфчийбййн (ошх 2017) рбгч дчщш бйп шоъ дцшйлд щм ейиойп E бъжерд мбйп дсйлеп мсшип шйаеъ. брйъез рлмме 11 озчшйн, бдн сд"л 435,532 ощъъфйн – лащш оъелп 4,164 дн земй сшип шйаеъ. баефп лммй, роца лй ощъъфйн тн дшод двбедд бйеъш щм цшйлъ ейиойп E дйе бсйлеп роек б-16% мдъфъзеъ сшип шйаеъ - бдщееад мощъъфйн тн шоъ дцшйлд дроелд бйеъш. дзечшйн ошайн лй дсйлеп дйд роек б-5% тбеш лм тмййд щм 2 о"в/йен бцшйлъ ейиойп E. чщш жд дйд ощотеъй бойезг бчшб отщрйн, ак ма дйд оебдч сиийсийъ бчшб ощъъфйн щайрн отщрйн ае щтйщре бтбш. дзечшйн ослойн лй ооцайн амд оцбйтйн тм дъфчйг довп щм ейиойп E офрй дъфъзеъ сшип шйаеъ, ллм дршад бщм дщфМтъе ревгъ дзоцеп еревгъ дгмчъ ефтймеъе дарий-сширйъ. тег оцййрйн дзечшйн лй бъжерд дотшбйъ дочеш дтйчшй мейиойп E дйре фемй сейд ещоп сейд, дтщйшйн бвоа-иечефшем, бтег щбъжерд дасйаъйъ дочеш дтйчшй мейиойп E дйре тмйн йшечйн ебйцйн дтщйшйн бамфа-иечефшем.
https://www.ncbi.nlm.nih.gov/pubmed/28244705
бгез тглрй (2017), щфешсн бощеъу тм йгй дчшп дтемойъ мзчш дсшип (AICR) едолеп даошйчай мзчш дсшип (WCRF), ослойн цееъ дзечшйн аъ дтгейеъ дозчшйеъ бревт мчщш бйп ъжерд ефтймеъ вефрйъ мбйп сшип чемешчимй. гез жд, додеед тглеп мгез щфешсн бщръ 2007, лемм 99 озчшйн (щртшле блм дтемн) - бдн л-29 оймйеп ощъъфйн ел-250,000 очшйн щм сшип чемешчимй. тм сок дооцайн щрасфе, дзечшйн ослойн лй чййоеъ тгейеъ обессеъ млк щцшйлъ гврйн омайн (лщмещ ореъ мйен), сйбйн ъжеръййн, оецшй змб (л-500 вш'/йен), риймъ ъесфй сйгп ебйцет фтймеъ вефрйъ ъешойн мдфзъъ дсйлеп мсшип чемешчимй, бтег щцшйлъ бщш аген ебщш отебг, цшйлд щм йеъш ощрй ощчаеъ амледемййн мйен, тегу ощчм, щореъ ечеод вбедд одеейн вешой сйлеп мдъфъзеъ сшип чемешчимй. бресу, дзечшйн ослойн лй чййоеъ тгейеъ осейоеъ мвешой сйлеп ресфйн, ащш чщешйн бсйлеп роек йеъш - лемм цшйлъ ожереъ тщйшйн бейиойп C, цшйлъ гвйн, ейиойп D ериймъ оемий-ейиойрйн, лащш цшйлд роелд (фзеъ о-100 вшн мйен) щм фйшеъ ейшчеъ ма тоймрййн ецшйлъ ожереъ долймйн бшжм осев дн (щочеше бзй) чщешд бсйлеп вбед йеъш мсшип чемешчимй. ма роцае тгейеъ зг-ощотйеъ бдъййзс мвешойн ъжеръййн ресфйн лвеп гврйн, ъфезй агод, щеоп одзй, теу, фйшеъ йн, дшлб зеоцеъ дщеоп, лемсишем, аеовд 3 щочешд бгвйн, чирйеъ, щен, селш оесу, чфд, ъд, фзойоеъ, тоймрйн, теос вмйчой, зеоцд фемйъ, ейиойп A, ейиойп B6, ейиойп E, смрйен, оъйерйп, биа-чшеип, мйчефп, ск дцшйлд дчмешйъ, ъгйшеъ дашезеъ ае гфес дъжерд.
мдтшлъ дзечшйн л-47% оочшй дсшип дчемешчимй рйърйн морйтд баоцтеъ дчфгд тм ъжерд бшйад, бйцет фтймеъ вефрйъ ещойшд тм ощчм ъчйп.
http://www.aicr.org/continuous-update-project/colorectal-cancer.html
бсчйшд (фбшеаш 2016) оселойн дооцайн оозчшйн фшд-чмйрййн ечмйрййн бревт мщйоещ бовееп ъесфй ъжерд ибтййн морйтъ дъфъзеъ сшип дфд елийфем ъеок бщймеб дийфем дарий-сширй дочебм (рйъез, дчшреъ ае лйоеъшфйд). босвшъ дсчйшд оецвйн дооцайн бревт мдщфтд дарий-сширйъ щм шлйбйн аръецйарйрйн, асфшвес, ъд йшеч, ейиойп C бойрерйн вбедйн, мйчефп, змбеп доцей бсейд (Bowman-Birk inhibitor) ечрбйреайгйн. ооцайн амд оцбйтйн тм лк щбйцет щйрей ъжеръй (бтйчш двбшъ дцшйлд щм фйшеъ ейшчеъ), риймъ ъесфйн ревгй зоцеп, ейиойп C бойрерйн вбедйн ещйоещ бчрбйреайгйн тщеййн мъшен мдфзъъ дщлфем щм ъайн сширййн емдвбшъ дсйлей мщйфеш одмк дозмд. дзечшйн ослойн лй лйен тйчш дтгейеъ оъййзсеъ морйтд ергшщйн озчшйн ресфйн тм оръ мбзеп аъ ддщфтд еаъ орврерй дфтемд щм шлйбйн амд еазшйн - дп морйтд едп мийфем.
https://www.ncbi.nlm.nih.gov/pubmed/26863913
бсчйшд (йемй 2017) грйн дзечшйн бъфчйг дафщшй щм ейиойп B3 бдврд офрй сшип дтеш, бщм ъшеоъе мъйчеп ржчй DNA, ейсеъ дсбйбд дгмчъйъ дрецшъ бтеш едфзъъ дфвйтд бфтймеъ дзйсерйъ бтчбеъ зщйфд мчшйрд.
https://www.ncbi.nlm.nih.gov/pubmed/28681504
лзмч оозчш течбд (аевеси 2017), щретг мбзеп аъ дчщш бйп ейиойрйн есшип (VITAL), бозчш дрелзй рбгч дчщш бйп риймд ооещлъ щм ейиойрй B мбйп дсйлеп мсшип шйаеъ. бозчш рлмме 77,118 ощъъфйн бвймай 50-76, одн 808 аебзре тн сшип шйаеъ. дзечшйн бгче аъ дсйлеп мсшип шйаеъ бйзс мойреп дйеой дооецт щм ейиойрйн еоемий-ейиойрйн биеез щм 10 щрйн. бчшб рщйн ма роца чщш бйп риймъ ейиойрй B (зеоцд фемйъ, B6 е-B12) мбйп дсйлеп мсшип шйаеъ. тн жаъ, бчшб вбшйн роца лй риймъ ъесфй ейиойп B6 е-B12 (лъесу рфшг ема лзмч ооемий-ейиойп) дййъд чщешд бтмййд щм 30-40% бсйлеп мсшип шйаеъ. баефп сфцйфй, бдщееад мвбшйн щма риме ъесфйн амд, цшйлд вбедд маешк жоп щм ейиойп B6 (отм 20 о"в/йен) ещм ейиойп B12 (отм 55 оч"в/йен) дййъд чщешд бсйлеп лфем мдъфъзеъ сшип шйаеъ. шоъ дсйлеп дййъд вбедд йеъш тбеш вбшйн отщрйн. тег оцййрйн дзечшйн лй чщшйн амд роцае тбеш лм севй сшип дшйаеъ омбг сшип осев агречшцйреод, дчщеш бойгд дроелд бйеъш мтйщеп.
https://www.ncbi.nlm.nih.gov/pubmed/28829668
бозчш чмйрй (йемй 2017) рбгч дшлб фмешъ дотй бчшб земй сшип дотй двс едетшлд ддщфтд щм ъесу фшебйеийчд тм дшлб дзййгчйн. босвшъ дозчш рмчзд бйефсйд ерасфе гвйоеъ цеад о-15 земй сшип дотй, лащш 8 одн риме ъесу фшебйеийчд бойреп йеой щм 14 оймйашг зййгчйн оджп Bifidobacterium lactis е-7 оймйашг зййгчйн оджп Lactobacillus acidophilus. бресу, рмчзд бйефсйд ерасфе гвйоеъ цеад очбецъ бйчешъ, длеммъ 21 ощъъфйн мма сшип ае мма озмд гмчъйъ ботй. роца лй дшлб дзййгчйн бъайн дсширййн дйд оаефййп бовееп вгем йеъш щм жрйн щерйн, лемм Fusobacterium, Selenomonas е- Peptostreptococcus бдщееад мчбецъ дбйчешъ. лое лп, бчшб земй сшип щриме фшебйеийчд роцад шод вбедд йеъш щм зййгчйн оййцшй беийшаи лвеп Faecalibacterium е-Clostridiales елп шод роелд йеъш щм зййгчйн дчщешйн бсшип чемешчимй лвеп Fusobacterium е-Peptostreptococcus. дзечшйн ослойн лй мземй сшип дотй дшлб ййзегй щм зййгчйн бвйгем дсширй ебшчод дшйшйъ дсоелд, лащш мриймъ фшебйеийчд феирцйам мдщфйт тм дшлб дзййгчйн еблк мъшен модмк дийфем бсшип дотй.
https://www.ncbi.nlm.nih.gov/pubmed/28944067
бсчйшд (аечиебш 2017) оецвеъ дтгейеъ дтглрйеъ бдъййзс мъшеод щм аешз зййн бшйа морйтъ сшип дтшоерйъ, ъек жйдей лйеерй озчш тъйгййн. одсчйшд темд лй йщрн озчшйн фшд-чмйрййн еъцфйъййн дошайн лй мвешой аешз зййн щерйн, лемм ъжерд ефтймеъ вефрйъ, тщей мдйеъ ъфчйг бдаиъ дъчгоеъ дозмд, бцоцен щйтеш дъоеъд ебдфзъъ рим дозмд баефп лммй, бчшб земй сшип тшоерйъ боцб оъчгн. баефп сфцйфй, цшйлд вбедд щм йшчеъ ефйшеъ, дфзъъ дцшйлд щм бщш аген ещеоп шеей едвбшъ дфтймеъ двефрйъ роцае чщешйн бсйлеп роек йеъш мдъфъзеъ сшип дтшоерйъ, мтцйшъ дъчгоеъ дозмд емтмййд бщйтеш ддйщшгеъ. бозчшйн ачшаййн обечшйн роца лй ъесфй смрйен еейиойп C ма дйе йтймйн морйтъ дъфъзеъ сшип дтшоерйъ, елй ъесфй ейиойп E тмемйн ау мдвбйш аъ дсйлеп. дзечшйн оцййрйн лй лйен ртшк озчш вгем, дбезп аъ ддщфтд щм ъжерд тщйшд бйшчеъ бчшб земй сшип дтшоерйъ, еозчш ресу, дбезп аъ ддщфтд щм фтймеъ вефрйъ бчшб земйн тн сшип тшоерйъ вшешъй. дзечшйн ослойн лй чййоъ ъойлд мъшеод щм аешз зййн бшйа морйтъ сшип дтшоерйъ, аемн ргшщйн озчшйн ачшаййн обечшйн тм оръ мдтшйк аъ дйтймеъ дчмйрйъ щм вешойн амд.
https://www.ncbi.nlm.nih.gov/pubmed/29049045
бозчш ачшай обечш (аечиебш 2017) рбгчд дъшеод щм ъесфй сйбйн ефшебйеийчд мийфем бщмщем тм шчт джрд аришмйъ мазш рйъез мдсшъ дзмч дгйсимй щм дчйбд, бчшб оиефмйн тн сшип дчйбд.бозчш рлмме 120 оиефмйн, ащш земче баефп ачшай м-3 чбецеъ: фешоемъ джрд риемъ сйбйн, фешоемъ джрд оетщшъ бсйбйн ефешоемъ джрд оетщшъ бсйбйн бщймеб ъесу фшебйеийчд ащш длйм аъ джрйн Bifidobacterium е-lactobacillus. лм дфешоемеъ рйъре бощк щбтд йойн мазш дрйъез. роца лй осфш доиефмйн щсбме ощмщем дйд роек йеъш бчбецъ дфешоемд дощембъ (5%) оащш бчбецъ дфешоемд доетщшъ бсйбйн бмбг (30%) ебчбецъ дфешоемд риемъ дсйбйн (60%). ма роцае дбгмйн ощотеъййн бйп дчбецеъ бйзс мдфштеъ азшеъ бгшлй дтйлем, лвеп лабй бип бзймеъ едчаеъ. ощк дащфеж дйд ашек йеъш бчбецъ дфешоемд риемъ дсйбйн бдщееад мщъй дчбецеъ дазшеъ. ма роцае дбгмйн бйп дчбецеъ ббгйчеъ дгн, лемм шоъ мйофецйийн, амбеойп ефшд-амбеойп еишрсфшйп. дзечшйн ослойн лй дщймеб щм сйбйн ефшебйеийчд роца йтйм мдфзъъ щмщем бчшб оиефмйн тн сшип чйбд дочбмйн джрд аришмйъ мазш рйъез.
https://www.ncbi.nlm.nih.gov/pubmed/29069041
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн (аевеси 2017) обечшйн детшле дтгейеъ бревт мдщфтд дойийбд щм ъесфй сйгп морйтъ дйщреъ щм агреод чемешчимйъ (вйгемйн щфйшйн ишен-сширййн ботй). бсчйшд рлмме 5 озчшйн бдн 2,234 ощъъфйн тн дйсиешйд щм агреод чемешчимйъ. бозчшйн дщерйн ртщд щйоещ бойреп щм 720-2,000 о"в/йен сйгп аморимй, бдщееад мфмсбе, мъчефъ отчб щм 3 тг 5 щрйн.роца лй риймъ ъесфй сйгп дййъд омеед бсйлеп роек б-12% мдйщреъ двйгем, мма дщфтд оебдчъ тм вйгемйн бщмб оъчгн. брйъез мфй ъъй-чбецеъ роца лй риймъ ойрерйн щм отм 1,600 о"в/йен сйгп аморимй дййъд омеед бсйлеп роек б-26% мтеоъ сйлеп роек б-16% тбеш ойрерйн щм тг 1,200 о"в/йен. ма геез тм дщфтеъ щмймйеъ зоешеъ дчщешеъ бриймъ сйгп, аемн геез тм тмййд бщйтеш дочшйн щм дйфшчмцойд. дзечшйн ослойн лй чййоеъ тгейеъ обессеъ дъеолеъ бдщфтд дойийбд щм ъесфй сйгп мдфзъъ дсйлеп мдйщреъ агреод чемешчимйъ, аемн ск дтгейеъ айрп зг ощотйеъ еайлеъ дтгейеъ длеммъ дйрд роелд лк щргшщйн озчшйн ресфйн тм оръ мащщ аъ дооцайн. дтшлъ отшлъ: щйоещ бъесфй сйгп бойрерйн отм 500 о"в маешк жоп роца чщеш бъзмеад еъоеъд емлп, лфй щлъеб вн боаош, айп мшаеъ бъецаеъ счйшд же домцд чмйрйъ бщмб жд.
https://www.ncbi.nlm.nih.gov/pubmed/28796047
бозчш очшд-бчшд, (2019) ащш обесс тм ръерйн оозчш ачшай обечш вгем, щртшк бсйп, рлмме 229 ощъъфйн тн абзрд згщд щм сшип, амйдн деъаод чбецъ бйчешъ щм 229 ощъъфйн мма сшип. роца лй:
- шод вбедд йеъш бгн щм ейиойп E дййъд чщешд бсйлеп оефзъ мсшип ботшлъ дтйлем.
- шоъ ейиойп E вбедд дййъд чщешд бсйлеп оефзъ мсшип баефп лммй бчшб ощъъфйн тн шоъ смрйен вбедд, ак бсйлеп оевбш мсшип бчшб ощъъфйн тн шоъ смрйен роелд.
https://www.ncbi.nlm.nih.gov/pubmed/30713028
зжшд мъзймъ дозчшйн
аеЙовд 3
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2021), детшлд ддщфтд щм ъйсеу аеовд 3 тм оггйн щм осъ, рфз еъфчег дщшйш. бсчйшд рлмме 123 озчшйн, лащш ддщфтд щм аеовд 3 рбгчд бчшб ощъъфйн тн озмеъ щереъ лвеп сшип ае COPD, ае бчшб ощъъфйн бшйайн мазш айоеп вефрй отййу. бдъбсс тм 66 озчшйн щрлмме боид-армйжд, роца лй мъйсеу аеовд 3 дйд йъшеп мщйфеш осъ двеу дшжд, осъ щшйшй дщмг езежч дщшйш. дзечшйн ослойн, лй ооцай дозчш оцбйтйн тм лк щмъесфй аеовд 3 тщейд мдйеъ ъшеод мщйфеш осъ езежч дщшйш, аемн йщ мбзеп бозчшйн вгемйн йеъш дан тщейд мдйеъ млк ъшеод морйтъ сшчефрйд(1).
https://pubmed.ncbi.nlm.nih.gov/34857251/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2021) детшлд ддщфтд щм ъесфй аеовд 3 бчшб земй сшип. дзечшйн оцййрйн, лй ъесфй аеовд 3 тщеййн мъшен мийфем бъъ-ъжерд бчшб земй сшип, оцб доафййп л-70% одоиефмйн. брйъез дрелзй рбгчд ддщфтд тм оцб дщшйш, айлеъ дзййн, ощчм ештймеъ дчщешд бийфем ревг дсшип. бсчйшд рлмме шч ощъъфйн отм вйм 18 еозчшйн бдн рйъп аеовд 3 бриймд феойъ бойреп щм 600 вшн мйен мфзеъ мощк щмещд щбетеъ еотмд. бсчйшд рлмме 31 озчшйн бдн оиефмйн тн севй сшип щерйн дроцайн бшоеъ щереъ щм ъъ-ъжерд. ощк ддътшбеъ рт бйп 28 йен м-25 щбетеъ, еойреп аеовд 3 рт бйп 0.6 м-3.96 вшн/йен, лащш ойреп д-EPA дйд мфзеъ щрй вшн/йен б-12 озчшйн ефзеъ олк б-16 озчшйн. дзечшйн оцййрйн, лй шеб дозчшйн девгше бсйлеп вбед ае ма бшеш мдийд. боид-армйжд щлммд 26 одозчшйн ма роцад ъшеод мриймд щм ъесфй аеовд 3 бдъййзс моцб дщшйш, айлеъ дзййн ае дощчм. йзг тн жаъ, роца лй риймъ аеовд 3 дййъд омеед бсйлеп роек б-80% мдъфъзеъ рейшефъйд дйчфйъ лъецад оийфемй длйоеъшфйд. дзечшйн ослойн лй йщ мащщ аъ дооцайн бозчшйн ресфйн байлеъ оъегемевйъ иебд ебчбецъ оиефмйн деоеврйъ йеъш.
https://pubmed.ncbi.nlm.nih.gov/34130028/
бсчйшд щйиъйъ щм озчшйн ачшаййн обечшйн (2022), детшлд ддщфтд щм ъйсеу аеовд 3 тм осъ двеу дшжд ебрййъ щшйш, боцбйн щм дтгш фтймеъ вефрйъ. дзечшйн осбйшйн, лй ддщфтд щм аеовд 3 рзчшд бтйчш бчшб ощъъфйн фтймйн вефрйъ, ак айп осфйч тгейеъ мвбй ддщфтд бчшб ощъъфйн тн аешз зййн йещбрй ае ощъъфйн доцеййн боцб жорй щм зесш йлемъ ъретъйъ. бсчйшд рлмме щбтд озчшйн бдн 192 ощъъфйн. бзойщд оъек щйщд озчшйн бдн рбгчд ддщфтд тм дщшйш роца лй ъйсеу аеовд 3 ъшн мдтмаъ рфз еосъ щшйшй дщмг, ебщрй озчшйн роца йъшеп маеовд 3 бдчщш моггйн щм сйръжъ дзмбеп бщшйш. тн жаъ, бщрй озчшйн ма роцад дщфтд маеовд 3 тм дбйией дврий бщшйшй дщмг. ооцай дсчйшд оцбйтйн тм йъшеп мъйсеу аеовд 3 мщйфеш осъ дщшйш вн бдтгш фтймеъ вефрйъ.
https://pubmed.ncbi.nlm.nih.gov/35112608/
боид-армйжд щм озчшйн ъцфйъййн (2022) рбгч дчщш бйп цшйлъ аеовд 3 еаеовд 6 бъжерд ебйп сшчефрйд. дзечшйн оцййрйн лй боид-армйжд чегоъ щм озчшйн ачшаййн обечшйн роца лй ъесфй аеовд 3 ъшое мщйфеш осъ езежч дщшйш бчшб чщйщйн, ебоегмйн щм зйеъ отбгд дегвод ддщфтд дойийбд щм аеовд 3 тм вешойн бйемевййн дчщешйн бсшчефрйд. бсчйшд рлмме щйщд озчшйн бдн детшлд дцшйлд дъжеръйъ щм аеовд 3 еаеовд 6 бчшб ощъъфйн тн ебмй сшчефрйд. роца, лй дсйлей мсбем осшчефрйд дйд роек б-59% бчшб ощъъфйн тн цшйлд вбедд щм аеовд 3 мтеоъ роелд. тег роца лй бчшб ощъъфйн тн сшчефрйд шоъ дцшйлд щм аеовд 3 дййъд роелд йеъш баефп оебдч бдщееад мощъъфйн мма сшчефрйд. баефп лммй ма роца чщш бйп дсйлей мсбем осшчефрйд еаеовд 6, аемн бчшб ощъъфйн тн сшчефрйд шоъ даеовд 6 дййъд оти роелд йеъш мтеоъ ощъъфйн мма сшчефрйд. дзечшйн ослойн лй ъецаеъ дозчш оцбйтеъ тм чщш дфек бйп аеовд 3 есшчефрйд, ак айп осфйч тгейеъ тм оръ мдсйч мвбй дчщш тн аеовд 6.
https://pubmed.ncbi.nlm.nih.gov/35096921/
бозчш ачшай обечш (2021) детшлд дъшеод щм оъп ъесфй аеовд 3 мщйфеш ъсойрй тййфеъ бчшб озмйойн осшип. дзечшйн оцййрйн лй дтгейеъ мвбй дчщш бйп ъесфй щоп гвйн еъсойрй тййфеъ айрп тчбйеъ ема бшеш одн двешойн мдбгмйн бъецаеъ бйп дозчшйн. бозчш жд рбгчд ддщфтд щм доцб дъжеръй дбсйсй щм дощъъфйн тм ъецаеъ ддътшбеъ. бозчш рлмме 85 рщйн, 4-36 зегщйн мазш сйен дийфем бсшип дщг дсебмеъ оъсойрй тййфеъ бшод бйрерйъ тг вбедд. дощъъфеъ земче ачшайъ мчбмъ ойреп йеой щм 6 вшн щоп гвйн, 6 вшн щоп сейд ае 3 вшн олм азг мощк щйщд щбетеъ. млм дощъъфеъ детшк доцб дъжеръй дбсйсй бъзймъ ддътшбеъ, лащш 69% одп дйе боцб ъжеръй иеб е-31% сбме озсш ъжеръй чм тг бйрерй. роца лй рщйн боцб ъжеръй иеб дйе бтмеъ шоъ аеовд 3 вбедд йеъш бъзймъ ддътшбеъ, аемн йзс аеовд 6 маеовд 3 дйд бмъй ъмей боцб дъжеръй дбсйсй. бчшб рщйн боцб ъжеръй иеб дтмййд бшоъ аеовд 3 бгн бтчбеъ ддътшбеъ дййъд вбедд йеъш, мма дщфтд тм дщйрей бшоъ аеовд 6 бгн. дзечшйн отшйлйн лй бчшб озмйоеъ боцб ъжеръй иеб риймъ 3 вшн мйен щоп гвйн мощк щйщд щбетеъ ъебйм мтмййд щм 0.36 о"в/о"м бшоъ аеовд 3 бгн, мтеоъ тмййд щм 0.21 о"в/о"м бчшб рщйн тн зсш ъжеръй. блм дчбецеъ рцфд щйфеш бъсойрй дтййфеъ, мма дбгм бйп дчбецеъ ебаефп бмъй ъмей боцб дъжеръй дбсйсй. тн жаъ, бчшб дрщйн щриме щоп гвйн, тмййд вгемд йеъш бшоъ аеовд 3 бгн дййъд омеед бщйфеш вгем йеъш бъсойрй дтййфеъ. осчръ дзечшйн дйа лй оцб ъжеръй иеб тщей мъшен мщйфеш дсфйвд щм аеовд 3 еблк мдебйм мщйфеш вгем йеъш бъсойрй дтййфеъ. дозчш оеоп тм йгй д-NIH едзбшд даошйчайъ мсшип едзечшйн огеезйн тм дтгш рйвегй айришсйн.
https://pubmed.ncbi.nlm.nih.gov/35011059/
бозчш лфем-сойеъ обечш фмсбе (2021) рбгчд ддщфтд щм ъесу аеовд 3 бчшб рщйн обевшеъ добцтеъ айоерй дървгеъ. дзечшйн оцййрйн, лй йщрп тгейеъ доцбйтеъ тм йъшеп мрщйн бдщфтд дарбемйъ щм аеовд 3, емлп мъйсеу аеовд 3 тщейд мдйеъ ъетмъ бчшб рщйн обевшеъ ащш оаефййреъ бъвебъ щшйш роелд майоерй дървгеъ. бозчш рлмме 16 рщйн бшйаеъ бреъ 64 бооецт, ащш земче ачшайъ мриймъ 3,680 о"в/йен аеовд 3 ае фмсбе мощк щйщд щбетеъ, бресу мдщъъфеъ бълрйъ айоерй дървгеъ щмещ фтойн бщбет. роца лй айоерй ддървгеъ ъшое мщйфеш зежч дщшйш бщъй дчбецеъ, тн йъшеп маеовд 3 бдчщш мтмййд босъ дщшйш. ма роца йъшеп оебдч маеовд 3 бдъййзс мсйръжъ дзмбеп бщшйш, аемн бщбетййн дазшерйн мдътшбеъ жедъд овод мфйд чцб дсйръжд дйд вбед йеъш бчбецъ даеовд 3 бдщееад мфмсбе. дзечшйн ослойн лй риймъ ъесу аеовд 3 ъшод мдтмаъ осъ дщшйш бтчбеъ айоерй дървгеъ, тн ъфчйг афщшй мсйръжъ дзмбеп бщшйш (2).
https://pubmed.ncbi.nlm.nih.gov/34857226/
бщръ 2010 дзм башд"б озчш лфем-сойеъ обечш фмсбе, щоишъе дтйчшйъ дййъд мдтшйк дан риймъ ъесфй аеовд 3 еейиойп D бойреп вбед мъчефд ооещлъ, тщейд мдйеъ йтймд мдфзъъ дсйлеп мдъфъзеъ сшип еъзмеад чшгйеесчемшйъ. дозчш ртшк тм йгй цееъ зечшйн одшееашг, елмм 25,871 ощъъфйн: 13,085 рщйн отм вйм 55 е-12,786 вбшйн отм вйм 50, ошзбй ашд"б, мма дйсиешйд щм сшип ае ъзмеад чшгйеесчемшйъ. дощъъфйн земче ачшайъ м-4 чбецеъ:
ъчефъ ддътшбеъ дзмд бйп ребобш 2011 мошх 2014, едсъййод бсеу 2017, лащш ощк ддътшбеъ дооецт дйд 5.3 щрйн. ъецаеъ дозчш дошлжйеъ децве бщръ 2018, блрс щм айвег дмб даошйчай (AHA) ебщрй оаошйн блъб дтъ New England Journal of Medicine. отбш млк, оаж етг дйен офешсойн оаошйн шбйн дтесчйн бдйбийн ресфйн щм ъецаеъ дозчш, вн бдъййзс мдщАфтъ ддътшбеъ тм ъецаеъ ресфеъ, лвеп селшъ, озмеъ тйрййн, жйлшеп еъфчег чеврйийбй, озмъ лмйеъ етег. мдмп фйшеи дооцайн дтйчшййн(1):
ейиойп Dй (2)
-
сшип: ма роца дбгм оебдч сиийсийъ бйп дощъъфйн щчйбме ейиойп D, мбйп дощъъфйн щчйбме фмсбе бщйтеш очшй дсшип баефп лммй (793 мтеоъ 824 очшйн, бдъаод), елп бщйтеш дочшйн щм сшип щг, тшоерйъ ае чемешчимй. тн жаъ, роцад ъойлд млк щриймъ ейиойп D мъчефд ооещлъ, тщейд мъшен мйшйгд щм л-25% бсйлеп мъоеъд осшип.
-
ъзмеад чшгйеесчемшйъ: ма роца дбгм оебдч сиийсийъ бйп дощъъфйн щчйбме ейиойп D, мбйп дощъъфйн щчйбме фмсбе бщйтеш дайшетйн дчшгйеесчемшййн баефп лммй (396 мтеоъ 409 айшетйн, бдъаод) ае бдъййзс мщйтеш дочшйн щм аеин щшйш дмб, щбх, ъоеъд овешойн чшгйеесчемшййн ае ъоеъд олм вешн.
-
дщфтеъ щмймйеъ: роцае дщфтеъ щмймйеъ оетиеъ мриймъ ейиойп D бойреп вбед, мма тмййд оебдчъ бсйлеп мдйфшчмцойд, абрйн блмйеъ ае ъсойрйн ботшлъ дтйлем.
дзечшйн ослойн, лй ъецаеъ дозчш айрп ъеолеъ бриймъ ейиойп D бойреп вбед морйтъ сшип ае ъзмеад чшгйеесчемшйъ бчшб обевшйн бшйайн ащш цешлйн ейиойп D бойреп дргшщ мщойшд тм бшйаеъ дтцн.
аеЙовд 3 (3)
-
ъзмеад чшгйеесчемшйъ: роцад йшйгд щм 8%, щайрд оебдчъ сиийсийъ, бщйтеш дайшетйн дчшгйеесчемшййн бчшб дощъъфйн щчйбме щоп гвйн бдщееад мфмсбе (386 мтеоъ 419 айшетйн, бдъаод). ъецад жаъ рбтд ойшйгд байшетйн щм аеин щшйш дмб, мма дбгм ощотеъй байшетй щбх. баефп сфцйфй, риймъ щоп гвйн дфзйъд аъ дсйлеп маеин щшйш дмб б-28%, еаъ дсйлеп мъоеъд лъецад оаеин щшйш дмб б-50%, мма дщфтд тм дсйлеп мщбх ае мъоеъд чшгйеесчемшйъ овешойн щайрн аеин щшйш дмб. тег роца лй риймъ аеовд 3 дййъд омеед бйшйгд щм 22% бцръешйн (ъдмйлй арвйефмсийд).
-
сшип: ма роца дбгм оебдч сиийсийъ, бйп дощъъфйн щчйбме щоп гвйн мбйп дощъъфйн щчйбме фмсбе бщйтеш очшй дсшип баефп лммй (820 мтеоъ 797 очшйн, бдъаод), елп бщйтеш дочшйн щм сшип щг, сшип тшоерйъ, сшип чемешчимй, ъоеъд осшип ае ъоеъд олм вешн.
-
дщфтеъ щмймйеъ: риймъ ъесу щоп гвйн рсбмд дйиб, мма тмййд бсйлеп мгйоен ае мъсойрйн ботшлъ дтйлем.
-
рйъез мфй ъъй-чбецеъ: дщфтд ойийбд, роцад бчшб ощъъфйн щгйеезе бъзймъ дозчш тм цшйлд роелд щм гвйн (тг 1.5 ореъ мщбет), тн йшйгд щм 19% бсйлеп майшетйн чшгйеесчемшййн ещм 40% бсйлеп маеин щшйш дмб, мма йъшеп оебдч мдътшбеъ бчшб ощъъфйн тн цшйлъ гвйн вбедд (отм 1.5 ореъ мщбет).
-
бресу, роцад дщфтд ойийбд мриймъ ъесу щоп гвйн, бчшб ощъъфйн ооеца афше-аошйчай, баефп бмъй ъмей бцшйлъ дгвйн.
мсйлен, ъецаеъ дозчш дтйчшйеъ ошаеъ лй риймъ ейиойп D ма ъшод мдфзъъ дсйлеп мсшип ае мъзмеад чшгйеесчемшйъ, аемн тщейд мъшен мдфзъъ дсйлеп мъоеъд осшип. риймъ аеовд 3 ма ъшод мдфзъъ дсйлеп мсшип ае мъзмеад чшгйеесчемшйъ баелмесййд длммйъ, аемн дййъд омеед бдфзъъ дсйлеп маеин щшйш дмб, елп мдфзъъ дсйлеп дчшгйеесчемшй бчшб ощъъфйн тн цшйлъ гвйн роелд.
ъецаеъ ресфеъ:
-
блрс щм айвег дмб даошйчай (AHA), щртшк бребобш 2020, децве ъецаеъ шащерйеъ орйъез ресу (VITAL-Rhythm) бе рбгчд дйтймеъ щм ейиойп D еаеовд 3 морйтъ фшфеш фшежгешйн (AF). бозчш жд, ма роцад ъойлд мщйоещ бъесфй ейиойп D ае аеовд 3 морйтъ фшфеш фшежгешйн, лащш ййълп ериймъ аеовд 3 тмемд ау мдвбйш аъ дсйлеп. йзг тн жаъ, овод жаъ ма дййъд оебдчъ сиийсийъ, еогебш бъецаеъ шащерйеъ бмбг щишн фешсое еишн тбше бйчешъ тойъйн(4).
-
брйъез ощрй щм дръерйн, рбгчд дйтймеъ щм ейиойп D мдфзъъ дсйлеп мсшип оъчгн, лъмеъ б-BMI. бъчефъ ддътшбеъ жеде 1,617 очшйн щм сшип фемщрй, лащш бчшб ощъъфйн щчйбме ейиойп D, роца сйлеп роек б-17% мсшип фемщрй бдщееад мфмсбе (щйтеш очшйн щм 1.7% мтеоъ 2.1%). дйшйгд бсйлеп дййъд оебдчъ шч бчшб дощъъфйн тн BMI биеез дрешод, ак ма бчшб ощъъфйн тн BMI отм 25 (сйлеп роек б-38% мтеоъ сйлеп роек б-11% бчшб ощъъфйн тн BMI биеез 25-30 есйлеп вбед б-5% бчшб ощъъфйн тн BMI отм 30)(5).
- http://www.vitalstudy.org/findings.html
- https://pubmed.ncbi.nlm.nih.gov/30415629/
- https://pubmed.ncbi.nlm.nih.gov/30415637/
- https://professional.heart.org/es/meetings/scientific-sessions
- https://pubmed.ncbi.nlm.nih.gov/33206192/
бозчш ачшай обечш (йреаш 2017) рбгчд дйтймеъ щм ъесу ъжерд оетщш баеовд 3 мдфзъъ ддщфтеъ щмймйеъ щм ийфем лйоеъшфй.
бозчш рлмме 61 земй сшип дещи, дтебшйн лйоеъшфйд чгн-рйъезйъ (рйае-агв'ебрийъ), длеммъ щймеб щм гесичсм, цйсфмаийп е-5- фмеаешеаешцйм. дрзчшйн земче баефп ачшай мчбмъ ъесу аеовд 3 бойреп вбед (900 о"в зеоцд амфа-мйремрйъ мйен) ае бойреп роек (250 о"в зеоцд амфа-мйремрйъ мйен) бджрд аришмйъ мощк 15 йен (3 йойн мфрй длйоеъшфйд ебочбйм м-12 йой дийфем). ооцай дозчш ошайн лй ма дйд дбгм бйп дчбецеъ бйзс мщйтешй дрейишефрйд ае дмейчефрйд. тн жаъ, роца лй бдщееад мриймъ аеовд 3 бойреп роек, риймъ аеовд 3 бойреп вбед дййъд омеед бщлйзеъ роелд йеъш баефп оебдч щм гмчъ шйшйеъ дфд (сиеоийийс) (p=0.018), бщйтеш роек йеъш, щайрре оебдч сиийсийъ, щм оиефмйн дсебмйн ощмщемйн зоешйн (16.1% мтеоъ 36.7%, p=0.068) елп бщйтеш роек йеъш еоебдч щм оиефмйн дсебмйн одфштеъ бъфчегй длбг (тмййд баржйойн AST е-ALT, p=0.012 е-p=0.015, бдъаод). ооцай дозчш оцбйтйн тм дйтймеъ щм аеовд 3 бойреп вбед мдврд тм дшйшйеъ етм фтймеъ длбг бодмк ийфемй лйоеъшфйд.
https://www.ncbi.nlm.nih.gov/pubmed/27644137
бсчйшд щйиъйъ еоид-армйжд (афшйм 2017) рбгчд ддщфтд щм ъесфй аеовд 3 бчшб земй сшип, дтебшйн рйъез мдсшъ вйгем ботшлъ дтйлем.дзечшйн осбйшйн лй земйн амд роцайн бсйлеп мсйбелйн щерйн мазш дрйъез - лвеп ъъ-ъжерд, гйлей зйсерй, сишс етмййд бъдмйлйн гмчъййн - еаеовд 3 тщейд мдйеъ бтмъ дщфтд ойийбд. бсчйшд рлмме ъщтд озчшйн ачшаййн обечшйн, бдн 623 земйн, лащш щйщд одозчшйн ртшле бсйп. роца лй бчшб земйн щриме ъесу аеовд 3 (бойрерйн дощърйн оозчш мозчш), бдщееад мчбецъ бйчешъ тн ъжерд бтмъ тшк чмешй ждд, роца щйфеш оебдч бфтймеъ дзйсерйъ, тн шод роелд йеъш щм CRP е- IL-6 ешоеъ вбедеъ йеъш щм амбеойп еъай T осев CD3 е-CD4. тн жаъ, ма роца дбгм бйп дчбецеъ бшоъ TNF-α ериймъ аеовд 3 дййъд омеед бйшйгд бъай T осев CD8 . дзечшйн ослойн лй риймъ ъесу аеовд 3 5-7 йойн мфрй дрйъез емаешк ъдмйк ддзмод ъшод мдфзъъ дъвебд дгмчъйъ емщйфеш дфтймеъ дзйсерйъ еблк тщейд мдйеъ бтмъ дщфтд ойийбд мземй сшип мазш рйъез ботшлъ дтйлем. дтшъ дотшлъ: мцг осчреъ озчш жд, гйеезйн чегойн отйгйн тм дцешк брчйиъ ждйшеъ бриймъ зеоцеъ щеоп осев аеовд 3 осфш йойн мфрй рйъез, бщм тмйд бсйлеп мгйоен. мцтшйре, айп ажлеш млк боаош лмм.
https://www.ncbi.nlm.nih.gov/pubmed/28410575
бдъбсс тм ръерйн ощрй озчшй течбд вгемйн (йемй 2016), зечшйн бзре аъ дчщш бйп цшйлъ зеоцеъ щеоп осев аеовд 3 щочешп бгвйн мбйп щйтеш дъоеъд бчшб 1,659 ощъъфйн тн сшип чемешчимй.роца лй цшйлд вбедд йеъш щм аеовд 3 мазш абзеп дозмд дййъд чщешд бсйлеп роек йеъш мъоеъд осшип чемешчимй, лащш амд щцшле мфзеъ 0.3 вшн мйен аеовд 3 дйе бсйлеп роек бл-40% мъоеъд, бдщееад моиефмйн щцшле тг 0.1 вшн мйен аеовд 3. бресу, земйн ащш мазш дабзрд дтме аъ цшйлъ даеовд 3 бмфзеъ 0.15 вшн мйен дйе бтмй сйлеп роек бл-70% мъоеъд бдщееад мземйн щма щйре аъ цшйлъ аеовд 3. ма роца чщш бйп цшйлъ аеовд 3 мазш дабзрд мбйп дсйлеп мъоеъд олм вешн. дзечшйн ослойн лй дтмаъ дцшйлд щм аеовд 3 бземйн тн сшип чемешчимй тщейд мщфш аъ сйлейй ддйщшгеъ щмдн.
http://www.ncbi.nlm.nih.gov/pubmed/27436272
счйшд (2016) дтесчъ бфтймеъ дарий-сширйъ щм шлйбйн ъжеръййн щерйн, бгвщ тм ъшеоън мийфем бсшип дщг. дсчйшд леммъ фйшеи мвбй зеоцъ щеоп аеовд 3 доефчъ огвйн, шжшбишем доцей бтрбйн е-EGCG доцей бъд йшеч елп оефч одцоз Ziziphus jujube. босвшъ дсчйшд оцйвйн дзечшйн аъ орврерй дфтемд доемчемшййн бдн шлйбйн амд отлбйн ъдмйлйн сширййн, бйрйдн ейсеъ дфтймеъ щм аржйойн ревгй зоцеп ейцйшъ дщфтд арий-фшемйфшийбйъ (тйлеб щвщев ъайн сширййн) еафефиеийъ (тйгег оееъ ъайн сширййн). дзечшйн чешайн мчйен озчшйн ресфйн мдтшлъ дщйоещ дчмйрй бшлйбйн амд лзмч одийфем бсшип дщг.
https://www.ncbi.nlm.nih.gov/pubmed/26156544
бозчш отбгд (йерй 2017), добесс тм гвйоеъ щрасфе очбецъ земй сшип чемешчимй, рбгч мшащерд дчщш бйп сйлейй ддйщшгеъ мбйп дбйией щм аржйойн дотешбйн боибемйжн щм зеоцеъ щеоп осев аеовд 3 (CYP4F11) еаеовд 6 (CYP4A11). роца лй земйн тн шод вбедд йеъш щм аржйойн дчщешйн боибемйжн щм аеовд 6 дйе бтмй сйлейй дйщшгеъ роелйн йеъш бдщееад мземйн тн шод вбедд йеъш щм аржйойн дчщешйн боибемйжн щм аеовд 3. дзечшйн осбйшйн лй доибемйийн дрецшйн офйшеч аеовд 3 ъешойн морйтъ дъфщиеъ двйгем емлп ллм щшоъ даржйойн дотешбйн боибемйжн щм аеовд 3 вбедд йеъш, лк йщрд тмййд боибемйийн амд. мтеоъ жаъ, доибемйийн щм аеовд 6 чщешйн бцойзъ двйгем ебдъчгоеъ дозмд. ооцай дозчш тщеййн мъшен мфйъез ъшефеъ згщрйеъ дойетгеъ мфтемд сфцйфйъ тм аржйойн амд.
https://www.ncbi.nlm.nih.gov/pubmed/28557975
бсчйшд щйиъйъ еоид-армйжд (2018) рбгчд ддщфтд щм риймъ ъесфй аеовд 3, баоцтеъ джрд ъек-ешйгйъ, тм дфтймеъ дзйсерйъ едъецаеъ дчмйрйеъ бчшб оиефмйн тн сшип ботшлъ дтйлем мазш рйъез. бсчйшд рлмме щбтд озчшйн ачшаййн обечшйн, бдн 457 земй сшип ботшлъ дтйлем - лемм сшип чемешчимй, сшип чйбд есшип отй. бозчшйн дщерйн дощъъфйн бчбецъ ддътшбеъ чйбме щймеб щм аеовд 3 еаеовд 6 бйзс щм 1:4 ае 1:3 (миебъ аеовд 6) тн ойреп щм 0.2 вшн/ч"в аеовд 3, едощъъфйн бчбецъ дбйчешъ чйбме щоп сейд ае аеовд 6 бмбг, мощк 5-7 йойн мазш дрйъез. орйъез лемм щм дръерйн темд лй земйн щриме аеовд 3 дйе бсйлеп роек б-64% мсбем осйбелйн жйдеоййн еощк ащфежн дйд чцш б-2.3 йойн бооецт. тег роца лй бчшб земйн щриме аеовд 3 зм щйфеш бфтймеъ дзйсерйъ щм ъай дгн дмбрйн. дзечшйн ослойн лй ооцайн амд осфчйн ъойлд мйтймеъ щм ъесу аеовд 3 мазш рйъез бчшб земй сшип дотшлъ дтйлем, аемн ргшщйн озчшйн бдйчу вгем йеъш тм оръ мащщ аъ дооцайн.
https://www.ncbi.nlm.nih.gov/pubmed/29222889
бозчш лфем-сойеъ обечш фмсбе (гцобш 2017), щртшк байшап, детшлд дйтймеъ щм аеовд 3 мийфем боечежйийс (лйбйн егмчъ бзмм дфд), дрвшн лъецад оийфемй лйоеъшфйд. бозчш рлмме 60 оиефмйн, ащш земче ачшайъ мриймъ ъесу аеовд 3 (бойреп йеой щм 360 о"в EPA е-240 о"в DHA) ае фмсбе, мощк 3 щбетеъ бочбйм мийфемй длйоеъшфйд. роца лй бщбетййн дшащерйн зеошъ доечежйийс дййъд роелд йеъш бчбецъ даеовд 3, лащш мазш 3 щбетеъ ма дййъд тгеъ моечежйийс бчшб 100% одощъъфйн бчбецъ даеовд 3 мтеоъ 33% бчбецъ дфмсбе. ощк джоп бе дощъъфйн сбме ооечежйийс рт бйп 4 м-9 йойн бчбецъ даеовд 3, мтеоъ мфзеъ 10 йойн бчбецъ дфмсбе. дзечшйн ослойн лй риймъ ъесу аеовд 3 дййъд омеед бшод фзеъд щм лаб езесш резеъ бзмм дфд едвшеп, елп бщйфеш айлеъ дзййн, йлемъ далймд едщъййд еайлеъ дщйрд.
https://www.ncbi.nlm.nih.gov/pubmed/29324423
бозчш, щртшк бчшб тлбшйн (гцобш 2017), роца лй аеовд 3 щочешд бщоп гвйн дййъд йтймд йеъш баефп рйлш оаеовд 3 оочеш цозй морйтъ вйгемйн сширййн ббмеиеъ дзмб.
https://www.ncbi.nlm.nih.gov/pubmed/29413488
озчш чмйрй (афшйм 2018) рбгчд ддщфтд щм ожеп шфеай долйм аеовд 3 мийфем бчлчсйд (айбег ощчм) бчшб оиефмйн тн сшип бгшлй дошд ае бмбмб дтебшйн ийфемй лйоеъшфйд. бозчш рлмме 27 оиефмйн, ащш чйбме ожеп шфеай оетщш баеовд 3 (Racol®) баоцтеъ цйрешйъ джрд. бресу, оиефмйн тн сшип мбмб чйбме ъесу аржйой тйлем (LipaCreon®) мщйфеш дсфйвд. йтймеъ дийфем детшлд баоцтеъ огйгъ осъ щшйшй дщмг ебгйчеъ гн, щрмчзе бъзймъ дозчш емазш 4 е-8 щбетеъ. одъецаеъ темд лй бчшб лм доиефмйн рцфъд тмййд оебдчъ босъ щшйшй дщмг мазш 4 е-8 щбетеъ бдщееад мръерй дбсйс. дзечшйн ослойн лй риймъ ъесу аеовд 3 тщейд мъшен мдфзъъ члчсйд бчшб земй сшип бгшлй дошд ае сшип мбмб щайре рйъп мдсшд брйъез.дтшъ отшлъ: дозчш мма чбецъ бйчешъ етм лп йщ мдъййзс мъецаеъ баефп оевбм.
https://www.ncbi.nlm.nih.gov/pubmed/29599363
зжшд мъзймъ дозчшйн
еДйиойп D
мдмп щъй оид-армйжеъ ащш безреъ аъ дчщш бйп риймъ ъесфй ейиойп D ебйп дсйлеп мъоеъд осшип. бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2022) рбгч дчщш бйп риймъ ъесфй ейиойп D ебйп ъоеъд осшип. дзечшйн осбйшйн лй зсш ейиойп D чщеш бсйлеп оевбш мсшип емъоеъд, аемн ма бшеш одй дъетмъ щм ъйсеу ейиойп D. бсчйшд рлмме 12 озчшйн бдн 72,669 ощъъфйн щайрн земй сшип. бозчшйн амд рбгчд ддщфтд щм риймъ ъесу ейиойп D тн ае бмй сйгп бойрерйн щерйн бдщееад мфмсбе ае мсйгп бмбг. ощк ддътшбеъ рт бйп 2 м-5.3 щрйн. мдмп дооцайн дтйчшййн:
- дсйлеп мъоеъд осшип детшк б-6 озчшйн бдн 61,882 ощъъфйн. брйъез лемм щм дръерйн ма роца дбгм оебдч бйп риймъ ъесфй ейиойп D ебйп чбецъ дбйчешъ. тн жаъ, риймъ ейиойп D бойреп йеой (бдщееад мойреп ъчефъй ае зг фтой) дййъд чщешд бсйлеп роек б-16% мъоеъд осшип. бресу, роца лй риймъ ейиойп D дййъд чщешд бсйлеп роек б-37% мъоеъд осшип шйаеъ.
- дсйлеп мдъфъзеъ сшип детшк б-11 озчшйн бдн 51,369 ощъъфйн. брйъез лемм щм дръерйн ма роца дбгм оебдч бйп риймъ ъесфй ейиойп D ебйп чбецъ дбйчешъ бдъййзс мсйлеп длммй мсшип ае мсевй сшип сфцйфййн (шйаеъ, щг, тшоерйъ, чемешчимй).
дзечшйн ослойн лй баефп лммй ма роцад ъойлд мъетмъ щм ъйсеу ейиойп D бдфзъъ дсйлеп мъоеъд ае мъзмеад бсшип, омбг ъетмъ афщшйъ бдфзъъ дсйлеп мъоеъд осшип шйаеъ.
боид-армйжд щм озчшйн ачшаййн обечшйн (2022) рбгч дчщш бйп риймъ ъесфй ейиойп D едсйлеп мсшип ъек бзйръ ддщфтд щм асишивййъ дъйсеу ещм дщорд.брйъез рлмме 13 озчшйн бдн рбгч дсйлеп мдъфъзеъ сшип (12 озчшйн), ъоеъд осшип (6 озчшйн) еъоеъд олм вешн (10 озчшйн). б-8 одозчшйн рйъп ейиойп D бриймд йеойъ бойреп щм 400 тг 4,000 йзб"м мйен еб-5 озчшйн рйъп ъйсеу ъчефъй бойреп щрт бйп 20,000 йзб"м мщбет м-500,000 йзб"м мщрд. ощк ддътшбеъ едотчб рт бйп 3 м-10 щрйн.
мдмп дооцайн дтйчшййн:
- ма роца чщш оебдч бйп ъйсеу ейиойп D ебйп дсйлеп мдъфъзеъ сшип, баефп бмъй ъмей басишивййъ дъйсеу (риймд йеойъ мтеоъ ъчефъйъ). тн жаъ, бозчшйн тн риймд йеойъ роца сйлеп роек б-24% мсшип бчшб ощъъфйн бощчм ъчйп ак ма бчшб ощъъфйн тн тегу ощчм ае щореъ.
- баефп лммй ма роца чщш оебдч бйп ъйсеу ейиойп D ебйп ъоеъд осшип. тн жаъ, бозчшйн бдн рйъп ейиойп D бриймд йеойъ роца сйлеп роек б-13% мъоеъд.
- риймъ ейиойп D дййъд чщешд бсйлеп роек б-5% мъоеъд олм вешн бдщееад мчбецъ дбйчешъ. бозчшйн тн риймд йеойъ роца сйлеп роек б-7%, мма чщш оебдч бозчшйн тн риймд ъчефъйъ.
дзечшйн ослойн лй риймд йеойъ, ак ма ъчефъйъ, щм ъесфй ейиойп D чщешд бдфзъъ дсйлеп мъоеъд осшип, елп чщешд бсйлеп оефзъ мдъфъзеъ сшип шч бчшб ощъъфйн бощчм ъчйп.
https://pubmed.ncbi.nlm.nih.gov/35954381/
https://pubmed.ncbi.nlm.nih.gov/35676320/
боид-армйжд щм озчшйн ъцфйъййн едътшбеъййн (2022) детшк дчщш бйп дщйоещ бъесфй ейиойп D мазш абзръ сшип ебйп дйщшгеъ. дзечшйн оцййрйн лй риймъ ейиойп D мфрй дабзрд роцад чщешд бсйлеп оефзъ мъоеъд, лащш тгейеъ тглрйеъ оцбйтеъ тм ъетмъ афщшйъ вн мриймъ ейиойп D мазш дабзрд. брйъез рлмме дръерйн о-11 озчшйн, одн 6 озчшй течбд е-5 озчшйн ачшаййн обечшйн. бозчшйн амд рбгч дчщш бдъййзс мдйщшгеъ баефп лммй (9 озчшйн), мдйщшгеъ мма дзошд (8 озчшйн), мдйщшгеъ сфцйфйъ мсшип (3 озчшйн) емдйщреъ дозмд (3 озчшйн). брйъез лемм щм дръерйн ощрй севй дозчшйн роца лй бдщееад мощъъфйн щма риме ейиойп D мазш дабзрд, риймъ ъесфй ейиойп D дййъд чщешд бсйлеп роек б-13% мъоеъд баефп лммй. дъецаеъ бдъййзс моггй ддйщшгеъ еддйщреъ дресфйн ма дйе оебдчйн сиийсийъ. тн жаъ, брйъез мфй ъъй-чбецеъ роца лй ъецаеъ амд дйе оебдчеъ шч бозчшй дтечбд. дзечшйн ослойн лй риймъ ъесфй ейиойп D чщешд бощк дйщшгеъ ашек йеъш бчшб земй сшип, аемн йщ мащщ аъ дооцайн щлп ма роцад ъойлд мчщш сйбъй бозчшйн ачшаййн обечшйн.
https://pubmed.ncbi.nlm.nih.gov/36014928/
бсчйшд щйиъйъ еоид-армйжд (2023) щм озчшйн ачшаййн обечшйн детшлд ддщфтд щм ъесфй ейиойп D тм оггй гмчъ бчшб оиефмйн тн сшип ае тн рвтйн ишен-сширййн. дзечшйн оцйтйн лй мейиойп D феирцйам мгйлей вйгемйн баоцтеъ дщфтд тм ъдмйлй гмчъ. бсчйшд рлмме 8 озчшйн бдн 592 ощъъфйн, лемм земеъ сшип щг (4 озчшйн), рщйн тн вйгемйн ишен-сширййн бцееаш дшзн (2 озчшйн) еоиефмйн тн вйгемйн сширййн ае щфйшйн ботй двс (2 озчшйн). б-5 одозчшйн рйъре ъесфй ейиойп D фтн бщбет ае фтн бщбетййн бойреп 50,000 йзб"м, ебозчшйн дазшйн рйъп ойреп йеой щм тг 4,000 йзб"м. ощк ддътшбеъ рт бйп 8 м-24 щбетеъ. брйъез лемм щм дръерйн роца лй риймъ ъесфй ейиойп D дййъд омеед бйшйгд оебдчъ богг дгмчъ TNF-α. бресу, жедъд овоъ йшйгд щайрд оебдчъ сиийсийъ боггй дгмчъ IL-6 е-CRP. ма роцад дщфтд тм шоъ IL-10. дзечшйн ослойн лй роцад ъойлд мдщфтд ревгъ дгмчъ щм ейиойп D, едн оцйтйн лй тщейд мдйеъ ъетмъ мриймд оеъаоъ айщйъ щм ейиойп D мгйлей дъвебд дгмчъйъ бчшб оиефмйн тн сшип ае рвтйн ишен-сширййн.
https://pubmed.ncbi.nlm.nih.gov/37244755/
бсчйшд щйиъйъ еоид-армйжд щм озчшйн ачшаййн обечшйн (2019) рбгч дчщш бйп риймъ ъесфй ейиойп D мбйп дсйлеп мъоеъд. бсчйшд рлмме 52 озчшйн, бдн 75,454 ощъъфйн, ащш бгче аъ ддщфтд щм ъесфй ейиойп D бдщееад мфмсбе ае мдтгш ийфем. сд"л ъетге 8,033 очшй ъоеъд, оъелн 1,331 очшйн щм ъоеъд оозмеъ чшгйеесчемшйеъ е-877 осшип. брйъез лемм щм дръерйн ма роца чщш бйп риймъ ъесфй ейиойп D мбйп дсйлеп мъоеъд. тн жаъ, риймъ ъесфй ейиойп D дййъд омеед бсйлеп роек б-16% мъоеъд осшип. брйъез мфй ъъй-чбецеъ ма роцад дщфтд оебдчъ мощърйн лое шоъ дбсйс щм ейиойп D ае дойреп, аемн роца йъшеп осейн мъесу ейиойп D3 тм фрй ейиойп D2.
https://pubmed.ncbi.nlm.nih.gov/31405892/
боид-армйжд щм озчшйн ачшаййн обечшйн (2019) детшлд ддщфтд щм риймъ ъесфй ейиойп D тм дсйлеп мъзмеад емъоеъд осшип. дзечшйн осбйшйн лй боид-армйжеъ чегоеъ роцае ъецаеъ сеъшеъ, ебшеб дозчшйн рйъре ойрерйн роелйн йзсйъ (тг 1,100 йзб"м/йен). брйъез дрелзй рлмме вн озчшйн тглрййн, бдн ртщд щйоещ бойрерйн вбедйн йеъш. бдъййзс мщйтеш дъзмеад бсшип: брйъез рлмме тщшд озчшйн, лащш бъчефъ отчб щм 3-10 щрйн аебзре 6,537 земйн. бчбецъ ддътшбеъ дещвд шоъ ейиойп D бгн щм 54-135 рреоем/мйиш, аемн ма роцае дбгмйн оебдчйн бйп дчбецеъ. лмеош, ма роцад дщфтд мриймъ ъесфй ейиойп D тм дсйлеп мсшип. бдъййзс мщйтеш дъоеъд осшип: брйъез рлмме зойщд озчшйн, лащш бъчефъ отчб щм 3-10 щрйн ъетге 1,591 очшй ъоеъд. роца лй риймъ ъесфй ейиойп D дййъд чщешд бсйлеп роек б-13% мъоеъд осшип. дзечшйн оцййрйн лй рйъп мййзс ооца жд бтйчш мозчшйн бдн рйъп ойреп йеой, брйвег мозчшйн бдн рйъп ойреп вбед оаег баефп ъчефъй (бемес). дзечшйн ослойн лй риймъ ъесфй ейиойп D дййъд омеед бйшйгд оебдчъ бщйтеш дъоеъд осшип, ак мма дщфтд тм щйтеш дъзмеад.
https://www.ncbi.nlm.nih.gov/pubmed/30796437
бщръ 2010 дзм башд"б озчш лфем-сойеъ обечш фмсбе, щоишъе дтйчшйъ дййъд мдтшйк дан риймъ ъесфй аеовд 3 еейиойп D бойреп вбед мъчефд ооещлъ, тщейд мдйеъ йтймд мдфзъъ дсйлеп мдъфъзеъ сшип еъзмеад чшгйеесчемшйъ. дозчш ртшк тм йгй цееъ зечшйн одшееашг, елмм 25,871 ощъъфйн: 13,085 рщйн отм вйм 55 е-12,786 вбшйн отм вйм 50, ошзбй ашд"б, мма дйсиешйд щм сшип ае ъзмеад чшгйеесчемшйъ. дощъъфйн земче ачшайъ м-4 чбецеъ:
ъчефъ ддътшбеъ дзмд бйп ребобш 2011 мошх 2014, едсъййод бсеу 2017, лащш ощк ддътшбеъ дооецт дйд 5.3 щрйн. ъецаеъ дозчш дошлжйеъ децве бщръ 2018, блрс щм айвег дмб даошйчай (AHA) ебщрй оаошйн блъб дтъ New England Journal of Medicine. отбш млк, оаж етг дйен офешсойн оаошйн шбйн дтесчйн бдйбийн ресфйн щм ъецаеъ дозчш, вн бдъййзс мдщАфтъ ддътшбеъ тм ъецаеъ ресфеъ, лвеп селшъ, озмеъ тйрййн, жйлшеп еъфчег чеврйийбй, озмъ лмйеъ етег. мдмп фйшеи дооцайн дтйчшййн(1):
ейиойп Dй (2)
-
сшип: ма роца дбгм оебдч сиийсийъ бйп дощъъфйн щчйбме ейиойп D, мбйп дощъъфйн щчйбме фмсбе бщйтеш очшй дсшип баефп лммй (793 мтеоъ 824 очшйн, бдъаод), елп бщйтеш дочшйн щм сшип щг, тшоерйъ ае чемешчимй. тн жаъ, роцад ъойлд млк щриймъ ейиойп D мъчефд ооещлъ, тщейд мъшен мйшйгд щм л-25% бсйлеп мъоеъд осшип.
-
ъзмеад чшгйеесчемшйъ: ма роца дбгм оебдч сиийсийъ бйп дощъъфйн щчйбме ейиойп D, мбйп дощъъфйн щчйбме фмсбе бщйтеш дайшетйн дчшгйеесчемшййн баефп лммй (396 мтеоъ 409 айшетйн, бдъаод) ае бдъййзс мщйтеш дочшйн щм аеин щшйш дмб, щбх, ъоеъд овешойн чшгйеесчемшййн ае ъоеъд олм вешн.
-
дщфтеъ щмймйеъ: роцае дщфтеъ щмймйеъ оетиеъ мриймъ ейиойп D бойреп вбед, мма тмййд оебдчъ бсйлеп мдйфшчмцойд, абрйн блмйеъ ае ъсойрйн ботшлъ дтйлем.
дзечшйн ослойн, лй ъецаеъ дозчш айрп ъеолеъ бриймъ ейиойп D бойреп вбед морйтъ сшип ае ъзмеад чшгйеесчемшйъ бчшб обевшйн бшйайн ащш цешлйн ейиойп D бойреп дргшщ мщойшд тм бшйаеъ дтцн.
аеЙовд 3 (3)
-
ъзмеад чшгйеесчемшйъ: роцад йшйгд щм 8%, щайрд оебдчъ сиийсийъ, бщйтеш дайшетйн дчшгйеесчемшййн бчшб дощъъфйн щчйбме щоп гвйн бдщееад мфмсбе (386 мтеоъ 419 айшетйн, бдъаод). ъецад жаъ рбтд ойшйгд байшетйн щм аеин щшйш дмб, мма дбгм ощотеъй байшетй щбх. баефп сфцйфй, риймъ щоп гвйн дфзйъд аъ дсйлеп маеин щшйш дмб б-28%, еаъ дсйлеп мъоеъд лъецад оаеин щшйш дмб б-50%, мма дщфтд тм дсйлеп мщбх ае мъоеъд чшгйеесчемшйъ овешойн щайрн аеин щшйш дмб. тег роца лй риймъ аеовд 3 дййъд омеед бйшйгд щм 22% бцръешйн (ъдмйлй арвйефмсийд).
-
сшип: ма роца дбгм оебдч сиийсийъ, бйп дощъъфйн щчйбме щоп гвйн мбйп дощъъфйн щчйбме фмсбе бщйтеш очшй дсшип баефп лммй (820 мтеоъ 797 очшйн, бдъаод), елп бщйтеш дочшйн щм сшип щг, сшип тшоерйъ, сшип чемешчимй, ъоеъд осшип ае ъоеъд олм вешн.
-
дщфтеъ щмймйеъ: риймъ ъесу щоп гвйн рсбмд дйиб, мма тмййд бсйлеп мгйоен ае мъсойрйн ботшлъ дтйлем.
-
рйъез мфй ъъй-чбецеъ: дщфтд ойийбд, роцад бчшб ощъъфйн щгйеезе бъзймъ дозчш тм цшйлд роелд щм гвйн (тг 1.5 ореъ мщбет), тн йшйгд щм 19% бсйлеп майшетйн чшгйеесчемшййн ещм 40% бсйлеп маеин щшйш дмб, мма йъшеп оебдч мдътшбеъ бчшб ощъъфйн тн цшйлъ гвйн вбедд (отм 1.5 ореъ мщбет).
-
бресу, роцад дщфтд ойийбд мриймъ ъесу щоп гвйн, бчшб ощъъфйн ооеца афше-аошйчай, баефп бмъй ъмей бцшйлъ дгвйн.
мсйлен, ъецаеъ дозчш дтйчшйеъ ошаеъ лй риймъ ейиойп D ма ъшод мдфзъъ дсйлеп мсшип ае мъзмеад чшгйеесчемшйъ, аемн тщейд мъшен мдфзъъ дсйлеп мъоеъд осшип. риймъ аеовд 3 ма ъшод мдфзъъ дсйлеп мсшип ае мъзмеад чшгйеесчемшйъ баелмесййд длммйъ, аемн дййъд омеед бдфзъъ дсйлеп маеин щшйш дмб, елп мдфзъъ дсйлеп дчшгйеесчемшй бчшб ощъъфйн тн цшйлъ гвйн роелд.
ъецаеъ ресфеъ:
-
блрс щм айвег дмб даошйчай (AHA), щртшк бребобш 2020, децве ъецаеъ шащерйеъ орйъез ресу (VITAL-Rhythm) бе рбгчд дйтймеъ щм ейиойп D еаеовд 3 морйтъ фшфеш фшежгешйн (AF). бозчш жд, ма роцад ъойлд мщйоещ бъесфй ейиойп D ае аеовд 3 морйтъ фшфеш фшежгешйн, лащш ййълп ериймъ аеовд 3 тмемд ау мдвбйш аъ дсйлеп. йзг тн жаъ, овод жаъ ма дййъд оебдчъ сиийсийъ, еогебш бъецаеъ шащерйеъ бмбг щишн фешсое еишн тбше бйчешъ тойъйн(4).
-
брйъез ощрй щм дръерйн, рбгчд дйтймеъ щм ейиойп D мдфзъъ дсйлеп мсшип оъчгн, лъмеъ б-BMI. бъчефъ ддътшбеъ жеде 1,617 очшйн щм сшип фемщрй, лащш бчшб ощъъфйн щчйбме ейиойп D, роца сйлеп роек б-17% мсшип фемщрй бдщееад мфмсбе (щйтеш очшйн щм 1.7% мтеоъ 2.1%). дйшйгд бсйлеп дййъд оебдчъ шч бчшб дощъъфйн тн BMI биеез дрешод, ак ма бчшб ощъъфйн тн BMI отм 25 (сйлеп роек б-38% мтеоъ сйлеп роек б-11% бчшб ощъъфйн тн BMI биеез 25-30 есйлеп вбед б-5% бчшб ощъъфйн тн BMI отм 30)(5).
- http://www.vitalstudy.org/findings.html
- https://pubmed.ncbi.nlm.nih.gov/30415629/
- https://pubmed.ncbi.nlm.nih.gov/30415637/
- https://professional.heart.org/es/meetings/scientific-sessions
- https://pubmed.ncbi.nlm.nih.gov/33206192/
бозчш лфем-сойеъ обечш фмсбе (2022) рбгче дбгмйн овгшййн бдщфтд щм ейиойп D бчшб земй сшип оъчгн, бгвщ тм ъсойрй тййфеъ. боаош чегн огеезйн дзечшйн тм лк щейиойп D бойреп 4,000 йзб"м/йен мощк 12 щбетеъ дйд йтйм мдфзъъ дщйоещ бощллй лабйн еъсойрй тййфеъ бчшб земй сшип тн зсш ейиойп D. дн оцййрйн лй шоъ ейиойп D роелд дййъд чщешд бшоъ тййфеъ вбедд йеъш бчшб вбшйн ак ма бчшб рщйн, емлп бозчш жд дн обцтйн рйъезй дощк мдтшлъ ддбгмйн довгшййн бдщфтд щм оъп ейиойп D. бдъбсс тм дръерйн щм 150 ощъъфйн роца лй оъп ейиойп D дйд омеед бщйфеш оебдч бшоъ дтййфеъ бчшб вбшйн, мма дщфтд оебдчъ бчшб рщйн. ддщфтд дойийбд бчшб вбшйн дййъд бмъй ъмейд бойреп щм ощллй длабйн. осчръ дзечшйн дйа лй дщйфеш бъсойрй дтййфеъ бтчбеъ дтмаъ шоъ ейиойп D бгн дйд ощотеъй йеъш бчшб вбшйн мтеоъ рщйн.
https://pubmed.ncbi.nlm.nih.gov/35159013/
бозчш лфем-сойеъ обечш фмсбе, (2019) щртшк бйфп, рбгчд ддщфтд щм ъесу ейиойп D тм ощк ддйщшгеъ бчшб оиефмйн тн сшип бгшлй дтйлем бщмбйн 1 тг 3. бозчш рлмме 417 оиефмйн брй 66 бооецт - 10% одн тн сшип еещи, 42% тн сшип чйбд е-48% тн сшип чемешчимй. доиефмйн земче ачшайъ мриймъ ейиойп D бойреп 2,000 йзб"м/йен ае фмсбе - дзм одбйчешъ дшащерд мазш дрйъез емощк ъчефъ отчб зцйерйъ щм 3.5 щрйн. ма роцае дбгмйн оебдчйн бйп дчбецеъ бдъййзс мщйтеш дйщреъ дозмд ае ъоеъд (20% бчбецъ ддътшбеъ е-26% бчбецъ дфмсбе) ае бщйтеш ддйщшгеъ бощк 5 щрйн (82% бчбецъ ддътшбеъ е-81% бчбецъ дфмсбе). тн жаъ, ддщфтд щм дъесу дййъд оебдчъ бчшб оиефмйн тн шоеъ бсйс роелеъ щм ейиойп D (бойреп щм 20 тг 40 рревшн/о"м) тн щйтеш дйщшгеъ мма дйщреъ бощк 5 щрйн щм 85% бчбецъ ддътшбеъ мтеоъ 71% бчбецъ дфмсбе. баефп лммй, дзечшйн ослойн лй риймъ ъесу ейиойп D ма дебймд мщйфеш ощк ддйщшгеъ бчшб оиефмйн тн сшип бгшлй дтйлем.
https://www.ncbi.nlm.nih.gov/pubmed/30964526
бдъбсс тм ръерйн щм озчш лфем-сойеъ обечш фмсбе, (2018) рбгч дан ъесу ейиойп D бойреп вбед тщей мъшен мдфзъъ дсйлеп мсшип баелмесййд длммйъ. бозчш рлмме 5,110 обевшйн бвймай 50-84, ащш земче ачшайъ мриймъ ейиойп D (мма сйгп) бойреп шащерй щм 200,000 йзб"м емазш олп бойреп зегщй щм 100,000 йзб"м, ае мриймъ фмсбе. ощк ддътшбеъ рт бйп 2.5-4.2 щрйн (зцйеп щм 3.3 щрйн). бощк ъчефъ дозчш аебзре 328 очшйн щм сшип, 6.5% обйп дощъъфйн щриме ейиойп D е-6.4% обйп дощъъфйн щриме фмсбе. дзечшйн ослойн лй ма роцад ъойлд млк щриймъ ейиойп D бойреп вбед ъшод морйтъ сшип, аемн ргшщйн озчшйн ресфйн мдтшлъ ддщфтд щм риймъ ейиойп D баефп йеой ае щбетй мощк ъчефд ооещлъ йеъш.
https://www.ncbi.nlm.nih.gov/pubmed/30027269
бозчш зък (2021) рбгчд шоъ ейиойп D бчшб земй сшип, едетшк дойреп дргшщ морйтъ зсш. дзечшйн осбйшйн, лй мейиойп D ъфчйг борйтъ дъфъзеъ двйгем дооайш ебъойлд бфтймеъ ревгъ дсшип щм отшлъ дзйсеп, аемн лйен ма чййоеъ дрзйеъ мвбй оъп ъесфй ейиойп D мземй сшип. бозчш рлмме дръерйн щм 500 земй сшип ооеца мбп, одн 136 оиефмйн гйеезе тм риймд ашелъ иеез щм ъесфй ейиойп D бойрерйн щерйн. босвшъ дозчш роггд шоъ ейиойп D бгн ерасфе ръерйн чмйрййн обйъ дземйн. роца лй 66.8% одоиефмйн сбме озсш ейиойп D (фзеъ о-30 рревшн/о"м), лащш 31.6% обйп доиефмйн щгйеезе тм риймъ ъесфйн сбме озсш ейиойп D. доафййрйн щдйе чщешйн бриййд оевбшъ мзсш ейиойп D баелмесййъ дозчш дйе вйм обевш йеъш, вбшйн, абзрд щм сшип шащ ецееаш ае чшцйреоъ ъай чщчщ (SCC), ейшйгд б-BMI. бдъбсс тм дръерйн, дзечшйн отшйлйн лй дойреп дойибй морйтъ зсш ейиойп D бчшб земй сшип дйре 2,250 йзб"м/йен, ойреп вбед одойреп дргшщ маелмесййд длммйъ. дзечшйн огеезйн тм дтгш ойоеп мозчш етм дтгш рйвегй айришсйн.
https://pubmed.ncbi.nlm.nih.gov/34130032/
бозчш зък (фбшеаш 2016) бе рлмме 190 вбшйн ащш тбше рйъез млшйъъ дтшоерйъ, роца лй шод роелд щм ейиойп D чщешд бсйлеп оевбш мвйгем авшсйбй йеъш бтшоерйъ.
http://www.ncbi.nlm.nih.gov/pubmed/26903577
счйшд (ошх 2016) доцйвд аъ дооцайн бйзс мчщш бйп ейиойп D едсйлеп мселшъ емсшип дмбмб. одтгейеъ темд лй ййълп емеейиойп D ъфчйг бозмеъ дчщешеъ бмбмб, лемм селшъ сев 1 есев 2 есшип дмбмб. дъфчйг щм ейиойп D беейсеъ дфтймеъ дзйсерйъ оцбйт тм дъшеод дафщшйъ щме морйтъ селшъ сев 1. бдчщш мселшъ сев 2, дозчшйн оцбйтйн тм ддщфтд щм ейиойп D тм фтймеъ ъай бъа бмбмб, тм дшвйщеъ майрсемйп етм дъфъзеъ гмчъ отшлъйъ.оозчшйн ъцфйъййн темд чщш бйп зсш ейиойп D мбйп сйлеп оевбш мселшъ сев 1 е-2, лащш озчшйн дтесчйн бсшип дмбмб мшеб оцбйтйн тм дъшеод щм шоъ ейиойп D вбедд мщйтеш роек йеъш щм сшип мбмб елп тм чщш бйп зщйфд мщощ мбйп сйлеп роек йеъш мъзмеад еъоеъд осшип дмбмб. мошеъ ооцайн амд, ргшщйн озчшйн ачшаййн обечшйн тм оръ мбзеп баефп отойч аъ дъфчйг щм ейиойп D морйтъ озмеъ мбмб.
http://www.ncbi.nlm.nih.gov/pubmed/27030935
озчш (афшйм 2016) ащш ретг мщзжш ооцайн чегойн доцбйтйн тм лк щшод вбедд йеъш щм ейиойп D бгн чщешд бсйлеп роек йеъш мсшип. бозчш ртщд щйоещ бръерйн ощрй озчшйн дщерйн бшоъ ейиойп D дооецтъ. дозчш дшащеп дйре озчш ачшай обечш длемм 1,169 рщйн отм вйм 55 тн шоъ ейиойп D бгн щм 30 рревшн/о"м бооецт. дозчш дщрй дйре озчш течбд фшесфчийбй длемм 1,135 рщйн отм вйм 55 тн шоъ ейиойп D бгн щм 48 рревшн/о"м бооецт. дзечшйн дщее аъ щйтешй дсшип (лм севй дсшип дфемщрййн омбг сшип дтеш) бйзс мшоъ ейиойп D бъчефъ отчб щм л-4 щрйн. роца лй щйтеш дсшип дйд роек йеъш бчшб рщйн тн шйлеж ейиойп D вбед йеъш, лащш рщйн тн шоъ ейиойп D вбедд о-40 рревшн/о"м дйе бтмеъ сйлеп роек бл-67% мзмеъ бсшип бдщееад мрщйн тн шоъ ейиойп D роелд о-20 рревшн/о"м. дзечшйн ослойн лй щйфеш шоъ ейиойп D одеед лмй орйтъй зщеб аемн дн айрн оцйтйн одй дшод даефийоамйъ щм ейиойп D бгн ае лйцг оеомх мдвбйш аъ шйлеже бгн (зщйфд оевбшъ мщощ, ъжерд ае ъесфйн).
http://www.ncbi.nlm.nih.gov/pubmed/27049526
бозчш (2021) добесс тм шщеоеъ дъоеъд дмаеойеъ бвшАорйд, дтшйле дзечшйн аъ дтмейеъ еаъ дзйслеп длсфй борйтъ ъоеъд осшип баоцтеъ оъп ъесу ейиойп D млм даелмесййд отм вйм 50. дзечшйн оцййрйн лй боид-армйжеъ тглрйеъ дегвод йшйгд оебдчъ бсйлеп мъоеъд осшип бтчбеъ риймъ ъесфй ейиойп D. босвшъ дрйъез, ддтшлд щм осфш очшй дъоеъд дрйърйн морйтд зещбд тм бсйс осфш очшй дъоеъд щм обевшйн отм вйм 50 едйшйгд бсйлеп мъоеъд лфй щзещбд боид-армйжеъ чегоеъ (л-13%). дзйслеп длсфй зещб бдъан мтмеъ ийфем щм земй сшип сефрй щдетшлд бл-40,000 айше магн, едтмеъ дщръйъ щм ъесу ейиойп D магн детшлд л-25 айше магн. бдъбсс тм ръерйн амд, дзечшйн отшйлйн щоъп ъесу ейиойп D млм даелмесййд отм вйм 50 бвшАорйд цфей морет л-30,000 очшй ъоеъд тм шчт сшип блм щрд, бтмеъ ощетшъ щм л-900 оймйеп айше езйслеп щм 1.154 оймйашг айше, еблк мзйслеп рие щм 254 оймйеп айше бщрд. ъецаеъ амд ъеолеъ бтйгег риймъ ъесфй ейиойп D бчшб обевшйн морйтъ дъоеъд осшип.
https://pubmed.ncbi.nlm.nih.gov/33540476/
бгез тглрй (2017), щфешсн бощеъу тм йгй дчшп дтемойъ мзчш дсшип (AICR) едолеп даошйчай мзчш дсшип (WCRF), ослойн цееъ дзечшйн аъ дтгейеъ дозчшйеъ бревт мчщш бйп ъжерд ефтймеъ вефрйъ мбйп сшип чемешчимй.гез жд, додеед тглеп мгез щфешсн бщръ 2007, лемм 99 озчшйн (щртшле блм дтемн) - бдн л-29 оймйеп ощъъфйн ел-250,000 очшйн щм сшип чемешчимй. тм сок дооцайн щрасфе, дзечшйн ослойн лй чййоеъ тгейеъ обессеъ млк щцшйлъ гврйн омайн (лщмещ ореъ мйен), сйбйн ъжеръййн, оецшй змб (л-500 вш'/йен), риймъ ъесфй сйгп ебйцет фтймеъ вефрйъ ъешойн мдфзъъ дсйлеп мсшип чемешчимй, бтег щцшйлъ бщш аген ебщш отебг, цшйлд щм йеъш ощрй ощчаеъ амледемййн мйен, тегу ощчм, щореъ ечеод вбедд одеейн вешой сйлеп мдъфъзеъ сшип чемешчимй. бресу, дзечшйн ослойн лй чййоеъ тгейеъ осейоеъ мвешой сйлеп ресфйн, ащш чщешйн бсйлеп роек йеъш - лемм цшйлъ ожереъ тщйшйн бейиойп C, цшйлъ гвйн, ейиойп D ериймъ оемий-ейиойрйн, лащш цшйлд роелд (фзеъ о-100 вшн мйен) щм фйшеъ ейшчеъ ма тоймрййн ецшйлъ ожереъ долймйн бшжм осев дн (щочеше бзй) чщешд бсйлеп вбед йеъш мсшип чемешчимй. ма роцае тгейеъ зг-ощотйеъ бдъййзс мвешойн ъжеръййн ресфйн лвеп гврйн, ъфезй агод, щеоп одзй, теу, фйшеъ йн, дшлб зеоцеъ дщеоп, лемсишем, аеовд 3 щочешд бгвйн, чирйеъ, щен, селш оесу, чфд, ъд, фзойоеъ, тоймрйн, теос вмйчой, зеоцд фемйъ, ейиойп A, ейиойп B6, ейиойп E, смрйен, оъйерйп, биа-чшеип, мйчефп, ск дцшйлд дчмешйъ, ъгйшеъ дашезеъ ае гфес дъжерд. мдтшлъ дзечшйн л-47% оочшй дсшип дчемешчимй рйърйн морйтд баоцтеъ дчфгд тм ъжерд бшйад, бйцет фтймеъ вефрйъ ещойшд тм ощчм ъчйп.
http://www.aicr.org/continuous-update-project/colorectal-cancer.html
лзмч оозчш течбд фшесфчийбй шзб (ошх 2018), дтесч ббшйаеъ даелмесййд бйфп, бозчш дрелзй детшк дчщш бйп шоъ ейиойп D бгн мбйп дсйлеп мдъфъзеъ сшип. бозчш дрелзй рлммд ъъ-чбецд щм 3,301 земй сшип ечбецъ бйчешъ щм 4,044 ощъъфйн мма сшип оъщтд ошлжйн шфеаййн цйбешййн бйфп. дзечшйн сйееве аъ дощъъфйн машбт чбецеъ (шбтерйн), бдъан мшоъ ейиойп D, щроггд мфрй абзеп дсшип, ъек дъаод мойп емтеръ дщрд. роца лй шод вбедд йеъш щм ейиойп D бгн дййъд чщешд бсйлеп роек йеъш мсшип олм сев. баефп сфцйфй, бдщееад мощъъфйн бшбтеп дшащеп (дшод дроелд бйеъш щм ейиойп D, 36 рреоем/мйиш бооецт), дсйлеп мсшип дйд роек йеъш б-19%, б-25% еб-22% тбеш ощъъфйн бшбтеп дщрй (49 рреоем/мйиш бооецт), дщмйщй (58 рреоем/мйиш бооецт) едшбйтй (75 рроем/мйиш бооецт), бдъаод. ооцайн амд дйе бемийн бойезг тбеш сшип длбг. дзечшйн ослойн лй ъецаеъ дозчш ъеолеъ бдщтшд мфйд мейиойп D дщфтд овйрд офрй дъфъзеъ сшип осевйн щерйн.
https://www.ncbi.nlm.nih.gov/pubmed/29514781
бозчш лфем-сойеъ обечш фмсбе (ошх 2018) детшлд ддщфтд щм ъесфй сйгп еейиойп D тм дсйлеп мдъфъзеъ фемйфйн ощеррйн ишен-сширййн ботй. бозчш рлмме 2,259 ощъъфйн бвймай 45-75 о-11 ошлжйн шфеаййн башд"б, ащш тбше дсшд щм мфзеъ агреод азъ бъдмйк чемересчефйд. дощъъфйн земче ачшайъ мазъ оашбт чбецеъ щриме: ъесу сйгп бойреп 1,200 о"в/йен, ъесу ейиойп D бойреп 1,000 йзб"м/йен, щрйдн йзг ае фмсбе. мазш 3-5 щрйн щм риймъ дъесфйн (щмб ийфем), дощъъфйн дщмйое бгйчъ чемересчефйд ербзре щеб мазш 3-5 щрйн одфсчъ дъесфйн (щмб отчб). бодмк щмб дийфем, аебзре фемйфйн ощеррйн бчшб 27% одощъъфйн, щлмме фемйфйн дйфшфмсиййн бчшб 24% одощъъфйн еагреоеъ/фемйфйн ссймййн ощеррйн (SSA/Ps) бчшб 5% одощъъфйн. ма роцае дбгмйн оебдчйн бйп дчбецеъ бйзс мсйлеп мдефтъ фемйфйн ощеррйн олм сев. бодмк щмб дотчб, аебзре фемйфйн ощеррйн бчшб 30% одощъъфйн, щлмме фемйфйн дйфшфмсиййн бчшб 24% одощъъфйн е-SSA/Ps бчшб 6% одощъъфйн. бщмб дотчб роца лй дсйлеп м- SSA/Ps дйд вбед йеъш тбеш ощъъфйн щриме ъесфй сйгп бмбг (фй 2.65) ае ъесфй сйгп еейиойп D (фй 3.81). ооцайн амд оцбйтйн тм лк щриймъ ъесфй сйгп еейиойп D тмемд мдвбйш аъ дсйлеп м-SSA/Ps, лащш ддщфтд оефйтд 6-10 щрйн мазш риймъ дъесфйн.
https://www.ncbi.nlm.nih.gov/pubmed/29496722
бозчш очшд-бчшд вгем,(афшйм 2018) добесс тм ръерйн о-20 озчшй течбд, рбгч дчщш бйп шоъ ейиойп D бгн мбйп дсйлеп мдъфъзеъ сшип шйаеъ, щлп йщрн ооцайн ъцфйъййн доцбйтйн тм лк щшйлежйн вбедйн щм ейиойп D бгн тщеййн мдвп офрй сшип шйаеъ. бозчш рлмме 5,313 очшйн щм сшип шйаеъ, амйдн деъаод чбецъ бйчешъ щм 5,313 ощъъфйн бтмй оафййрйн геойн. бгйчеъ дгн щм дощъъфйн земй дсшип рмчзе лзощ щрйн бооецт мфрй абзеп дозмд. дзечшйн ма оцае чщш оебдч бйп шоъ ейиойп D бгн мбйп дсйлеп мдъфъзеъ сшип шйаеъ, вн лащш рбгчд ддщфтд щм вешойн ресфйн лое вйм, ойп, тйщеп есев дсшип.
https://www.ncbi.nlm.nih.gov/pubmed/29617726
брйъез лемм щм ръерйн о-17 озчшй течбд (йерй 2018) рбгч баефп шишесфчийбй дчщш бйп шйлеж шоъ ейиойп D бгн мбйп дсйлеп мсшип чемешчимй. бозчш рлмме дръерйн щм 5,706 ощъъфйн, щаебзре тн сшип чемешчимй, ечбецъ дщееад щм 7,107 ощъъфйн бшйайн. роца лй бдщееад мшоеъ ейиойп D щм 50-62.5 рреоем/мйиш, щдйре диеез дъзъеп досфйч мщойшд тм бшйаеъ дтцн, ощъъфйн тн зсш ейиойп D (фзеъ о-30 рреоем/мйиш) дйе бсйлеп вбед б-31% мсшип чемешчимй еайме ощъъфйн тн шоеъ вбедеъ йеъш щм 75-87.5 ещм 87.5-100 рреоем/мйиш дйе бсйлеп роек б-19% еб-27%, бдъаод. ма роца йъшеп мшоеъ двбедеъ о-100 рреоем/мйиш. ъецаеъ амд ма дещфте баефп ощотеъй од-BMI, фтймеъ вефрйъ ае вешой сйлеп азшйн. ръерйн амд обиайн сйлеп роек йеъш б-19% мрщйн е-7% мвбшйн тбеш лм тмййд щм 25 рреоем/мйиш бшйлеж ейиойп D бгн. дзечшйн ослойн лй шоеъ вбедеъ йеъш щм ейиойп D бгн дйе чщешеъ бсйлеп роек йеъш мсшип чемешчимй, бойезг бчшб рщйн. ръерйн амд оцбйтйн тм лк щдшйлеж даефийоамй дйре 75-100 рреоем/мйиш, шйлеж щдйре вбед йеъш оддомцеъ дрелзйеъ щм д-(IOM (Institute of Medicine.
https://www.ncbi.nlm.nih.gov/pubmed/29912394
зжшд мъзймъ дозчшйн
зеМоцд феЙмйъ
оид-армйжд зщебд щбецтд баесишмйд (фбшеаш 2014) тесчъ бчщш бйп цшйлъ зеоцд фемйъ мбйп дсйлеп мсевй сшип щерйн бгшлй дтйлем дтмйереъ – сшип дещи, сшип дчйбд есшип дмбмб. 9 озчшйн шишесфчийбййн дтесчйн бчщш бйп зеоцд фемйъ есшип дещи дшае лй цшйлд щм зеоцд фемйъ бъжерд дбйад мйшйгд щм л-40% бсшип дещи. рйъез дооцайн щм 16 дозчшйн дтесчйн бсшип дчйбд ма дшад чщш оебдч мзеоцд фемйъ. 8 озчшйн дшае йшйгд щм л-34% бсйлеп мсшип дмбмб бдчщш мцшйлъ зеоцд фемйъ. дзечшйн ослойн лй дооцайн осфчйн ъойлд шащерйъ мчщш бйп цшйлъ зеоцд фемйъ мбйп дсйлеп мсшип дещи едмбмб ан лй чййн чещй мфшщ ооцайн амд маеш ддишеврйеъ двбедд щм дозчшйн дщерйн. млп мгтъре ргшщйн озчшйн чмйрййн айлеъййн тм оръ мдощйк емзчеш чщшйн амд емдвгйш домцеъ ййщеойеъ маелмесййд дшзбд бйзс мцшйлъ зеоцд фемйъ.
http://www.ncbi.nlm.nih.gov/pubmed/24224911
счйшд (фбшеаш 2016) доцйвд аъ дтгейеъ дтглрйеъ бревт мчщш бйп шоъ дзеоцд дфемйъ бгн мбйп озмеъ щереъ. шащйъ оецвъ счйшд шзбд мвбй ддшлб, дочешеъ, дфтймеъ доибемйъ едъфчйг щм зеоцд фемйъ. бдощк оецвеъ дтгейеъ мвбй зеоцд фемйъ бдчщш моцбйн шфеаййн щерйн, лемм шоеъ вбедеъ щм деоецйсиайп, озмъ мб лмймйъ, йъш мзх гн, щбх, селшъ, дшйеп, сшип (баефп сфцйфй сшип тшоерйъ, сшип чемешчимй, сшип мбмб, сшип щг, мейчойд бймгйн есшип шйаеъ) озмеъ лмйд, озмеъ рейшемевйеъ еасъод бймгйн. дзечшйн ослойн лй йщрп тгейеъ шбеъ дъеолеъ бъфчйг щм зеоцд фемйъ бчйген бшйаеъ елп бфеирцйам морйтд еийфем бозмеъ. йщрд ъойлд шзбд мйтймеъ щм риймъ ъесфй зеоцд фемйъ ишн длрйсд мдшйеп морйтъ оеойн бътмд дтцбйъ (NTD). тн жаъ, дооцайн мвбй дчщш бйп зеоцд фемйъ мбйп оцбйн шфеаййн азшйн айрн зг-ощотййн ергшщйн озчшйн чмйрййн ресфйн тм оръ мдтшйк аъ дъшеод дчмйрйъ щм риймъ ъесфй зеоцд фемйъ.
http://www.ncbi.nlm.nih.gov/pubmed/27008500
бсчйшд (йерй 2017) оцйвйн дзечшйн аъ дтгейеъ бревт мчщш бйп цшйлъ зеоцд фемйъ мбйп дсйлеп ммечойд бвйм дймгеъ. одсчйшд темд лй мзеоцд фемйъ дщфтд тм доитп дврий еъфчйг борйтъ сшип едъчгоеъе - бтйчш бщм дщфМтъд тм ъдмйк доъймцйд щм д-DNA, ъдмйк зщеб ббчшд еъйчеп д-DNA. дщфтеъ аме зщебеъ бойезг бодмк ддшйеп, щлп мъжеръ дан ъфчйг ошлжй бдъфъзеъ дтебш ебриййд мъзмеад бдощк дзййн. йщрн ооцайн дошайн лй зсш бзеоцд фемйъ тщей мдщфйт тм ъдмйлй доъймцйд щм врйн осейойн еблк мдвбйш ъдмйлйн фъеврййн есширййн. бресу, дбгмйн вриййн чййойн тмемйн мдщфйт тм доибемйжн щм зеоцд фемйъ еблк мдщфйт тм дсйлеп мсшип, лемм мечойд бчшб ймгйн. тн жаъ, ддщфтд ллм дршад ъмейъ ойреп, лк щвн мтегу зеоцд фемйъ дщфтеъ щмймйеъ. дойреп дйеой доеомх деа 400 оч"в мобевшйн, 600 оч"в бдшйеп е-500 оч"в бдрчд.баефп лммй роца лй риймъ ъесу зеоцд фемйъ мфрй ебодмк ддшйеп тщейд мдееъ вешн овп офрй дъфъзеъ мечойд, аемн йщ мдощйк ембзеп оде дойреп даефийоамй, бойезг лащш ощемб тн ъесфйн ресфйн.
https://www.ncbi.nlm.nih.gov/pubmed/28588742
лзмч оозчш течбд (аевеси 2017), щретг мбзеп аъ дчщш бйп ейиойрйн есшип (VITAL), бозчш дрелзй рбгч дчщш бйп риймд ооещлъ щм ейиойрй B мбйп дсйлеп мсшип шйаеъ. бозчш рлмме 77,118 ощъъфйн бвймай 50-76, одн 808 аебзре тн сшип шйаеъ. дзечшйн бгче аъ дсйлеп мсшип шйаеъ бйзс мойреп дйеой дооецт щм ейиойрйн еоемий-ейиойрйн биеез щм 10 щрйн. бчшб рщйн ма роца чщш бйп риймъ ейиойрй B (зеоцд фемйъ, B6 е-B12) мбйп дсйлеп мсшип шйаеъ. тн жаъ, бчшб вбшйн роца лй риймъ ъесфй ейиойп B6 е-B12 (лъесу рфшг ема лзмч ооемий-ейиойп) дййъд чщешд бтмййд щм 30-40% бсйлеп мсшип шйаеъ. баефп сфцйфй, бдщееад мвбшйн щма риме ъесфйн амд, цшйлд вбедд маешк жоп щм ейиойп B6 (отм 20 о"в/йен) ещм ейиойп B12 (отм 55 оч"в/йен) дййъд чщешд бсйлеп лфем мдъфъзеъ сшип шйаеъ. шоъ дсйлеп дййъд вбедд йеъш тбеш вбшйн отщрйн. тег оцййрйн дзечшйн лй чщшйн амд роцае тбеш лм севй сшип дшйаеъ омбг сшип осев агречшцйреод, дчщеш бойгд дроелд бйеъш мтйщеп.
https://www.ncbi.nlm.nih.gov/pubmed/28829668
зжшд мъзймъ дозчшйн
смрйеМн
бсчйшд щйиъйъ (2024) детшле дооцайн оозчшйн ачшаййн обечшйн мвбй ддщфтд щм смрйен лийфем ощмйн бчшб земй сшип. бсчйшд рлмме 12 озчшйн бдн сд"л 2,483 земй сшип, лемм мйофеод щайрд дегвЧчйп, сшип шащ ецееаш, сшип бмеиъ дъшйс, мечойд, сшип шйаеъ, сшип щг, сшип цееаш дшзн есшип шзн, сшип тшоерйъ есшип щмфезйъ дщъп. бозчшйн амд рбгчд ддщфтд щм ъесфй смрйен осевйн щерйн биеез ойрерйн щм 200 тг 800 оч"в мйен.
ощк ддътшбеъ рт бйп 10 йойн м-5 щрйн. доггйн щдетшле дйе овеерйн елмме щйрей бшоъ PSA, штймеъ тм шчт ийфемй чшйрд, щйтеш дйщшгеъ, жоп тг мдйщреъ еайлеъ зййн. одъецаеъ темд лй бдъййзс мштймеъ тм шчт ийфемй чшйрд, мъйсеу смрйен дййъд дщфтд ойийбд шч бчшб оиефмйн щсбме озсш смрйен, мма йъшеп бчшб оиефмйн тн шоъ смрйен осфчъ. баефп бмъй ъмей бшоъ дсмрйен дбсйсйъ, ма роца йъшеп оебдч мриймъ ъесфй смрйен бдщееад мчбецъ дбйчешъ бдъййзс моггйн дресфйн щрбгче. дзечшйн ослойн лй бщм дишеврйеъ вгемд бйп дозчшйн еовбмеъ оъегемевйеъ, ма рйъп мдсйч баефп зг ощотй мвбй дйтймеъ щм ъесфй смрйен бчшб земй сшип. тн жаъ, рйлш лй моиефмйн тн зсш овржйен тщейд мдйеъ ъетмъ мъйсеу смрйен бодмк ийфемй чшйрд.
https://pubmed.ncbi.nlm.nih.gov/39374898/
бсчйшд (2021) грйн дзечшйн бтгейеъ дозчшйеъ дтесчеъ бъфчйг щм смрйен ббшйаеъ ебдъфъзеъ ъзмеад лшерйъ. бсчйшд офешийн дочешеъ дъжеръййн щм смрйен, лащш дшйлеж двгем бйеъш роца, бсгш йешг, божереъ щочешн одзй (бщш, гвйн, змб ебйцйн), йшчеъ (бтйчш оощфзъ доцмйбйн, щен ебцм), гврйн ефйшеъ, лъмеъ бшйлеж дсмрйен бчшчт. авежй бшжйм дн дожеп бе шйлеж дсмрйен дйре двбед бйеъш. бдощк, дзечшйн грйн басишивйеъ щм дтщшъ дожеп, бщйиеъ догйгд еддтшлд, ебоибемйжн едфтймеъ дбйемевйъ щм смрйен. бзмчд дщрй щм дсчйшд оецвйн дооцайн бдъййзс мъфчйг дсмрйен бозмеъ лшерйеъ, лемм озмеъ чшгйеесчемшйъ, селшъ, озмеъ щм бмеиъ дъшйс, гмчъ ачеийъ елшерйъ, сшип ебтйеъ фешйеъ. дзечшйн осййойн бфйшеи тшлй дййзес дъжеръййн (DRI). дн оцййрйн лй чййн иеез цш йзсйъ бйп зсш смрйен ештймеъ, лащш ддомцд дйа тм цшйлд ойрйомйъ щм 40 оч"в/йен, щлп бцшйлд роелд о-11 оч"в/йен оефйтйн ъсойрйн бшешйн лвеп фвйтд зйсерйъ, жйдеойн рвйфййн едфштд бфешйеъ. шод щм 100-200 оч"в/йен ргшщъ мцоцен ржчйн вриййн едъчгоеъ щм ооайшейеъ ббрй агн. штймеъ оефйтд бцшйлд щм 900 оч"в/йен елеммъ ъсойрйн лвеп айбег дбшч бщйтш ебцйфешрййн, дфштеъ ботшлъ дтйлем, дфштеъ тешйеъ, дфштеъ ботшлъ дтцбйн етег.
дзечшйн ослойн лй чййоеъ тгейеъ бшешеъ мдщфтд довйрд щм смрйен бдчщш мъзмеад чшгйеесчемшйъ, селшъ, сшип осевйн щерйн, озмеъ гмчъйеъ, жйден рвйфййн ефешйеъ, тн чщш бцешъ U бйп шоъ дсмрйен еддщфтд дбшйаеъйъ. мфйлк, мъйсеу смрйен тщейд мдйеъ ъетмъ маелмесййд тн шоъ бсйс роелд ак дщфтд ожйчд баелмесййд тн шоъ бсйс ъчйрд.
https://pubmed.ncbi.nlm.nih.gov/34065478/
озчш очшд-бчшд добесс тм озчш течбд (йерй 2016) айшефай вгем, оцбйт тм лк щшоеъ смрйен роелеъ тмемеъ мдйеъ чщешеъ бсйлеп оевбш мдъфъзеъ сшип длбг.
http://www.ncbi.nlm.nih.gov/pubmed/27357089
бозчш очшд-бчшд, (2019) ащш обесс тм ръерйн оозчш ачшай обечш вгем, щртшк бсйп, рлмме 229 ощъъфйн тн абзрд згщд щм сшип, амйдн деъаод чбецъ бйчешъ щм 229 ощъъфйн мма сшип. роца лй:
- шод вбедд йеъш бгн щм ейиойп E дййъд чщешд бсйлеп оефзъ мсшип ботшлъ дтйлем.
- шоъ ейиойп E вбедд дййъд чщешд бсйлеп оефзъ мсшип баефп лммй бчшб ощъъфйн тн шоъ смрйен вбедд, ак бсйлеп оевбш мсшип бчшб ощъъфйн тн шоъ смрйен роелд.
https://www.ncbi.nlm.nih.gov/pubmed/30713028
бозчш чмйрй ачшай (гцобш 2016) рбгчд ддщфтд щм цшйлъ смрйен бъжерд ещм ойцей ъд йшеч - бощемб ае брфшг - тм сорйн бйемевййн дчщешйн мсшип чемешчимй. дзечшйн оцййрйн лй йщрп тгейеъ оозчшйн афйгойемевййн, ъцфйъййн ефшд-чмйрййн, доцбйтеъ тм чщш щмймй бйп смрйен еъд йшеч мбйп дсйлеп мсшип чемешчимй, аемн дооцайн мвбй орврерй дфтемд дйрн оевбмйн.
бозчш рлмме 32 оъргбйн отм вйм 50 тн шоеъ смрйен роелеъ (Se≤1.36 µmol/l), ащш земче ачшайъ м-3 чбецеъ дозчш щриме мощк 6 щбетеъ:
- щйщд авежй бшжйм лочеш мсмрйен (л-48 оч"в/йен).
- ашбт лоесеъ щм ойцей ъд йшеч (800 о"в/йен EGCG).
- щйщд авежй бшжйм + ашбт лоесеъ щм ойцей ъд йшеч.
одъецаеъ темд лй риймъ смрйен е/ае ойцей ъд йшеч дййъд омеед беейсеъ сорйн бйемевййн дчщешйн мдъфъзеъ сшип чемешчимй, ебаефп сфцйфй щм смре-змберйн (SePP), щм осмемй ъчщешъ ъайъ (β-catenin), щм ъдмйлйн гмчъййн (NF-κB) еъдмйлй оъймцйд (DNMT1). ма роцад дщфтд вгемд йеъш мриймъ щрй дъесфйн бощемб мтеоъ ддщфтд щм лм ъесу брфшг.
https://www.ncbi.nlm.nih.gov/pubmed/27923410
бсчйшд (аечиебш 2017) оецвеъ дтгейеъ дтглрйеъ бдъййзс мъшеод щм аешз зййн бшйа морйтъ сшип дтшоерйъ, ъек жйдей лйеерй озчш тъйгййн. одсчйшд темд лй йщрн озчшйн фшд-чмйрййн еъцфйъййн дошайн лй мвешой аешз зййн щерйн, лемм ъжерд ефтймеъ вефрйъ, тщей мдйеъ ъфчйг бдаиъ дъчгоеъ дозмд, бцоцен щйтеш дъоеъд ебдфзъъ рим дозмд баефп лммй, бчшб земй сшип тшоерйъ боцб оъчгн. баефп сфцйфй, цшйлд вбедд щм йшчеъ ефйшеъ, дфзъъ дцшйлд щм бщш аген ещеоп шеей едвбшъ дфтймеъ двефрйъ роцае чщешйн бсйлеп роек йеъш мдъфъзеъ сшип дтшоерйъ, мтцйшъ дъчгоеъ дозмд емтмййд бщйтеш ддйщшгеъ.
бозчшйн ачшаййн обечшйн роца лй ъесфй смрйен еейиойп C ма дйе йтймйн морйтъ дъфъзеъ сшип дтшоерйъ, елй ъесфй ейиойп E тмемйн ау мдвбйш аъ дсйлеп. дзечшйн оцййрйн лй лйен ртшк озчш вгем, дбезп аъ ддщфтд щм ъжерд тщйшд бйшчеъ бчшб земй сшип дтшоерйъ, еозчш ресу, дбезп аъ ддщфтд щм фтймеъ вефрйъ бчшб земйн тн сшип тшоерйъ вшешъй. дзечшйн ослойн лй чййоъ ъойлд мъшеод щм аешз зййн бшйа морйтъ сшип дтшоерйъ, аемн ргшщйн озчшйн ачшаййн обечшйн тм оръ мдтшйк аъ дйтймеъ дчмйрйъ щм вешойн амд.
https://www.ncbi.nlm.nih.gov/pubmed/29049045
зжшд мъзймъ дозчшйн


 олймйн
олймйн  (Salvia hispanica) лу щм жштй ц'йд олймд л-2.5 вшн зеоцд амфа мйремайъ, 5 вшн сйбйн ъжеръййн, 2 вшн змбеп, ойршмйн лвеп
(Salvia hispanica) лу щм жштй ц'йд олймд л-2.5 вшн зеоцд амфа мйремайъ, 5 вшн сйбйн ъжеръййн, 2 вшн змбеп, ойршмйн лвеп